Two studies published in May 2021 illustrate the value and importance of telehealth to patients in 2020, and a disconnect among many C-level executives working in hospitals, academic medical centers, and other care provider organizations. Together, the two reports from J.D. Power and BDO illustrate some mis-alignment between the demand and supply side of telehealth.
 On the consumer demand side, patients’ growing use of telehealth in the COVID-19 pandemic along with more frequent digital contacts with health plans bolstered member satisfaction, discovered by the J.D. Power 2021 U.S. Commercial Member Health Plan Study.
On the consumer demand side, patients’ growing use of telehealth in the COVID-19 pandemic along with more frequent digital contacts with health plans bolstered member satisfaction, discovered by the J.D. Power 2021 U.S. Commercial Member Health Plan Study.
J.D. Power has conducted the U.S. Commercial Member Plan Study for the past 15 years. exploring consumer satisfaction with some 150 health insurance plans operating in 22 regions around the U.S. This year, J.D. Power assessed the opinions of 32,066 commercial health plan members between January and March 2021.
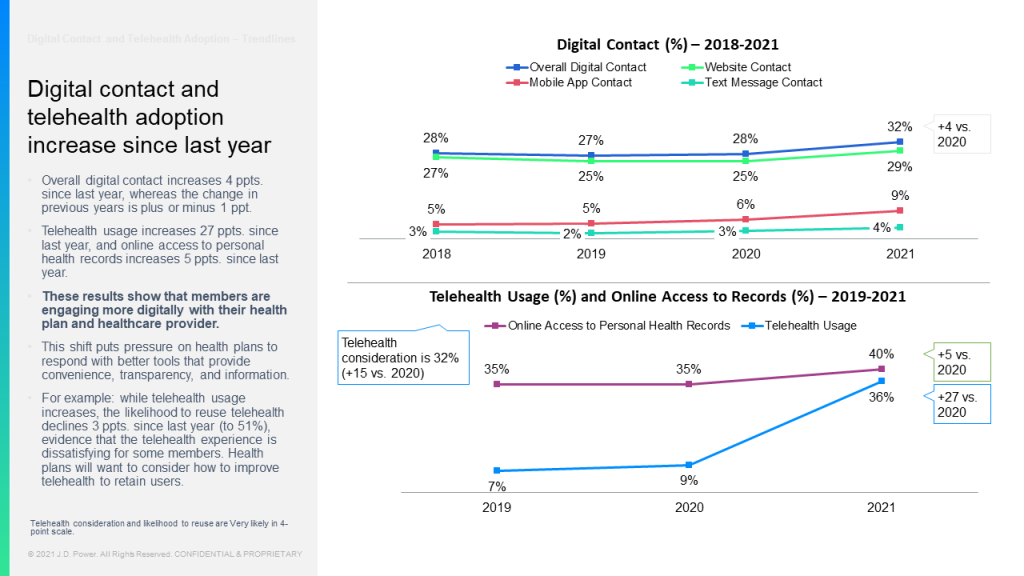
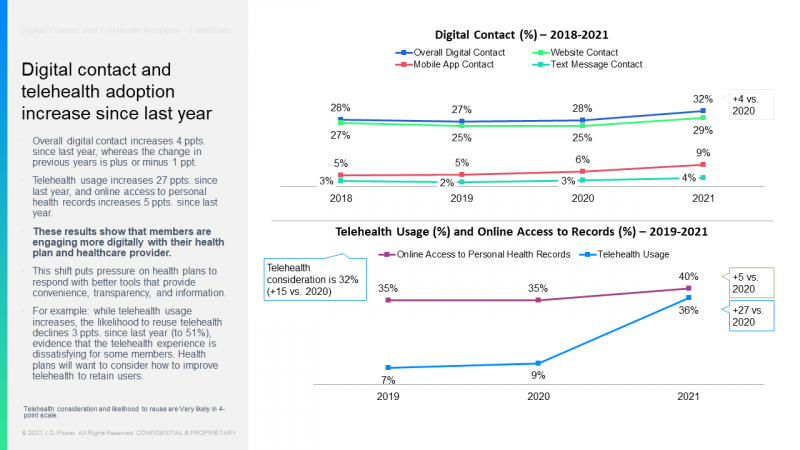
Across all health plans in the study, commercial plan members’ use of telehealth grew to 36%, an increase from 9% last year, as the lower portion of the first chart from the report shows: that’s the blue line illustrating “hockey stick”-like growth from 2020 to 2021.
With more digital contact as well, J.D. Power asserts that, “this shift puts pressure on health plans to respond with better tools that provide convenience, transparency, and information.”
Across all plans, consumers’ Net Promoter Scores (NPS) have increased year over year since 2019 when they hit a low of 11, now up 7 points in 2021 to 18. Consumers’ satisfaction with both health plan websites and information and communication.
