“We don’t un-learn,” Dr. Amy Abernethy asserted as she shared her pandemic perspectives on a panel with 2 other former U.S. health policy and regulatory leaders. The three spoke about navigating compliance (think: regulations and reimbursement) in an uncertain world.
 An uncertain world is our workplace in the health/care ecosystem, globally, in this moment. So to give us some comfort in our collective foxhole, my last post for this week of immersion in #HIMSS21 is based on the keynote speech of Michael Dowling, CEO of Northwell Health.
An uncertain world is our workplace in the health/care ecosystem, globally, in this moment. So to give us some comfort in our collective foxhole, my last post for this week of immersion in #HIMSS21 is based on the keynote speech of Michael Dowling, CEO of Northwell Health.
Dowling keynoted on the theme of “Leading for the Future,” sharing his lessons learned during COVID-19. Dowling leads one of the largest health systems in the U.S., serving millions of health citizens residing in greater New York City and reaching out into the area’s boroughs and ‘burbs.
As the 2021 HIMSS conference comes to a close, it’s fitting for me to finish this week’s synthesis of the meeting (from afar, not on the ground in Vegas) with Dowling’s wisdom.
He kicked off his lessons focusing in on a theme that would resonate with the HIMSS audience: “COVID changed our relationship with technology forever.”
With that introduction, Dowling counted off many learnings that none of us will or should be able to un-learn.
Be agile and flexible. We demonstrated in the pandemic that we could be agile, reconfiguring hospitals quickly, moving patients and staff because we had to. “Can we maintain this level of agility and flexibility in how we go forward?” Dowling wonders.
 Relaxing regulations can inspire creativity and entrepreneurial behavior. Prior to the emergence of COVID-19, the use of telehealth in U.S. healthcare was relatively low (with Northwell Health actually a more mature user of virtual care). With government’s relaxing regulations, health care providers could move staff and resources virtually from place to place, regardless of State licensure or other barriers to providing telemedicine, remote monitoring, and other flavors of telehealth. If pre-COVID era regulations that were dismissed in the pandemic revert back, Dowling is concerned the progress made for telehealth in 2020 will slow or return to pre-pandemic levels of uptake.
Relaxing regulations can inspire creativity and entrepreneurial behavior. Prior to the emergence of COVID-19, the use of telehealth in U.S. healthcare was relatively low (with Northwell Health actually a more mature user of virtual care). With government’s relaxing regulations, health care providers could move staff and resources virtually from place to place, regardless of State licensure or other barriers to providing telemedicine, remote monitoring, and other flavors of telehealth. If pre-COVID era regulations that were dismissed in the pandemic revert back, Dowling is concerned the progress made for telehealth in 2020 will slow or return to pre-pandemic levels of uptake.
Scale matters to survive a public health crisis. Dowling pointed to the benefits of being a large integrated health care system with multiple hospitals, ambulatory care services and a broad portfolio of capabilities that enabled Northwell Health to be responsive to the needs of the pandemic and deal with the crisis. On the other end of the size spectrum, smaller independent facilities faced huge challenges pivoting in the pandemic without the support of an integrated system to scale their response.
 In healthcare, our compact with technology has changed forever. Technology enabled health care providers to expand health citizens’ access to care, and serve it up more conveniently. We need to better understand what technologies result in good quality outcomes and provider-supportive workflows versus those that are wasteful, unsafe, or cost-ineffective.
In healthcare, our compact with technology has changed forever. Technology enabled health care providers to expand health citizens’ access to care, and serve it up more conveniently. We need to better understand what technologies result in good quality outcomes and provider-supportive workflows versus those that are wasteful, unsafe, or cost-ineffective.
Do not underestimate the importance of preparing early for a crisis. Well ahead of the pandemic, Northwell Health had heavily invested in a central lab, the transport system, supply chain infrastructure with warehouses, and other investments made “years ago” that turned out to be success factors in dealing with the public health shock. We must avoid short-run thinking, as Dowling spells out in his book, Leading Through a Pandemic. Long-run strategic preparedness is an “absolutely important” learning experience coming out of COVID, Dowling knows.
Take care of your staff. “We knew but didn’t appreciate the primary importance of taking extraordinary care of your staff,” Dowling shared. “People will give you lists of things of how they are inspiring performance, and protecting safety. During COVID we had to do these things at the extreme for staff to keep them inspired,” he observed. We cannot lose this commitment of focusing on the needs of employees in the health care system on an ongoing basis.
Invest even more in research and science. Research and science matters, and being able to invest in them matters, Dowling emphasized. As we go forward, we must maintain that commitment and invest even more heavily than in the past. Without leveraging the benefits of science, we would not be coming out of COVID, Dowling believes.
