The COVID-19 pandemic digitally transformed most people living in the U.S., re-shaping consumers to work from home when possible, go to school there, and buy all manners of goods and services via ecommerce.
 In March 2021, Zoom conducted research into the question, “how virtual do we want our future to be?” posing that to thousands of citizens living in 10 countries including the U.S.
In March 2021, Zoom conducted research into the question, “how virtual do we want our future to be?” posing that to thousands of citizens living in 10 countries including the U.S.
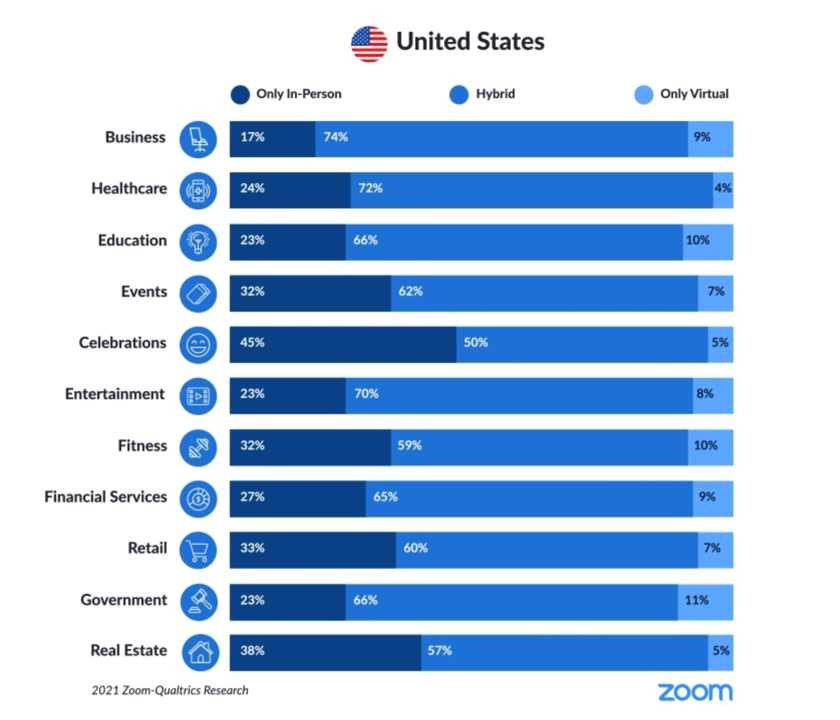
As the first chart from the study illustrates, most people in America expect hybrid lifestyles, from fitness and retail to entertainment and education.
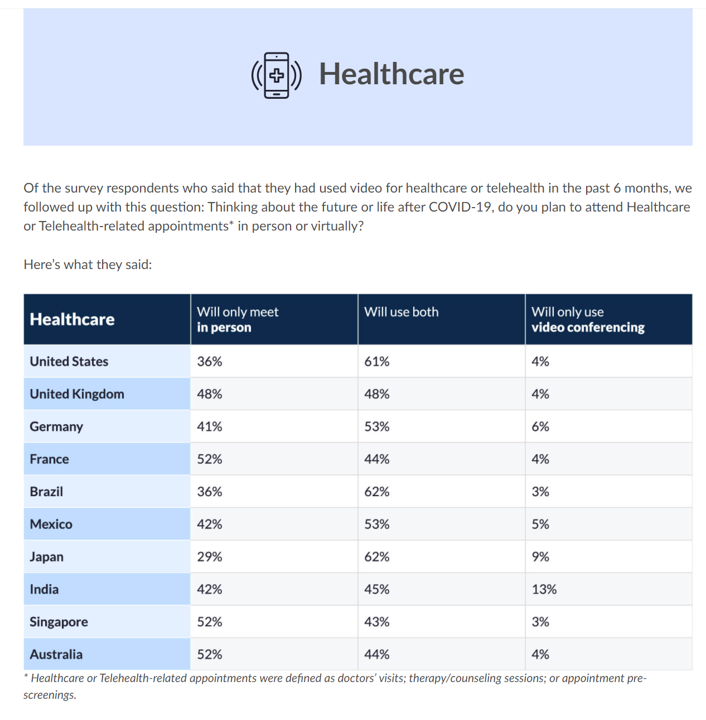
And 7 in 10 U.S. health citizens want their health care to be hybrid, too.
That means both virtual and in-person, or in the current parlance, “omni-channel.”
This week at the annual HIMSS Conference (being held in hybrid mode, BTW), Zoom announced its new program expanding virtual care to people via texts and email messages.
Zoom developed a new iOS mobile browser client on the Zoom for Healthcare platform, enabling people to connect for appointments with health care providers via Apple devices. This is designed to take out friction of having to download an app, allowing the patient to simply open up an email or text that contains a Zoom meeting link from the provider. This is in beta, and Zoom plans to roll the capability out to other operating systems.
I welcomed the opportunity to speak (via Zoom, of course) with Ron Emerson, Zoom’s Global Healthcare Lead, just a days before HIMSS 2021 kicked off.
 In preparing for our virtual meeting, I found that Ron had been trained as a nurse, and was a young pioneer working with the Maine telemedicine network 25 years ago.
In preparing for our virtual meeting, I found that Ron had been trained as a nurse, and was a young pioneer working with the Maine telemedicine network 25 years ago.
