“Americans remain in limbo between lives once lived and whatever the post-pandemic future holds,” the American Psychological Association observes in their latest read into Stress in America 2021, with this phase of the perennial study focused on Stress and Decision-Making During the Pandemic.
 The top-line: people face a daily web of risk assessment, up-ended routines, and endless news about the coronavirus locally and globally.
The top-line: people face a daily web of risk assessment, up-ended routines, and endless news about the coronavirus locally and globally.
While most people in the U.S. believe that “everything will work out” after the pandemic ends, the mental, emotional, and logistical daily distance between “now” and “then” brings uncertainty and indeed, prolonged stress.
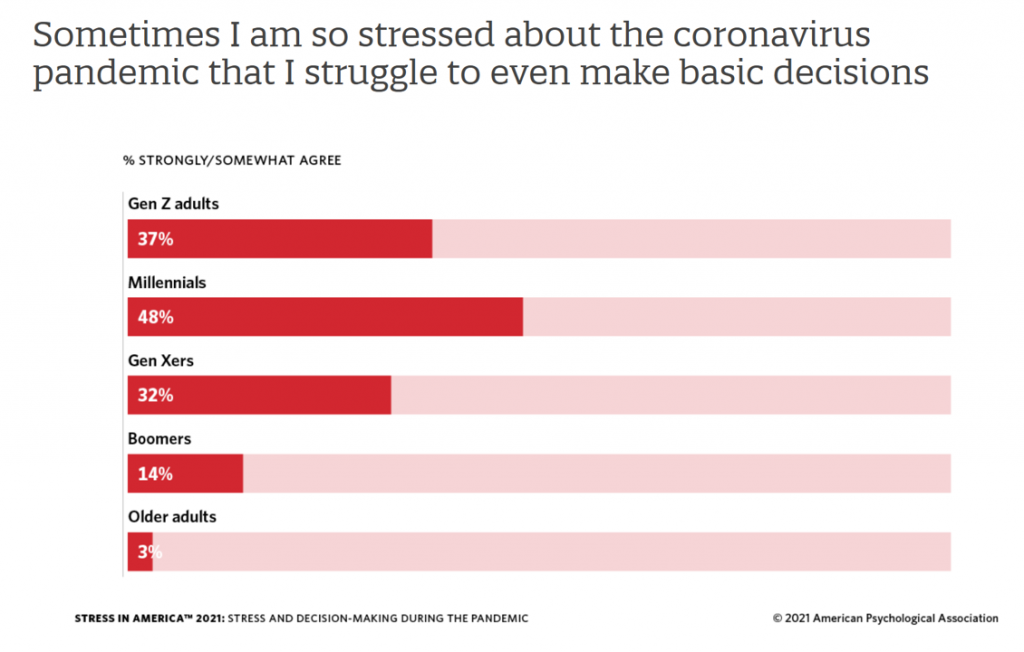
More Millennials, who generationally are sandwiched between older and younger people. feel the stress compared with other age groups — with Gen Z and Gen Xers following. Boomers and older people in America are less likely to feel so stressed by the pandemic, they struggle to make even the most basic decisions.
Those basic decisions, the APA details, can be as seemingly simple as what to eat, where to eat, or what to wear.
One in two people said the COVID-19 pandemic has made their planning for the future feel impossible.
 For parents, the strain has grown from 2020 into 2021: family responsibilities are a significant source of stress, and relationships are a source of stress. Thus, 4 in 5 parents said that they could have used more emotional support than they received over the past year.
For parents, the strain has grown from 2020 into 2021: family responsibilities are a significant source of stress, and relationships are a source of stress. Thus, 4 in 5 parents said that they could have used more emotional support than they received over the past year.
Furthermore, pandemic stress among people of color continues to be greater than stress on white Americans overall — especially among Hispanic adults who reported the highest levels of stress related to the pandemic. Their stress index topped at 5.6 versus 5.1 for Black as well as Asian adults, and 4.8 for non-Hispanic white adults in the U.S.
