 The COVID-19 pandemic sparked a reappraisal of value-based care, a shift to remote and virtual care, and acceleration of healthcare stakeholders’ investments in Artificial Intelligence-based solutions, Philips discovered in the 2021 Future Health Index, the company’s latest survey conducted among 2,800 health care leaders working in 14 countries.
The COVID-19 pandemic sparked a reappraisal of value-based care, a shift to remote and virtual care, and acceleration of healthcare stakeholders’ investments in Artificial Intelligence-based solutions, Philips discovered in the 2021 Future Health Index, the company’s latest survey conducted among 2,800 health care leaders working in 14 countries.
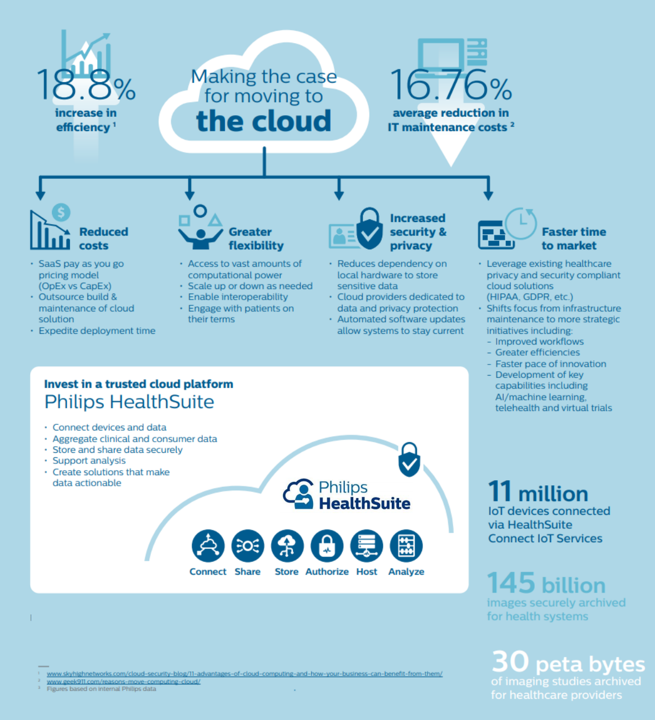
This week at the 2021 annual HIMSS conference, Philips is “making the case for moving to the cloud,” discussing the Philips HealthSuite, a cloud-based platform for connecting providers and patients, devices (and the data they generate), and care across the health care continuum.
That’s a big promise and vision, so to kick the tires on such a Holy Grail I had the opportunity to meet, virtually, with two key leaders of Philips’ health care business: Roy Jakobs, Chief Business Leader Connected Care, and Karsten Russell-Wood, Portfolio Leader, Post Acute & Home.
As I am attending #HIMSS21 virtually/online this week, avoiding a trip to Las Vegas but still wanting to be part of this important meeting, I was able to take a virtual tour of HealthSuite to learn more about the various workflows, stakeholders, and functions the platform supports. You can take a virtual tour, too, through the Philips Health Informatics Experience to get a more immersive experience of different use cases across the enterprise — and in patient’s hands and homes, as well.
[As a complementary sidebar, I experienced the analog to this presentation at CES 2021 when, once again, my trip to the largest annual consumer electronics show went all-virtual (again, missing a trip to Vegas), and Philips provided the consumer-facing version of their #CES21 announcements which you can click into here. And here was my assessment of the #CES2021 consumer health “yin” to Philips’ professional/medical care “yang” approach discussed at HIMSS 2021].
 “This is how you reduce friction in health care,” Karsten told me. “Friction is waste, cost, and inefficiencies in health care,” he explained, part of larger context of sustainability.
“This is how you reduce friction in health care,” Karsten told me. “Friction is waste, cost, and inefficiencies in health care,” he explained, part of larger context of sustainability.
In the words of the Philips virtual experience, we must bring people, data and technology together and connect the care journey. Moving to the cloud is an important pillar in re-building this friction-less, sustainable health system that, in the words of Philips, can “future-proof care.”
