Discrimination in health care is reported by more people in the U.S. than in Germany, Spain, or the U.K., we learn in the research reported in The Intersection of Health Equity in Communities & Business Strategy: A Call-to-Action, from Omnicomm PR Group (OPRG) and Atlantic Insights. 
The study was conducted among 6,000 people living in Germany, Spain, the United Kingdom and the United States, fielding 1,500 interviews in each of the four countries in March 2023.
The U.S. survey sample included 375 people identifying as Black, White, Hispanic, or Asian/Indigenous (summing to the N of 1,500). In addition, 500 people in this cohort of 1,500 were dealing with a mental or physical disability.
The study revealed five themes that underpinned health equity across the four nations studied:
- Discrimination
- Broken trust and not feeling safe
- On the upside, community engagement opportunities
- Digital divides, and,
- A lack of emotional intelligence and connection felt by many health citizens.
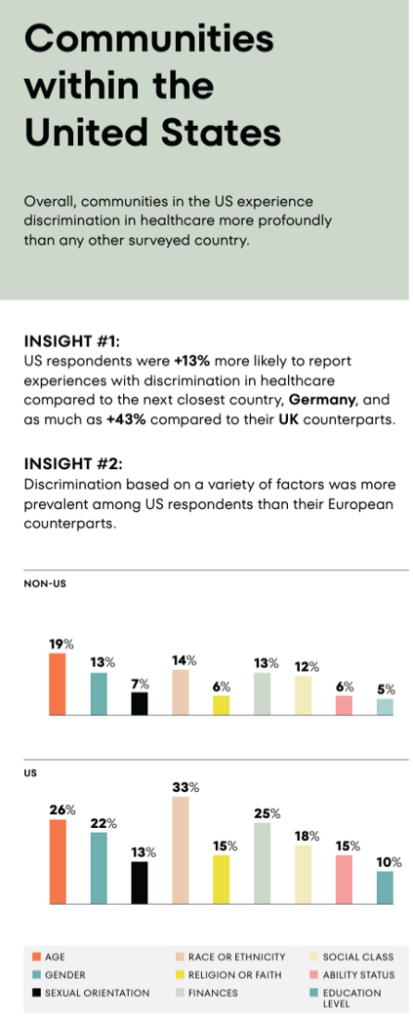
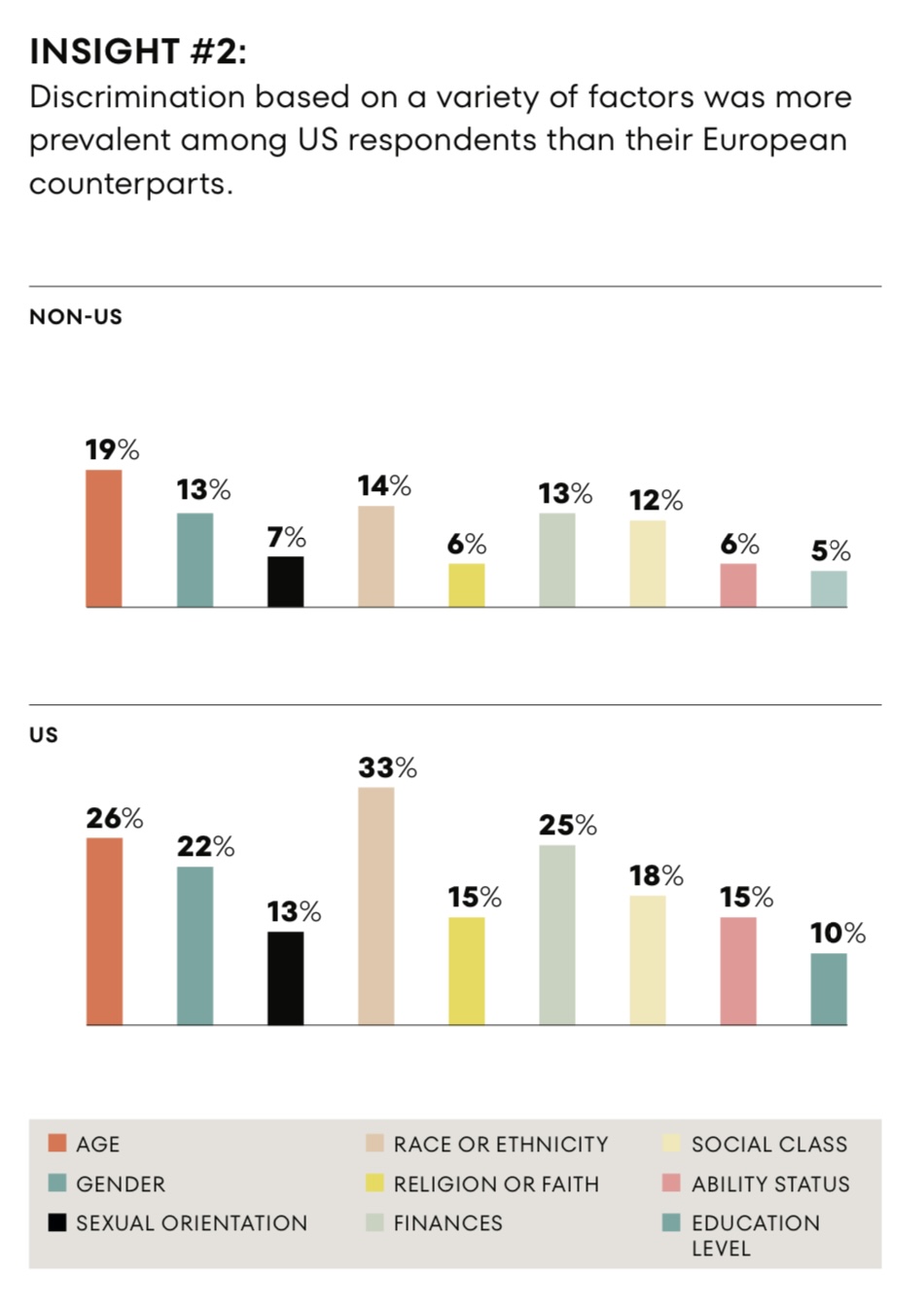
The second graphic focuses on the U.S. data findings, clearly illustrating that more people living in the U.S. are more likely to feel discrimination — 13% more likely to feel discrimination in health care settings than peers in Germany or the UK.
The bottom chart arrays data on feelings of discrimination by various factors: most notably, discrimination based on race or ethnicity yields the highest level, followed by the factors of age, finances, gender, and class.
The biggest differences in discrimination feelings between U.S. residents and those outside of the U.S. are for race/ethnicity (a 19% point delta), financial (12% differential, roughly double the rate for U.S. folks), gender (a 9% point difference) and ability status, also a 9% point delta over twice as great in the U.S. as in the non-U.S. nations in the study.
The study convened many advisors from a range of fields in public health, health equity, disability/ability community, academia, clinical practice, and community leaders in the LGBTQIA+ community, among others. These experts in the field offered up many recommendations and calls-to-action, among them…
