Before the coronavirus emerged, the top causes of death in developed countries were heart disease, cancers, diabetes, and accidents. Then COVID-19 joined the top-10 list of killers in the U.S. and the issue of pandemic preparedness for the next “Disease X” became part of global public health planning.
 But the biggest health threat to human life is climate change, according to a new report from the World Health Organization titled The Health Argument for Climate Action.
But the biggest health threat to human life is climate change, according to a new report from the World Health Organization titled The Health Argument for Climate Action.
It’s WHO’s special report on climate change and health, dedicated to the memory of Ella Kissi-Debrah — a child who died succumbing to impacts from air pollution. According to the pathologist who carried out her post-mortem, Ella had, “one of the worst cases of asthma ever recorded in the U.K.”
Ella lived in Lewisham in southeast London. After her death in 2013, the Southwark Coroner’s Court found that air pollution “made a material contribution” to her death, “a landmark decision” according to a government advisor on air pollution. The coroner concluded that Ella was exposed to excessive levels of pollution. During the three years prior to her death, she was admitted to the hospital 30 times.
This profoundly moving case study graphically illustrates but one human example of the role of the environment on human health, which is the basis for WHO’s report and call-to-action.
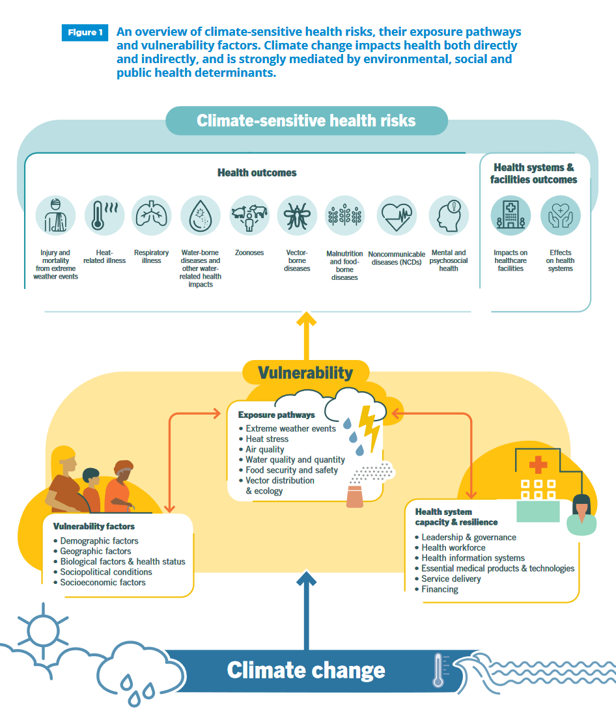
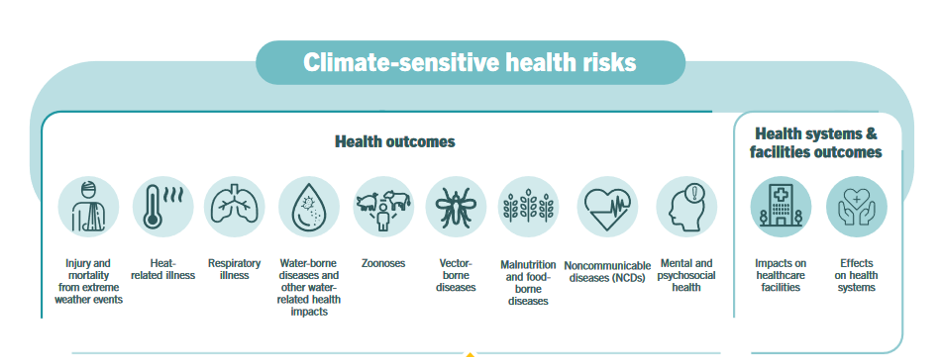
There are many climate-sensitive health risks, shown in the first diagram from WHO’s report. These include,
- Injury and mortality from extreme weather events
- Heat-related illness
- Respiratory illness (exacerbated for young Ella)
- Water-borne diseases
- Malnutrition and food-borne diseases, among other impacts on human health.
But there are also climate-related risks to health care institutions — think Hurricane Katrina and the images of patients having to be air-lifted out of urban New Orleans hospitals and nursing homes.