We must address the poor state of the public health infrastructure. COVID-19 uncovered in the harshest of lights the underbelly of U.S. health care, Dowling colorfully noted. Now the question is, going forward, to make sure we don’t forget to meet the challenge of health inequities and disparities, and “don’t let public officials forget about it,” Dowling urged, recommending that we all collaborate with community-based organizations and directly with communities adversely impacted by the pandemic.
Public health crises, like the pandemic, are global. COVID-19 isn’t just a national problem. We must learn from our pandemic crisis and re-think how we in the U.S. work with other countries globally to anticipate pandemics in the future to develop collective responses. “We cannot disconnect from a connected world,” Dowling said. “We will not be success [in overcoming the coronavirus] unless we deal with other countries in a collaborative way.”
The hospital of the future is not the hospital of 2019. What is the hospital of the future look like? Dowling asked, something I’m charged to think about a lot in my scenario planning work. “What do we mean by ambulatory and outpatient care? What is the doctor of the future? What should doctor’s and nurse’s competencies be ten years from now?”
Finally, Dowling asked: “What kind of system are we going to create?”
COVID-19 “raises our obligation to do more than we ever thought we could, and definitely more than we did before,” Dowling concluded.
 Health Populi’s Hot Points: At his twitter handle @MichaelJDowling, this leader for the future characterizes himself as “Healthcare Optimist.”
Health Populi’s Hot Points: At his twitter handle @MichaelJDowling, this leader for the future characterizes himself as “Healthcare Optimist.”
Health leaders have influence, if we choose to use it, Dowling suggested. We can build a sense of unity, of community….to give oxygen to hope, in his words.
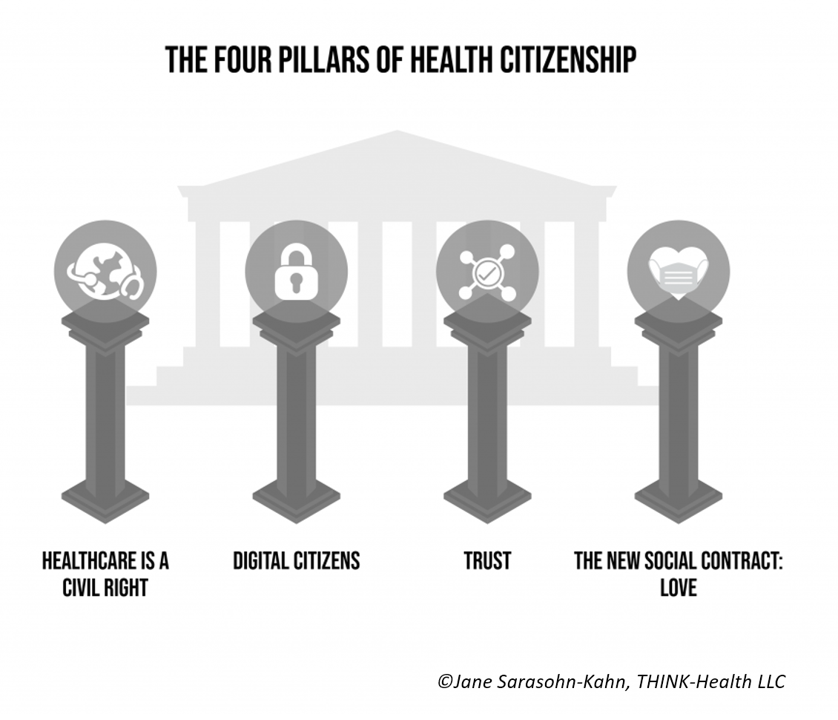
I leave you with Michael Dowling’s words of wisdom, to inspire and motivate all of us to do our part to build that community for better health and health care, and for every one of us. Each of us is a health citizen with rights and responsibilities: to engage in science fact, be role models for good health for each other, and to take good care of ourselves as best as we can. Our positive health behaviors, individually, actually inspire others’ in our social networks, and in our networks’ networks, we know from all being Connected.
As we return to our work and lives post #HIMSS21, I think of the book Connected reminding us that we have the opportunity to kick off virtuous cycles of good health behaviors. And, I return to another classic on my personal library shelf at home, Love Is the Killer App, by Tim Sanders, an early leader at Yahoo! In that book, Tim urged his readers to use the word “love” in the context of business.
Love must be one of our action verbs in re-imagining and re-building that better health/care system, I believe, bolstered in that belief by the lessons of Michael Dowling.





 Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a