Women in the U.S. have lower life expectancy, greater risks of heart disease, and more likely to face medical bills and self-rationing due to costs, we learn in the latest look into Health Care for Women: How the U.S. Compares Internationally from The Commonwealth Fund. 
The Fund identified four key conclusions in this global study:
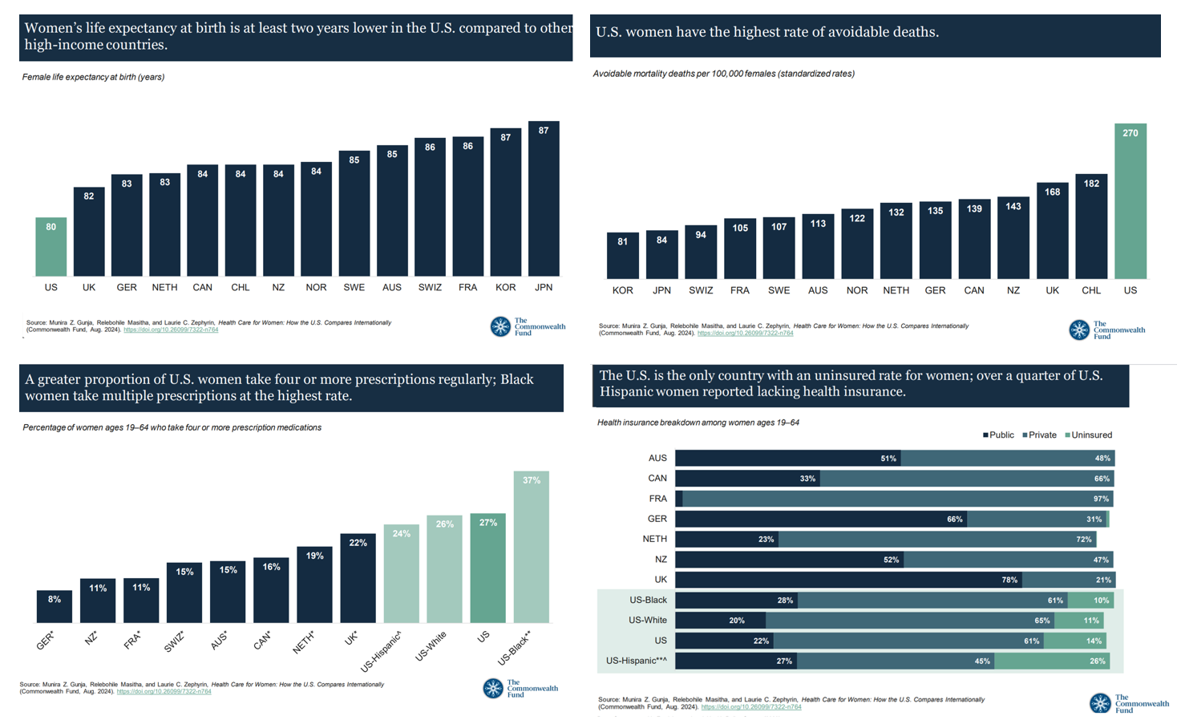
- Mortality, shown in the first chart which illustrates women in the U.S. having the lowest life expectancy of 80 years versus women in other high-income countries;
- Health status, with women in the U.S. more likely to consume multiple prescription drugs on a regular basis;
- Access to care, with the U.S. being the only country in this analysis with a “considerable” proportion of women who are uninsured; and,
- Affordability of care, where women in America have among the highest rates of skipping or postponing needed care due to cost — and also facing higher risk of medical bill issues.
The results are based on analyzing data from the CDC, the OECD, the Institute for Health Metrics and Evaluation, and the organization’s 2023 International Health Policy Survey conducted among adults age 18 and over in many countries.

Another signal of poor health system performance is a population’s rate of avoidable deaths — in which case women in the U.S. also draw the short end of the mortality stick.
Here in the second chart, we look to the far right to see the highest rate of avoidable death compared with other nations in the Fund’s study. That rate is 270 avoidable mortality deaths per 100,000 females; for Chile, second on this sobering statistic, that rate is 182 and in the UK, it’s 168.
The next in line covers women in New Zealand with roughly one-half the rate of avoidable deaths at 143.

Among many factors contributing to U.S. women’s relatively poorer health outcomes is financing of health care in America — in the data point captured in the third chart, one line item is self-rationing care, that is skipping or delaying medical services or prescription medicine fills because of the cost.
The far right end of this chart breaks out such self-rationing because by U.S. women overall — at 51% — and then broken out by race/ethnicity, with Hispanic women in America having the highest risk of delaying care due to cost. This is an issue women in other countries face at much lower rates — like 15% in the Netherlands, 18% in Germany and the UK, and 20% in France. 
Health Populi’s Hot Points: This paragraph clipped from the Fund’s report conclusions summarizes some of the key challenges women in America face when trying to access health care: some of those elements are lack of relationship with a physician ongoing, mounting medical bills, and uninsurance.

This chart tracks countries by health citizens’ lack of health insurance — identified by the green bars.
There is no green indicated for the other countries considered in this study — uninsurance is a uniquely American phenomenon which women peers living in Australia, Canada, France, Germany, the Netherlands, New Zealand, and the United Kingdom do not have any experience with. 
Lack of health insurance is one of the basic social determinants of health — shown here in Kaiser Family Foundation’s discussion on SDoH. Having health insurance coverage is impactful on a person’s life just as clean air, clean water, nutritious food, education, a fair wage job (and a consistent one) are to a person’s overall health and well-being — whatever country one resides in.





 Grateful to Gregg Malkary for inviting me to join his podcast
Grateful to Gregg Malkary for inviting me to join his podcast  This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're
This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're