By the autumn of 2020, U.S. physicians grew concerned that patients who were avoiding visits to doctor’s offices were missing care for chronic conditions, discussed in in Delayed and Forgone Health Care for Nonelderly Adults during the COVID-19 Pandemic from the Urban Institute. More than three-fourths of people who delayed or forewent care had at least one chronic health condition.
 The pandemic may have led to excess deaths from diabetes, dementia, hypertension, heart disease, and stroke, as well as record drug overdoses in the 12 months ending in May 2020.
The pandemic may have led to excess deaths from diabetes, dementia, hypertension, heart disease, and stroke, as well as record drug overdoses in the 12 months ending in May 2020.
In their JAMA editorial on these data, Dr. Bauchner and Dr. Fontanarosa call “these deaths [reflect] a true measure of the human cost of the Great Pandemic of 2020.”
The Urban Institute recommends from the start of this paper that these deaths underscore the importance of assuring people with chronic physical and behavioral conditions be able to access necessary care during and beyond the public health crisis.
The researchers studied data from the Coronavirus Tracking Survey of nonelderly U.S. adults ages 18-64 as of September 11 through 28, 2020.
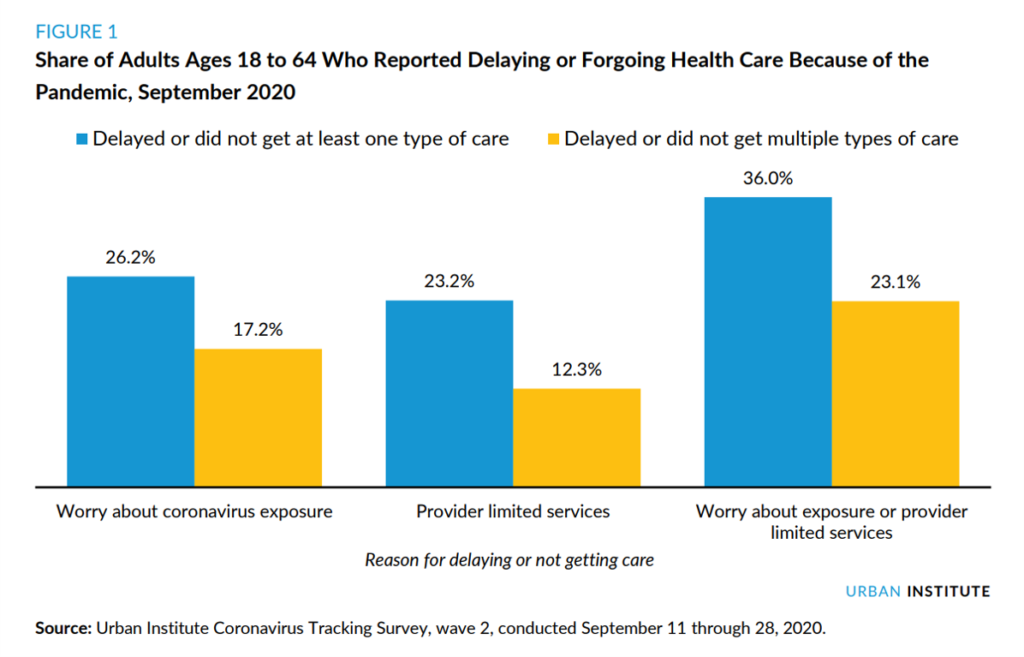
Over one-third of working-age Americans were delaying or forgoing care did so because their providers limited services or they were worried about exposure to the coronavirus, shown in the first chart.
Black adults were more likely than Whites to have delayed or forgone care. People with lower-incomes were also more likely to delay or not get health care.
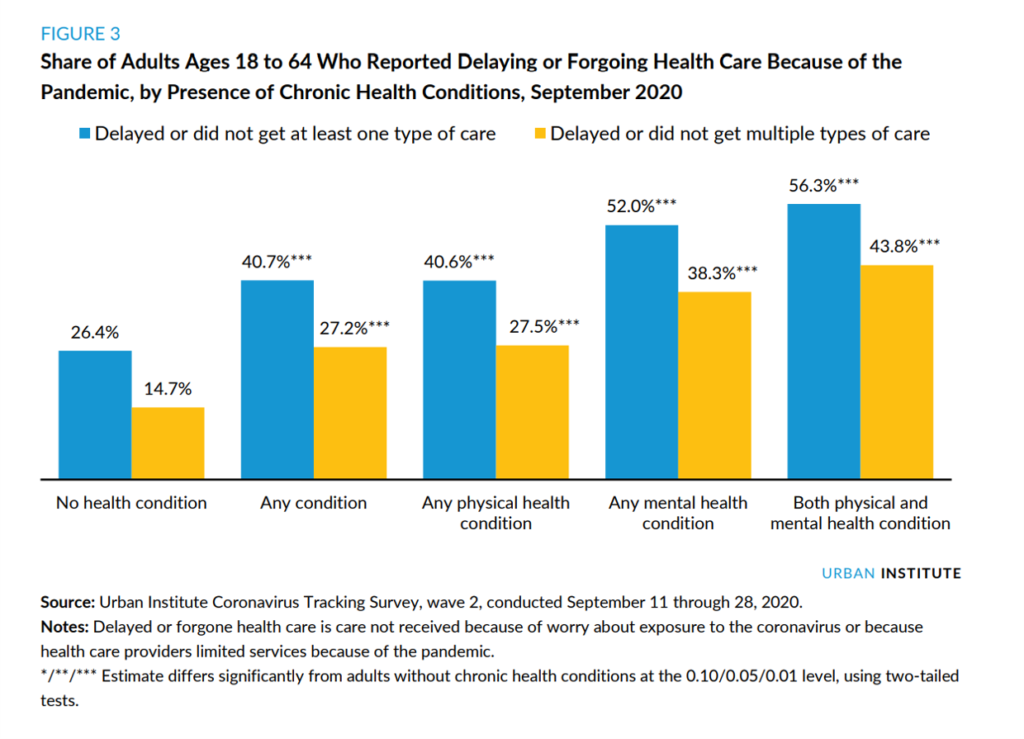 Four in 10 working aged Americans with at least one chronic condition (either physical or mental/behavioral) delayed or postponed care, compared with 26% (1 in 4) of people without a condition who delayed care.
