Health care access is a challenge in rural and urban areas, cities and suburbs, and across more demographic groups than you might realize, as we see wait times grow for appointments, primary care shortages, and delays in screening plaguing health systems around the world.
In the Future Health Index 2024, Philips’ latest annual report presents a profile of the state of health care focused on how to provide better care for more people.
For the report, Philips surveyed a total of 2,800 healthcare leaders consisting of 200 respondents in 14 countries: Australia, Brazil, China, India, Indonesia, Italy, Japan, the Netherlands, Poland, Saudi Arabia, Singapore, South Africa, the United Kingdom, and the United States. The study was fielded between December 2023 and February 2024.
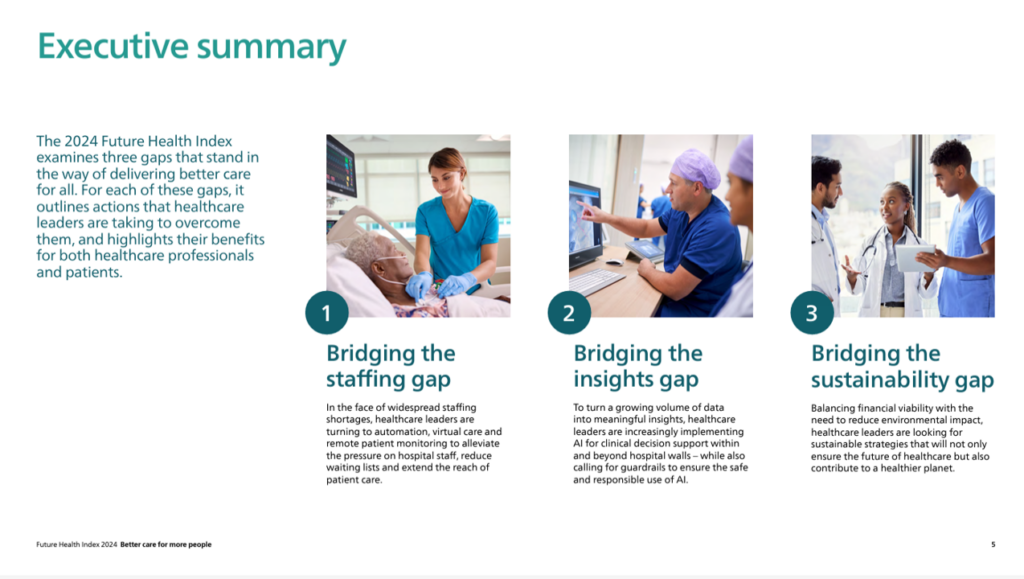
The interviews revealed three calls-to-action for addressing the challenge of channeling better health care services to more people:
- Bridging the staffing gap, taking on clinician burnout and staffing shortages
- Bridging the insights gap, corralling vast streams of data and sense-making to surface useful advice and actions — while assuring ethical applications of AI, and
- Bridging the sustainability gap — both in terms of financial viability and environmental stewardship.

First, the staff shortage which is a worldwide phenomenon, from Australia to the U.S. in terms of countries covered in the study. Globally, two-thirds of health care leaders see deteriorating staff well-being, physical and mental. That leads to over one-half of health care leaders sensing a growing likelihood of staff leaving their jobs due to healthcare professionals burning out.
Here’s where technology can help scale the precious human resources that are physicians, nurses, pharmacists, allied health professionals and other trained clinicians whose well-being has eroded starting before the pandemic. The chart illustrates health care leaders’ perspectives on automation for bolstering staff productivity and wellness at work.

The most prevalent use of automation across over one-half of the health care leaders’ organizations is with billing processes, appointment scheduling, patient check-in, staff scheduling, and clinical data entry.
Least-used yet but most-likely to implement in the next 3 years is automation for workflow prioritization — thing triage for workflow.
Over one-third of health care leaders plan to implement automation in the next 3 years for equipment maintenance and monitoring, clinical documentation and notetaking, and medication management.

Next, consider how to bridge the insights gap, given the vast amounts of data flowing from many care sites within and outside but allied to the health care organization. 94% of health care leaders say their organization is facing at least one data integration challenge negatively impacting their ability to provide timely quality care.
The pie chart identifies several of these challenges, each of which affects over one-third of the health care leaders polled in the research — including spending time accessing and integrating data results taking time away from care-giving; increased operational costs due to inefficiencies; limited coordination of care between providers and departments; repeating tests and scans due to medical record inefficiencies; and, increased risk of errors and patient safety issues.

Finally, we get to sustainability which translates into financial as well as environmental challenges.
Philips found that health care leaders are looking to balance fiscal pressures with environmental footprint goals for carbon reduction as well as other goals for planetary health.
86% of health care leaders see that reducing CO2 emissions and health care’s environmental impact are part of their mission or priority. Just under one-half of these executives have already implemented recycling waste programs, reduction or hazardous substances, and water and energy conservation programs. Over one-third are prioritizing reuse of medical equipment and supplies.
Looking forward, sustainable procurement, investing in green buildings and infrastructure, patronizing suppliers who have sustainable targets in place and other tactics will be implemented in the next three years.
Health Populi’s Hot Points: Achieving these calls-to-action will require collaboration and collective action in health care organizations’ communities. Philips concludes the report noting the need for further collaboration across the health care ecosystem — health systems and hospitals, technology companies, suppliers, and policy makers. 
Another tactic to embed in dealing across all three of the calls-to-action is the role that telehealth and virtual care can play for two of the three factors — dealing with staff shortages and sustainability in reducing carbon and saving people time while bolstering patient experience and convenience. Remote monitoring and hospital-to-home strategies will be part of a growing distributed care delivery system, designed with the best practices of privacy-by-design, ethics-by-design, and omnichannel platforms that are enchanting and seamless for patients and caregivers to access and use.
As Dr. Shez Partovi, Philips’ Chief Innovation & Strategy Officer, said, “When I think of the future of healthcare delivery, I think of ‘your care, your way.'”





 Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a