 8 in 10 people in the U.S. believe that total privacy in the digital world is history, based on a survey from Accenture conducted online in March and April 2014 and published in the succinctly-titled report, Eighty Percent of Consumers Believe Total Data Privacy No Longer Exists.
8 in 10 people in the U.S. believe that total privacy in the digital world is history, based on a survey from Accenture conducted online in March and April 2014 and published in the succinctly-titled report, Eighty Percent of Consumers Believe Total Data Privacy No Longer Exists.
84% of U.S. consumers say they’re aware what tracking personal behavior can enable – receiving customized offers and content that match one’s interests. At the same time, 63% of people in the U.S. also say they have a concern over tracking behavior. Only 14% of people in the U.S. believe there are adequate safeguards in place to protect their personal information.
But people are split, 50/50, between receiving relevant offers even it means tracking their behavior, vs. companies no longer tracking them even though they may receive irrelevant information.
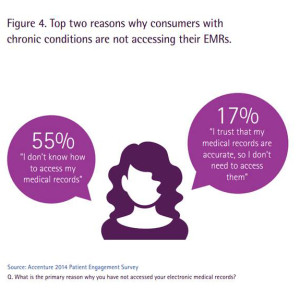 Accenture also found, in another survey of U.S. consumers, that people want to access their electronic medical records but most still don’t know ‘how’ to do that. While 87% of people believe it is important to have control over their personal health data, 55% believe they have little or no control over it, which yields a big confidence gap among U.S. health consumers who are seeing their data moving from paper to digital medical records as their health providers have been adopting and implementing EMRs over the past few years in response to incentives in the HITECH Act. (For more on this, see 4 in 5 doctors in American use an EHR, but most not ready for Stage 2 here in Health Populi). My take on Accenture’s consumer/EMR survey is that in a world of digital health data, sicker people are willing to trade off (some) privacy risks.
Accenture also found, in another survey of U.S. consumers, that people want to access their electronic medical records but most still don’t know ‘how’ to do that. While 87% of people believe it is important to have control over their personal health data, 55% believe they have little or no control over it, which yields a big confidence gap among U.S. health consumers who are seeing their data moving from paper to digital medical records as their health providers have been adopting and implementing EMRs over the past few years in response to incentives in the HITECH Act. (For more on this, see 4 in 5 doctors in American use an EHR, but most not ready for Stage 2 here in Health Populi). My take on Accenture’s consumer/EMR survey is that in a world of digital health data, sicker people are willing to trade off (some) privacy risks.
 Health Populi’s Hot Points: This week witnessed the fifth annual Health Datapalooza in Washington DC, bringing together entrepreneurs, public policy makers and regulators, health providers and patients to discuss the state of health data, Big Data, technologies to power and analyze that data, opportunities and concerns. On June 3rd, in the midst of the excitement of #HDPalooza, The Office of the National Coordinator of Health IT (ONC) published an announcement in the Federal Register about their reorganization, done in response to reduced funding and realignment. The announcement lists the following key identified roles in the new-and-improved ONC:
Health Populi’s Hot Points: This week witnessed the fifth annual Health Datapalooza in Washington DC, bringing together entrepreneurs, public policy makers and regulators, health providers and patients to discuss the state of health data, Big Data, technologies to power and analyze that data, opportunities and concerns. On June 3rd, in the midst of the excitement of #HDPalooza, The Office of the National Coordinator of Health IT (ONC) published an announcement in the Federal Register about their reorganization, done in response to reduced funding and realignment. The announcement lists the following key identified roles in the new-and-improved ONC:
A. Immediate Office of the National Coordinator (ARA)
B. Office of Clinical Quality and Safety (ARG)
C. Office of Planning, Evaluation, and Analysis (ARB)
D. Office of Standards and Technology (ARC)
E. Office of Programs (ARD)
F. Office of Public Affairs and Communications (ARH)
G. Office of the Chief Operating Officer (ARE)
H. Office of the Chief Privacy Officer (ARF)
I. Office of Policy (ARI)
J. Office of Care Transformation (ARJ)
K. Office of the Chief Scientist (ARK).
In the context of the above-the-Hot Points health data privacy discussion, it’s good to see “H,” the Office of the Chief Privacy Officer having a seat at the ONC Big Table.
But it seems the key health ecosystem player doesn’t have a Big Chair at that Big Table: the consumer, the patient, the caregiver.
This missing persona will be represented, based on the announcement, in two places:
- In “E,” the Office of Programs, which “supports care providers in the adoption, implementation and optimization of health information technology and adaptation to new care and payment models. The Office also oversees consumer use of electronic personal health information and activities for certification of health information technology;” and,
- In “B,” the Office of Clinical Quality and Safety, which “includes the Chief Nursing Officer (CNO) who advocates for patient care, clinical, and staffing nursing standards at the national level for ONC.”
Thank goodness for the nurses.
 The challenging state of Big Data, health privacy and security in America has been raised in recent reports from the President’s Council of Advisors on Science and Technology, the FTC (reported on here in Health Populi), the World Privacy Forum on health-scoring of Americans, and medical debt and credit scores from the Consumer Financial Protection Bureau. In the current climate, U.S. consumers’ health data feels very much up-for-grabs as private sector currency.
The challenging state of Big Data, health privacy and security in America has been raised in recent reports from the President’s Council of Advisors on Science and Technology, the FTC (reported on here in Health Populi), the World Privacy Forum on health-scoring of Americans, and medical debt and credit scores from the Consumer Financial Protection Bureau. In the current climate, U.S. consumers’ health data feels very much up-for-grabs as private sector currency.
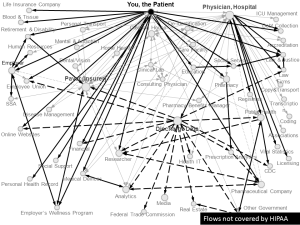
HIPAA, the purview of the Department of Health and Human Services, is part of a privacy patchwork quilt with plenty of holes that doesn’t protect peoples’ health data, writ large, as envisioned in the go-go world of Health Datapalooza. Ask Latanya Sweeney of Harvard’s Data Privacy Lab, and she’ll tell you: lots of peoples’ health data – particularly consumer-generated data left on social networks, created through self-tracking devices and mobile apps – fall through the cracks. Here’s Sweeney’s drawing showing the flows of “You, the Patient.”
An Office of the Health Consumer (or pick your favorite noun for The Person at the Center the Health System) would provide a strategic focus for all of the other “Offices” at ONC to work for. Quality and Safety for “whom?” Care Transformation for “whom?” Clinical Quality for “whom?”
ONC is seen as the most-followed government agency in the #HealthData community, shown in the blue diagram developed by WCG and the Health Data Consortium. Where else can a U.S. health consumer turn to inform, engage, inspire, advocate for them when it comes to health data access and rights?




 I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for