Four in 10 working aged Americans with at least one chronic condition (either physical or mental/behavioral) delayed or postponed care, compared with 26% (1 in 4) of people without a condition who delayed care.
Even more people dealing with a mental/behavioral health issue delayed/forewent care: 52% of people with any mental health condition skipped care, versus 40% of people with any physical health condition.
Patients dealing with both physical and mental health conditions were even more likely to skip care: 56% of folks managing both a physical and mental issue delayed/forewent care.
People who skipped care were most likely to avoid dental care (25%), visit to a GP or specialist (21%), preventive health screening or medical test (16%), treatment or follow-up care (12%), or a hospital visit (10%).
About one in four people who avoided care reported that their chronic health condition worsened.
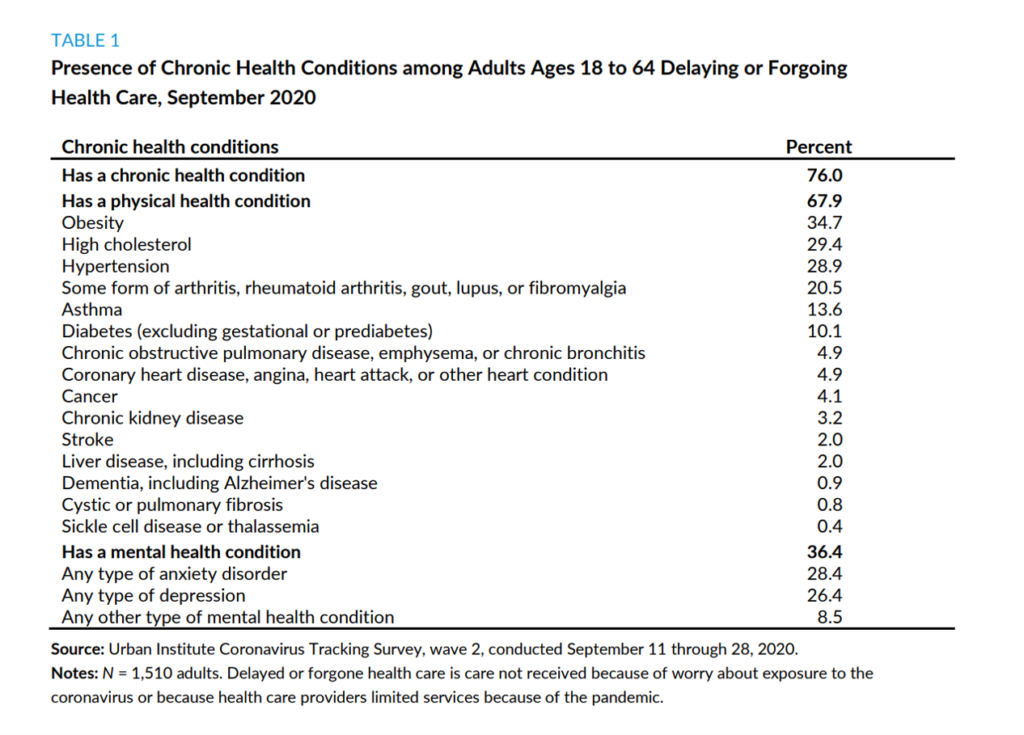 Health Populi’s Hot Points: Looking at the top ten chronic conditions diagnosed in people who avoided health care, we see the most common were obesity and diabetes (metabolic syndrome), heart disease risks (cholesterol, hypertension) along with arthritis and respiratory conditions (asthma, COPD). Many of these conditions also place people at higher risk of complications due to the coronavirus.
Health Populi’s Hot Points: Looking at the top ten chronic conditions diagnosed in people who avoided health care, we see the most common were obesity and diabetes (metabolic syndrome), heart disease risks (cholesterol, hypertension) along with arthritis and respiratory conditions (asthma, COPD). Many of these conditions also place people at higher risk of complications due to the coronavirus.
One-in-three people forgoing health care also had a diagnosed mental health condition — roughly equal proportions of anxiety disorder and depression.
The Urban Institute recommends that providers assure patients of the safety precautions institutions have taken since the start of the pandemic, as well as outreach to populations who have more likely avoided care. Medicaid programs, too, could develop targeted outreach and case management to ensure people who need care get care on a timely basis.
The Urban Institute also promotes the use of telehealth especially for chronic disease management and follow-up visits.
Concluding the report, Urban Institute recognizes that while this study did not focus on cost, personal health care finances can be a barrier for the very people this study identifies at-risk for delaying and forgoing needed care.
“The pandemic has led to widespread negative economic impacts, and many of those most affected by the recession have also delayed or forgone care because of cost of COVID-19 concerns,” previous Urban Institute research found. Health insurance coverage will be necessary, but not sufficient, the report asserts. Social determinants such as low incomes, financial instability, language and cultural barriers underpin health disparities and inequities.




 Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a