Why would Hispanic adults in the U.S. be hit disproportionately with stress in the pandemic era? Because of the unequal burden Hispanic people carry in the wake of COVID-19: more Hispanic adults were more likely to struggle with stress int he pandemic, more likely to know someone who had been sick or died of complications due to the coronavirus (42% versus 25% of non-Hispanic white adults).
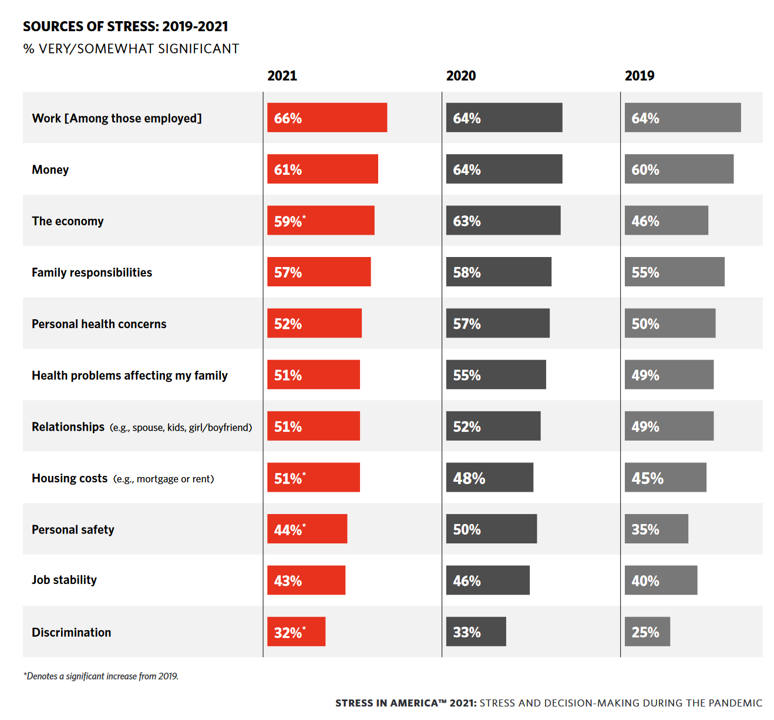
The second chart details the most significant sources of stress from 2019 into 2021. Those stress sources that increases in the three years were, in terms of statistical significance:
- The economy, increasing from 46% stressed to 59% stressed
- Housing costs, growing from 45% stressed to 51% stressed
- Personal safety, increasing from 35% stressed to 44% stressed, and,
- Discrimination, climbing from 25% stressed to 32%.
As a result, three in four U.S. adults have experienced some behavioral impact due to stress, such as headaches (34%), feeling overwhelmed (34%), fatigued (32%), or changes in sleep (32%). These were more likely to impact younger people than older folks in the U.S.
The APA’s August/COVID Resilience Survey was conducted online by The Harris Poll in August 2021 among 3,035 U.S. adults 18 and over.
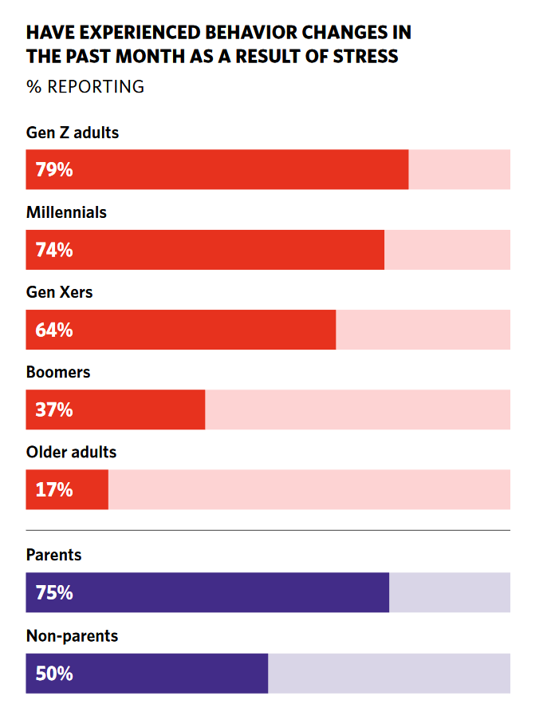
Health Populi’s Hot Points: Those pandemic-era headaches and sleep habit changes have been impacting more younger people than older people in America, shown in the last chart.