Ron cited three early learnings that he’s applying now in this bullish telehealth era:
- The experience of both patients and clinicians are key to building adoption and use of virtual care, respecting patient and clinician satisfaction;
- Clinical efficacy and how well care can be done from a distance; and,
- Cost-effectiveness and sustainability.
“At Zoom, we’ve developed trust in all 3 areas,” Ron told me, pointing to Zoom’s ease of use and dependability, experience in working in lower bandwidth environments, and integration with EHRs like Epic with a growing portfolio of use cases.
Zoom had already been a telehealth partner to many healthcare systems and organizations before COVID-19. They had developed business associate agreements (BAAs) for HIPAA compliance over four years ago, thousands of which had been in place across the U.S. prior to the pandemic — from Federally Qualified Health Clinics to some of the largest tertiary centers of excellence in the world, Ron explained.
Of course, the pandemic drove up telehealth traffic on Zoom simultaneous to mainstream consumers adopting Zoom as both a noun and a verb as in, “to Zoom.”
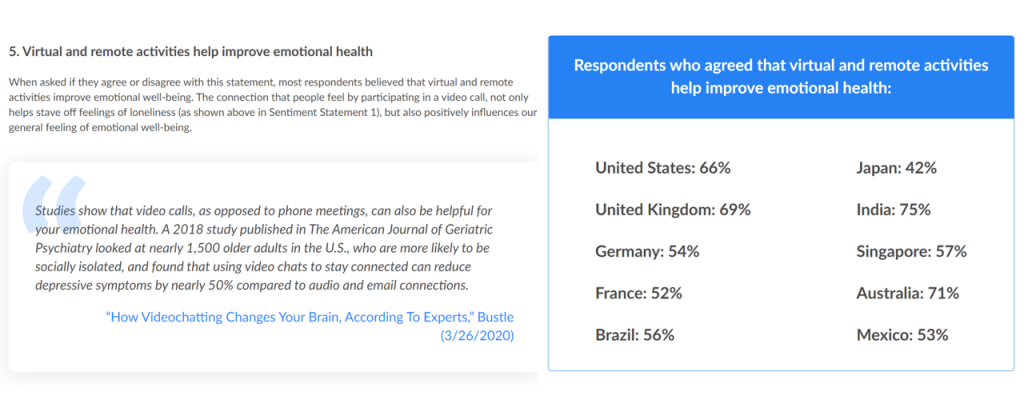
To that point, from aging grandparents down to kids, virtual connections helped bolster emotional health during the pandemic. The third graphic from the Zoom global survey report illustrates how different health citizens around the world felt about remote connections and emotional health, with U.S. consumers among the most bullish on the concept of virtual activities helping to improve mental health.
“One of Zoom’s focuses as a company and culture is about equity and access….we always focus on that,” Ron said to me. “If you look at the focus of this, anytime, we can reach out to people for access.”
In its conclusion on “going forward,” Zoom asserts that the tech we trusted to connect us personally and professionally through the first year of COVID-19 was more than simply “‘pandemic technology.’ Reliable video communications like Zoom are a way of life,” the company foresees.
Health Populi’s Hot Points: On Monday afternoon (9th August), HIMSS kicked off the week-long conference with a panel looking at the future of virtual care. One expert voice was Ateev Mehrotra of Harvard , one of my own go-to gurus on the evolving health landscape and public policy.
Ateev warned about digital divide risks for virtual care vs. phone calls (rich v poor, urban v rural). Furthermore, he envisioned the scenario that patients who receive the many growing flavors of virtual care — from phone to remote patient monitoring and real-time telemedicine visits — will be faced with new co-payments and explanations of benefits that may not make sense to them As telehealth grows we must educate health citizens on, simply put, Telehealth 101 — what are these services, how do they work, privacy implications and, to be sure, the costs covered by health plans and shared costs for the patient.
 To Ateev’s first point, I turn to a just-published research letter published in JAMA Network Open on the factors associated with use of and satisfaction with telehealth by adults in rural Virginia during the coronavirus pandemic. Maria Thomas of the Virginia Commonwealth University School of Medicine and colleagues from other Virginia-based organizations explored rural Virginians’ use of telehealth and experiences comparing demographics, health characteristics, literacy, internet access, and the probability of tapping into virtual care.
To Ateev’s first point, I turn to a just-published research letter published in JAMA Network Open on the factors associated with use of and satisfaction with telehealth by adults in rural Virginia during the coronavirus pandemic. Maria Thomas of the Virginia Commonwealth University School of Medicine and colleagues from other Virginia-based organizations explored rural Virginians’ use of telehealth and experiences comparing demographics, health characteristics, literacy, internet access, and the probability of tapping into virtual care.
“Implementation of telehealth will continue after the pandemic,” the authors forecast. But there’s a caveat: “our work highlights key considerations for rural residents to ensure that existing technology barriers are not exacerbated.”
To Ateev’s point, and my dear colleague Abner Mason, Founder and CEO of ConsejoSano’s ongoing reminder: we must be mindful of health equity, peoples’ access to broadband as well as hardware on-ramps and the cost of data plans, lest we further intensify the digital divides and health disparities still so prevalent in America.




 Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a