The Federation of American Scientists (FAS) was founded in 1945 by a group of scientists concerned about the atomic bomb — sharing a mission to focus on technology, science, and innovation to, in the Association’s words, “work toward a safer, more equitable, and more peaceful world.” 
Nearly 80 years after the organization’s launch, the FAS is focusing on the growing role of artificial and augmented intelligence across the many areas that touch peoples’ lives — including health care and well-being.
The FAS published a state-of-the-nation essay on June 27 on Improving Health Equity Through AI. The piece addresses challenges and opportunities, a balancing of, the facts that,
- “These systems can alert clinicians to potential drug interactions, suggest preventive measures, and recommend diagnostic tests based on patient data,” noting that,
- “Inequities in CDS AI pose a significant challenge to healthcare systems and individuals, potentially exacerbating health disparities and perpetuating an already inequitable healthcare system,” as well as increasing costs and eroding health citizens’ trust in their health/care systems.
The FAS asserts that we need regulatory frameworks, investment in AI accessibility, incentives for data collection and collaboration, and regulations for auditing and governance of AI systems used in CDS systems/tools. By addressing these challenges and implementing proactive measures, policymakers can harness AI’s potential to enhance healthcare delivery and reduce disparities, ultimately promoting equitable access to quality care for everyone.
With the objective of reducing health and care disparities and expanding equitable access to quality health care for all, herein is a call-to-action to promote the use of AI mindfully establishing and embedding regulatory frameworks, investment in AI accessibility, incentives for data collection and collaboration, and regulations for auditing and governance of AI systems.

The FAS notes that the Medicare and Medicaid programs in the U.S. cover about 40% of Americans, and therefore have the opportunity to design and scale responsible AI to patients in these plans.
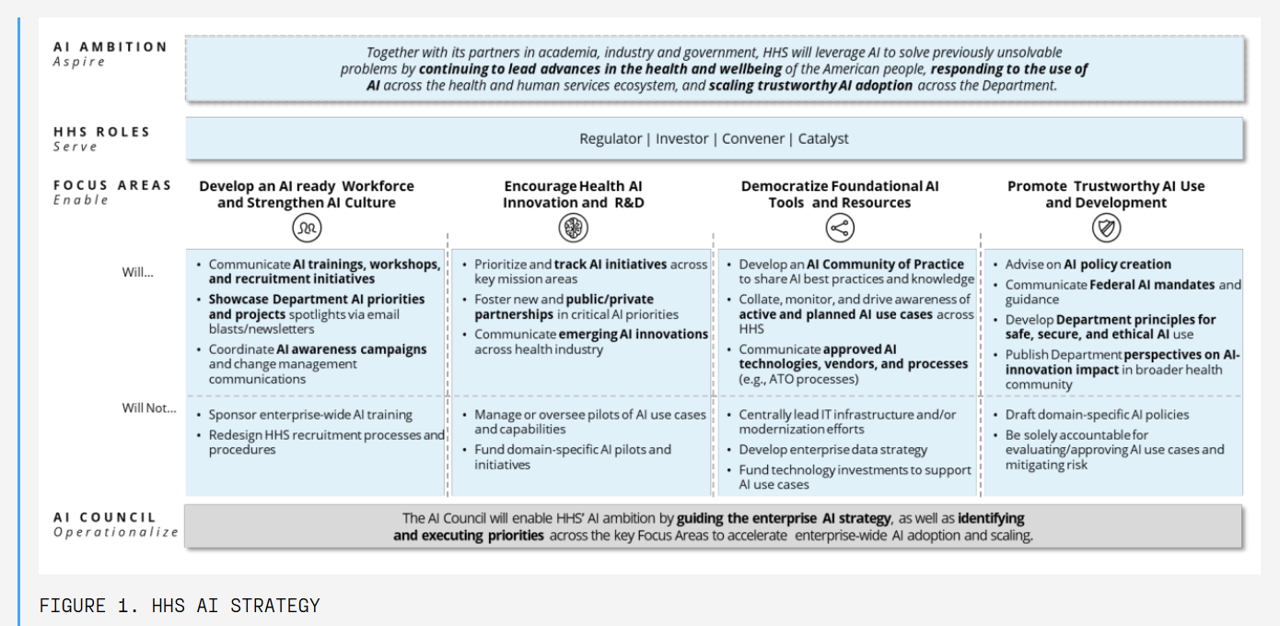
As part of the agency’s AI strategy, the U.S. Department of Health and Human Services developed a rubric for AI “hygiene” shown in this chart. The HHS AI strategy is organized in four focus areas: the workforce, innovation and R&D, democratizing tools and resources, and promoting trust.