In addition to pain and sleep impacts, over one-third of people said they are eating to manage stress, roughly the same percentage in 2021 as recorded in 2020.
This study crafted a Resilience Scale to measure how people responded to stress in 2021. Over one-half of people said they are struggling with the “ups and downs” of the pandemic: one-fourth were considered being of low resistance in the APA scale, measured as 1.00 to 2.99 out of 10.0. 48% of people in America had an average resilience index of 4.31 to 5.00.
Younger people, parents, and people with less than $50,000 in household income were more likely to have low resilience scores. These people were more likely to say their stress was higher in the past month than earlier in the pandemic, as well as higher than before the pandemic.
This group of highly-stressed people were also more likely to say they struggled to make basic daily decisions.
They also felt they could have used more emotional support than they received over the past year.
The pandemic certainly gave us the gift of knowledge in having to face the ubiquity of mental health in Americans’ overall health and well-being….or lack thereof. Most people in the U.S. have been faced with mental and behavioral stressors and subsequent physical manifestations of that stress in eating, sleeping, and daily decision making fog.
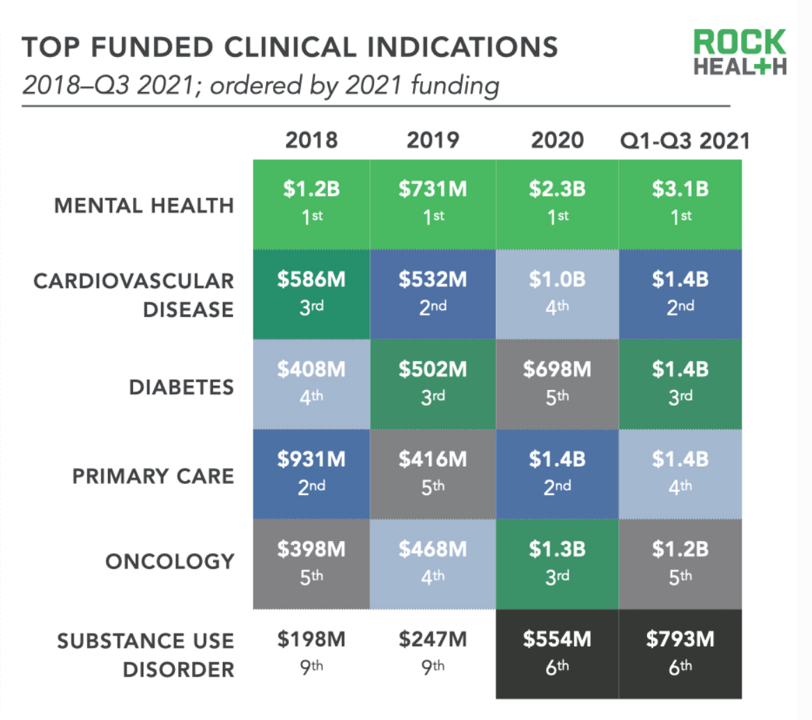 The growing supply of teletherapy serving more people at scale who need and want to access services has been encouraging to see, with investments in digital mental health hitting $3.1 billion and $793mm for substance use disorder for the first three quarters of 2021 based on Rock Health’s numbers. Galen Growth calculated that some $6.12 billion has been invested in mental health digital health cumulatively from 2017 to H1 2021.
The growing supply of teletherapy serving more people at scale who need and want to access services has been encouraging to see, with investments in digital mental health hitting $3.1 billion and $793mm for substance use disorder for the first three quarters of 2021 based on Rock Health’s numbers. Galen Growth calculated that some $6.12 billion has been invested in mental health digital health cumulatively from 2017 to H1 2021.
The leader of the ATA (American Telemedicine Association), Ann Mond Johnson, has a mantra that #TelehealthIsHealth.
That is indeed the case. Now, on to scaling this for all who need access to quality, truly accessible mental and behavioral health services. For health citizen/patient demand to meet up with that growing supply side will require health plans, payment designs, and social barriers to align.




 Thank you FeedSpot for
Thank you FeedSpot for