On the supply side, BDO surveyed 100 C-level leaders across the health care provider landscape in January 2021 to assess the executives’ views on digital health technology infrastructure and tools nearly one year into the pandemic.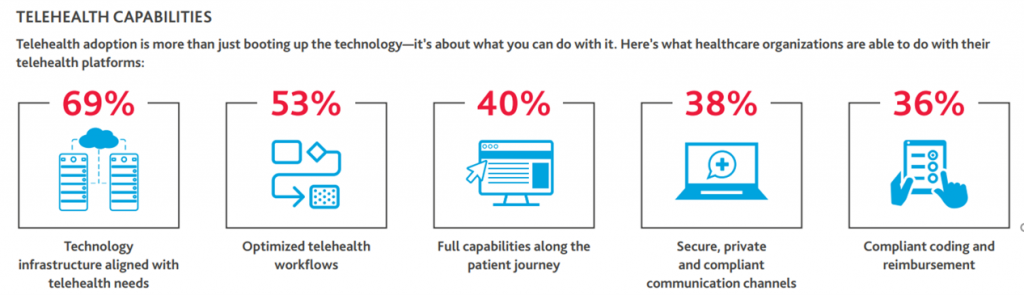
As a result of the COVID-19 pandemic, 60% of providers told BDO they are adding new digital projects in 2021.
Check out what providers have been doing with their telehealth platforms, shown in the chart. Two-thirds of providers are working to align their technology infrastructures with telehealth needs, and one-half believe they have optimized telehealth workflows.
 Another 2 in 5 say they are leveraging the full capabilities of virtual care along the patient journey, as well as ensure security, privacy and compliance in their communication channels.
Another 2 in 5 say they are leveraging the full capabilities of virtual care along the patient journey, as well as ensure security, privacy and compliance in their communication channels.
Telemedicine is, in fact, the top area where health care organizations are investing to improve the patient care experience: 75% of providers are investing in telemedicine to improve patient care in 2021 compared with 42% in 2019.
The “digital front door” has become increasingly important to health care organizations, as well, with 63% of providers enabling patients to make appointments through their portal, and 61% providing online bill payment.
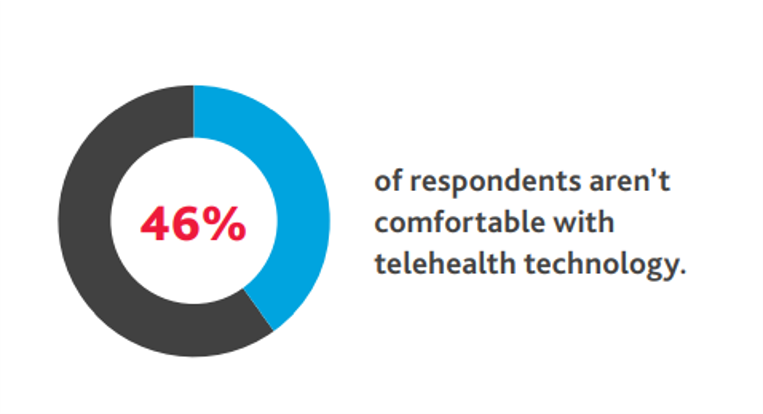
Even with these bullish investments toward virtual care to enhance the patient experience, 46% of health care providers said that they were “not comfortable” with telehealth technology as of January 2021.
Health Populi’s Hot Points: June 2021 is an auspicious month: first, it’s Pride Month! And second, the month features four weeks of sessions for the annual ATA Conference which kicked off last week on Tuesday 1stJune followed by more sessions on Thursday the 3rd. The ATA proceedings will continue Tuesday’s and Thursday’s for the remainder of June, concluding on Tuesday the 29th.
As Dr. Joe Kvedar, ATA Board Chair, noted at the conference kick-off, “During the pandemic, for the first time in history, patients experienced the convenience of having the doctor’s office brought into their home, and by all counts they loved it.”
He then noted that on the supply side, there is a “strong magnetic force” that compels health care providers to return to the norm of face-to-face, brick-and-mortar care.
Still, Kvedar acknowledged the “strong magnetic force” pulling the provider industry back toward brick-and-mortar care. “We have fixed assets…[but] there may be a time in the future where they become liabilities,” Dr. Kvedar warned.
To that point, I’ll note that my ATA 2021 session is scheduled for 15th June on MeCare: the engaged consumer changing the journey of health and care. I’ll be hosted by Karsten Russell-Wood who leads Philips’ portfolio for Post Acute & Home health care. Our session speaks to both the consumer demand for and value of virtual care and especially care delivered at home, including the scenario for some providers to not yet be aligned to that “MeCare” vision as we see through the J.D. Power and BDO research – that “magnetic force” health care is well-known for — fee-for-service, volume-based care.
One counter-force that would motivate providers to adopt virtual care as normal “healthcare” flow is value-based care. Importantly, Liz Fowler, the Director of the Center for Medicare and Medicaid Innovation (CMMI), spoke at a Health Affairs event on 3rd June and said that CMMI will look to focus more value-based models on the patient rather than the provider – to ensure that every member in a public health plan has a relationship with a physician, a health system, an accountable care organization, or other group taking on financial risk that accounts for the total cost of care.
Doing so could result in more regular and natural use of telehealth and virtual care that is incentivized by the value-based payment regime.




 Thank you FeedSpot for
Thank you FeedSpot for