- ”Go to Them,” that is, to the communities who have lost trust — via targeted outreach to help understand and build solutions based on peoples’ priorities.
- ”Ask Why, More,” to dig deeper into conversations with people simply asking the open-ended question, “Why?” Then….listen well.
- Dispel myths that have come out of history — and build bridges of trust, with small actions over time.
Then there is technology: “There is a need for AI solutions to recognize diversity,” the report asserts. “AI tools can bring transformative changes that enhance the delivery of care and improve health outcomes.” As Dr. John Whyte, WebMD’s Chief Medical Officer, calls out, “Doctors who don’t use AI are going to be replaced by doctors who do” as well as to figure out how to best use the tools and, as Dr. Whyte rightly notes, “to ensure empathy rises to the top.”
The calls-to-action are five — they are simple and they are bold:
- Eliminate bias and discrimination from health care.
- Engender trust through community and civil society engagement.
- Engage community and civil society int he development and implementation of interventions across the care continuum, from diagnostics to continued care.
- Leverage digital health to scale best practices in healthcare and delivery — leaving no one behind.
- Speak to peoples’ values, connect and lead with care and compassion.
Health Populi’s Hot Points: The CEO of BlackDoctor.org, Reggie Ware, makes the business case for dealing with health equity, saying, “A laser focus on health equity is not charity or philanthropy. It’s a business imperative and revenue driver that, if not addressed, has serious business ramifications.”
I discussed the economic burden of health inequities in the U.S. in a 2022 essay, weaving data from several studies that quantified the cost of health disparities using various methods. Based on a Deloitte study in 2022, the cost amounted to at least $1,000 of additional health care spending per capita — which acts essentially as a tax on U.S. health citizens. That’s just one aspect of the many cost-layers of health inequity. As Brian O. Buckley, Director of Health Equity Initiatives with NCQA, observed in the report, “health equity is a team sport and requires our collective effort worldwide.”




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for