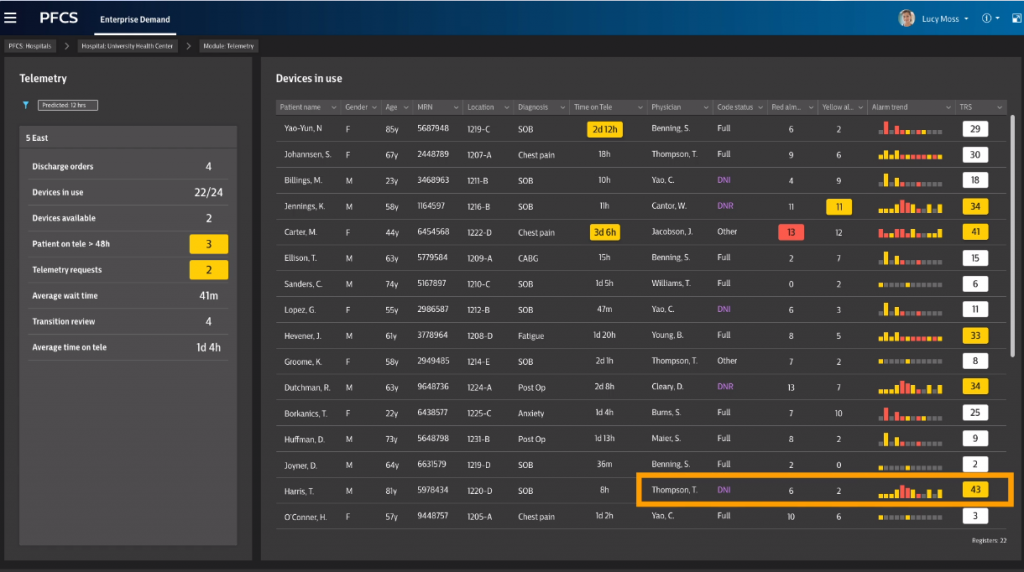 HealthSuite as a concept “spans the bedside to the webside,” Karsten characterized. Sustainability via HealthSuite is bolstered by balancing the clinical demands of patients with the supply side of clinicians, capital (such as inpatient beds and medical equipment), and that rarest of resources: time. By capturing data from the bedside and unit, in images and ancillary departments across an enterprise, and even from patients at home, the health care manager can better manage resources — as we all chant together, for each patient, the right setting, the right care, the right time.
HealthSuite as a concept “spans the bedside to the webside,” Karsten characterized. Sustainability via HealthSuite is bolstered by balancing the clinical demands of patients with the supply side of clinicians, capital (such as inpatient beds and medical equipment), and that rarest of resources: time. By capturing data from the bedside and unit, in images and ancillary departments across an enterprise, and even from patients at home, the health care manager can better manage resources — as we all chant together, for each patient, the right setting, the right care, the right time.
To Karsten’s point, this reduces friction and improves flow.
As the Future Health Index 2021 study learned, 65% of U.S. healthcare leaders are preparing for a shift to remote and virtual care.
 The resilient, sustainable health care future must enable that right patient/right setting/right care/right time continuum of care, which is part of Philips’ vision articulated well before HIMSS 2021.
The resilient, sustainable health care future must enable that right patient/right setting/right care/right time continuum of care, which is part of Philips’ vision articulated well before HIMSS 2021.
But the pandemic surely accelerated the adoption and use of telehealth, embraced by both patients and providers increasingly aligning to that right time-place-patient objective.
The only way to accomplish this is through partnerships (inside and outside of the legacy provider system) and using data that flows, is interoperable, and ready-for-AI.
Roy emphasized that while Philips most frequently works with Amazon/AWS, the company is as a practice “agnostic” to vendors and systems to allow the data flow.
 The continuum of care between hospital and home, and points in-between, necessities, “the ability to get access to that data, to track it, and interpret it and put intelligence on that,” Roy explained. “This has never been more important,” in light of the pandemic and tremendous strain on inpatient resources which, even today, we are finding in places that we wish were unthinkable — like pediatric ICUs.
The continuum of care between hospital and home, and points in-between, necessities, “the ability to get access to that data, to track it, and interpret it and put intelligence on that,” Roy explained. “This has never been more important,” in light of the pandemic and tremendous strain on inpatient resources which, even today, we are finding in places that we wish were unthinkable — like pediatric ICUs.
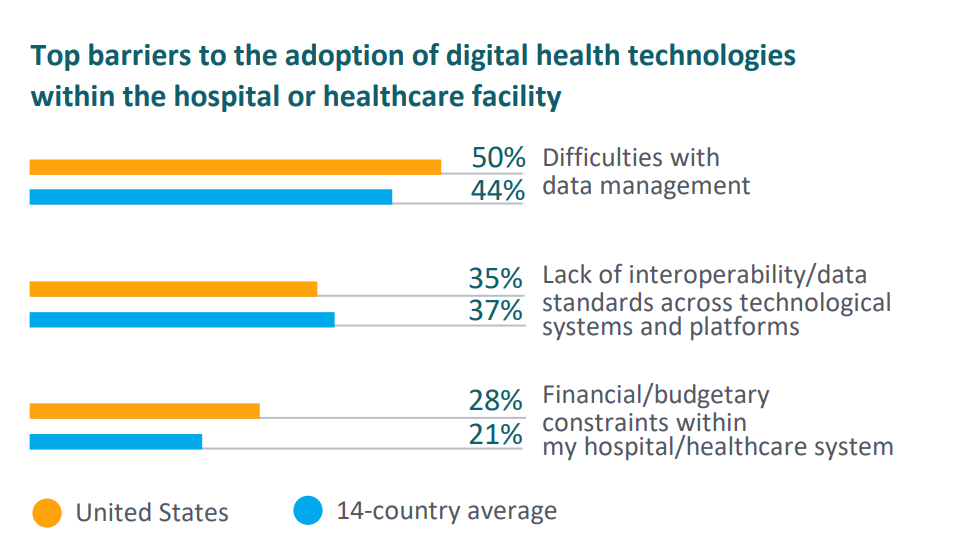
I revisited the 2021 Future Health Index for this data point, that in the U.S. healthcare leaders’ top barrier to the adoption of digital health tech within the institution is “difficulties with data management” and lack of interoperable data.