 Existing vulnerabilities enable those climate-related risks to more negatively impact health outcomes. Consider lack of connectivity for public health departments during Katrina, or poor water quality for the children living in Flint, Michigan.
Existing vulnerabilities enable those climate-related risks to more negatively impact health outcomes. Consider lack of connectivity for public health departments during Katrina, or poor water quality for the children living in Flint, Michigan.
The WHO report offers ten recommendations to inform and inspire our strategies and planning efforts to address climate change’s negative impacts on health, shown in the second chart. These focus on,
- Committing to a healthy recovery
- Recognizing that our health is not-negotiable
- Harnessing the health benefits of climate action to target those tactics with the greatest health, social, and economic gains
- Building health resilience to climate risks, in facilities and across sectors
- Creating energy systems that protect and improve climate and health
- Reimagining urban areas, transportation, and mobility
- Protecting and restoring nature as a foundation for our health — thinking nature-as-medicine
- Promoting healthy, sustainable, resilient food systems
- Financing a healthier, more equitable, greener future to build a well-being economy, and
- Listening to the health community and prescribing urgent climate action.
To that end, over 450 organizations representing over 45 million health workers in 102 different countries have signed a letter to Heads of State across the world urging climate action to protect their nation’s citizens’ health.
The effort is called the #HealthyClimate Prescription as an urgent call-to-action from global health workers (also using the hashtag #Climate Prescription). They wrote,
“While no one is safe from these risks, the people whose health is being harmed first and worst by the climate crisis are the people who contribute least to the problem and who are least able to protect themselves and their families against it—people in low-income countries and communities….Integrating health and equity into climate policy will protect peoples’ health, maximize returns on investments, and build public support for the urgently needed climate actions…The health cost savings will offset the costs of taking these actions.”
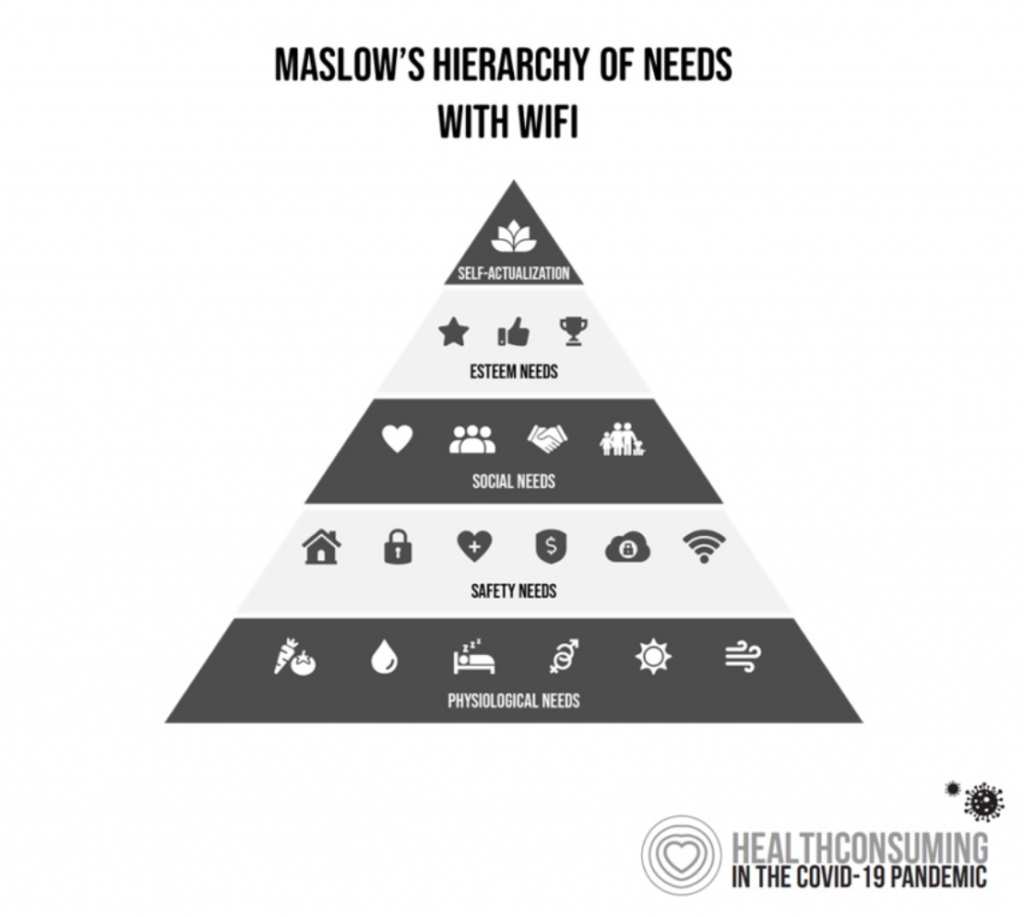 Health Populi’s Hot Points: The social determinants of health, those factors outside of medical care that shape our well-being and influence longevity, have included clean air and clean water on our most basic hierarchy of needs shown here at the base of the Maslow Hierarchy.