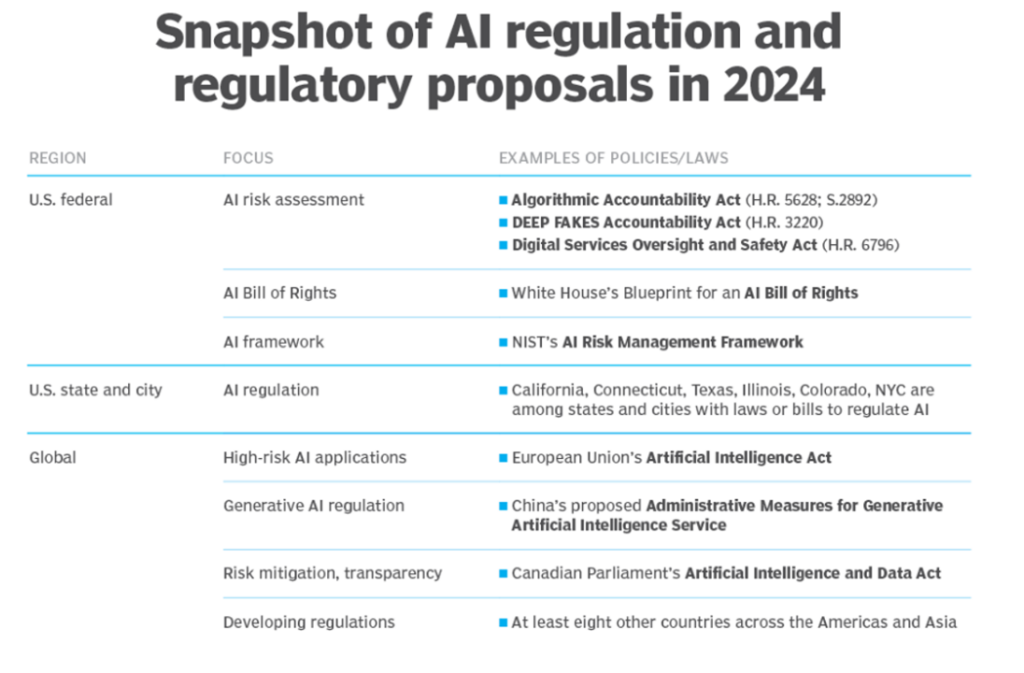
Among many recommendations, the FAS urges that the U.S. Congress enforce accountability for advanced algorithms through legislation — such as amending and passing the 2023 Algorithmic Accountability Act to assure all organizations involved in developing and using AI in health care have transparent access to the results of audits resulting from that accountability process.
In addition to accountability and auditability, FAS’s call-to-action also addresses the importance of funding to support AI access for health providers who serve under-served populations and folks in the social safety net and rural geographies, ensuring funding flows to providers such as Federally Qualitied Health Centers and rural providers, along with research organizations and private-public partnerships deploying care and solutions to vulnerable patient populations.
A third key consideration for you to know about in the FAS discussion is the scientists’ collective belief that AI and machine learning should be helpful and useful, and that regulations and guardrails should not stifle innovation — but privacy and data security must be assured as diverse and inclusive data are shared and collected to mitigate biases and assure broad representation in the patient data. The FAS believes that this aspect of health care AI developers and users should be evaluated by an accrediting organizations such as the Joint Commission’s Healthcare Equity Certification. 
Health Populi’s Hot Points: The FAS scientists also recognize the foundational importance of privacy regulation in the context of patients’ — as health citizens’ — willingness to share personal data for AI to do its thing effectively. Here is the fourth pillar of the DHHS AI Strategy to promote trustworthy AI use and development.
FAS wrote another policy paper on privacy on June 27 saying that the American Privacy Act (APRA) Must Include Online Civil Rights. Here, the scientists are calling for the House Energy & Commerce Committee to assure that a new privacy rights law include civil rights protections that ensure personal data is safely and fairly handled regardless of race, gender, sexuality, age, or any other protected characteristics.
Getting AI right — that is equitable and most useful — will be a team sport bringing diverse and inclusive data together with health ecosystem stakeholders, playing fairly together in patients’ trusting their sharing personal health information with those organizations who will develop, deploy, and use AI-informed clinical decision systems. Without attending to baking in equity-by-design and privacy-by-design, the scientists of FAS recognize that algorithmic bias could exacerbate health disparities and injustices — which also lead to increased costs to the health care system, payors, communities, and individuals in the form of lost life-years, quality of life, and human dignity.





 Grateful to Gregg Malkary for inviting me to join his podcast
Grateful to Gregg Malkary for inviting me to join his podcast  This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're
This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're