Care collaboration is the way of the future, Roy and Karsten both emphasized, and that is as important within the enterprise for clinical teams as it is when considering partnering to assure continuity of care that spans from the hospital to community touchpoints and the home.
 Health Populi’s Hot Points: Care collaboration is also part of a long-term sustainable health system. No one stakeholder in health care can deliver on the promise of a healthy society: most “health” and well-being is made outside of the hospital, at home, in a health citizen’s local neighborhood (that influential ZIP code or postal code), the school, the grocery store, the workplace (thinking hybrid in the pandemic economy — the power of the home as health hub).
Health Populi’s Hot Points: Care collaboration is also part of a long-term sustainable health system. No one stakeholder in health care can deliver on the promise of a healthy society: most “health” and well-being is made outside of the hospital, at home, in a health citizen’s local neighborhood (that influential ZIP code or postal code), the school, the grocery store, the workplace (thinking hybrid in the pandemic economy — the power of the home as health hub).
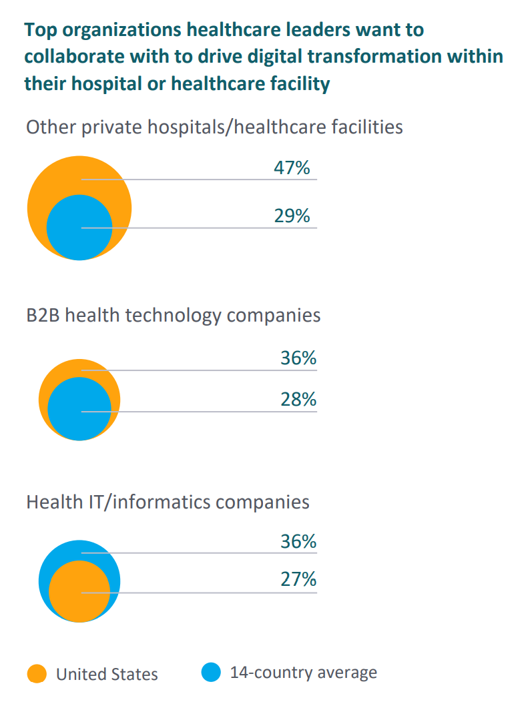
So Philips’ 2021 Future Health Index asked a question I was keen to revisit — what would be the top organizations with whom health care leaders would want to collaborate to drive digital transformation within their institution?
The last chart tells us the favored choice among U.S. healthcare leaders partnering in digital transformation “within” would be other hospitals and health care facilities (47%). These would include long-term care/rehabilitation centers, ambulatory and primary care centers (including urgent and retail health walk-in clinics), outpatient surgery centers, community health centers (e.g., FQHCs), pharmacies, and the home — growing in expectation by 50% in 3 years’ time (along with pharmacies as a place for routine delivery).
Another one-third of health executives would want to partner with health technology companies (36% thinking: Amazon, Google, Microsoft, Salesforce for example) for their digital transformations, as well as more traditional health IT and informatics companies (for example, Epic, Cerner, or Allscripts).
As we seek sustainable health care, Philips points to five key pillars to build on:
 Information architecture that takes advantage of “smart” technologies and the right tools for the organization’s objectives
Information architecture that takes advantage of “smart” technologies and the right tools for the organization’s objectives- Environmentally-minded sourcing to bolster sustainability – in a growing embrace of ESG principles
- Well-chosen collaborations with partners to foster innovation
- More care delivered outside of the hospital walls, in patients’ homes and in communities closer-to-home.
Finally, Philips’ has identified optimism pervading most health care managers’ mindsets, in and outside of the U.S.
That’s remarkable, isn’t it? Even as we face clinician burnout and a long, long period of muddling through the variants of the coronavirus and impacts on health citizens and national economies.
As Dr. Joseph Frassica, Philips’ Head of Research for the Americas and Chief Medical Officer North America, attests in the 2021 U.S. Index report, health care leaders are “looking to tackle some of the biggest social issues that the pandemic has brought into sharp relief,” calling out health equity and sustainability.
As Jan Kimpen, Philips CMO remarked in the global Index report, “Smart collaborations and meaningful partnerships will be critical to achieve digital transformation…we can expect greener healthcare systems over the next three years, with most healthcare leaders pledging to prioritize sustainable practices within their facility….Healthcare leaders are committed to building a future that is sustainable, adaptable and – above all – resilient.”




 Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a