Health Populi’s Hot Points: The social determinants of health, those factors outside of medical care that shape our well-being and influence longevity, have included clean air and clean water on our most basic hierarchy of needs shown here at the base of the Maslow Hierarchy.
That base addresses our physiological needs, without which we mere humans would perish: food and nutrition, water, rest, clean environment, shelter from storms.
WHO’s detailed evidence now places climate change here as a basic need for health and well-being, and ultimately, survival.
This effort will take a health-in-all-policies approach from a public sector point of view. But the private sector — companies and business, NGOs and labor unions, educational institutions, and other community members — all have roles to play in this call-to-action.
The growing embrace by the Business Roundtable on ESG principles, for example, will help Big Business to address things they can do for climate change. This week at the World Bank and IMF meetings (being held virtually all this week), the world’s bankers and financial services leaders are convening with a big focus on sustainability and green finance. The meeting is emphasizing this year countries’ responses to the COVID-19 crisis, working to boost health care systems, protect the poor and vulnerable, support business, and help countries towards a green, resilient recovery in the words of the Bank.
Climate action is a major pillar for the meeting because of the inter-relationship between health, wealth, and economic recovery.
On 12th October, I attended a (virtual) meeting on Pandemic Preparedness held by the University of Leuven in Belgium and hosted by several organizations collaborating across their interests: the Institute for the Future at KU Leuven, Health House, the Institute of Tropical Medicine in Antwerp, and Vrije Universiteit Brussel, funded with help from the King Baudouin Foundation. Each session included videos curated with experts, globally experienced with crisis communications, science, trust, health education, and other aspects of getting ready in advance for the next pandemic.
One conversation with a leader from the UN Office for Disaster Risk Reduction (UNDRR) particularly struck me: she said that the health crisis was a governance crisis, where “common sense was thrown out the window.” Then another person discussed the link between individual human rights combined with solidarity and community required for a collective response to a future pandemic — a sentiment that eroded in the coronavirus crisis.
 We can and must do better for ourselves, our families, and each other. The climate-change-for-health gives us an opportunity to address this mother-of-all-health-risks collectively, using evidence-based principles and collaborating across our narrow siloes and special interests. We must remember the intimate weave of health, wealth, productivity, and environmental stability.
We can and must do better for ourselves, our families, and each other. The climate-change-for-health gives us an opportunity to address this mother-of-all-health-risks collectively, using evidence-based principles and collaborating across our narrow siloes and special interests. We must remember the intimate weave of health, wealth, productivity, and environmental stability.
One interesting collaborator in this sandbox is Arnold Schwarzenegger, who contacted Ella’s mom to offer support for her commitment to climate change and public health to honor her daughter. The former California Governor hosted a Talanoa-style dialogue on climate change and health called, “Pollution: Making the Invisible Visible” in May 2019. This was part of the Austrian World Summit in Vienna, and included the participation of Rosamund Adoo-Kissi-Debrah, Ella’s mum.
FUI, Talanoa dialogue convenes people to discuss issues through their personal stories. The process comes out of a Fiji Pacific island tradition, an inclusive process that enables all voices to be heard. “We are all in the same canoe, and an effective response to climate change must involve every single person on Earth,” Luke Daunivalu, a leader in Fijian government, helped to explain.
I’ll be keeping Ella and her own story in the front of my mind throughout our journey to address climate change for everyone’s health and well-being. See you in the canoe.




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for