 Nations throughout the world are challenged by the cost of health care: from Brazil to China, India to the Philippines, and especially in the U.S., people are morphing into health care consumers. Three categories of health spending in the bulls-eye of countries’ Departments of Health are prescription drugs, and the costs of care in hospitals and doctors’ offices.
Nations throughout the world are challenged by the cost of health care: from Brazil to China, India to the Philippines, and especially in the U.S., people are morphing into health care consumers. Three categories of health spending in the bulls-eye of countries’ Departments of Health are prescription drugs, and the costs of care in hospitals and doctors’ offices.
In the U.S., one tactic for cost containment in health is “switching” certain prescription drugs to over-the-counter products – those deemed to be efficacious and safe for patients to take without seeking treatment from a doctor.
Over-the-counter drugs (OTCs) are available every day to consumers in grocery stores, pharmacies, and Big Box stores. OTCs already play a big role in health consumers’ personal health ecosystems: how people in the U.S. manage health where they live, work, play and learn the 362 days a year they aren’t in a doctor’s office. 
Last month, I attended a briefing meeting held by Pfizer to discuss the impact on health costs of expanding consumer access to over-the-counter drugs switched from prescription status. In kicking off the discussion, Mark Gelbert, who leads Global R&D in Pfizer’s Consumer Healthcare business, shared a personal OTC story. When he was a young boy, he spent a weekend with family friends who cared for him while his parents took a brief trip away from home. Gelbert described himself as a “highly allergic kid” with seasonal allergies: when symptoms hit him, his itchy eyes would swell up. Hours after his parents departed that May weekend, young Mark could barely open his eyes. The caretaking neighbors asked him: “where is your medicine?” Mark replied: it was in his house, locked. His younger brother had to crawl through a window and retrieve the medications [a scene straight out of Leave It To Beaver called Child Care.] 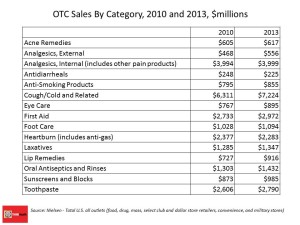
Back then, patients received allergy medicines via prescription. Today, the neighbors could have driven to a local pharmacy or supermarket to pick up Allegra, Claritin, Dimetapp (the OTC version of what I took for allergies as a kid, Dimetane via Rx), Zyrtec, or any number of branded and private label OTCs for the allergy category – which was worth about $7.2 bn in U.S. sales in 2013, making cough/cold/allergy the largest single OTC category. This scenario illustrates that OTC drugs today give consumers access, choice, and convenience.
Consider that 2014 marks the 30th anniversary of Advil. If you sustain a sports injury, experience a headache, or suffer from cramps, you can pick up Advil on a trip to the grocery store. Twenty years ago, if you had heartburn, your only OTC choice was Maalox or Tums, Gelbert said. If you had a yeast infection, you had to see your OB/GYN and get a prescription; today, a woman can buy Monistat in the women’s health aisle of the store.
“The consumer has the ability, knowledge and tools to handle more than a lot [of people] believe they can handle,” Gelbert asserted. This is important because the consumer is more savvy than ever before, and the health care system more complicated and costly than ever before, he continued. Consumers have access to more information, and already take advantage of these resources and tools. [Health Populi notes: 72% of Internet users seek health information online, according to Pew Research].
This is a quiet revolution in health care – self-care, Gelbert concluded. “You can’t go to CVS to get gastric bypass surgery, but you can get a proton pump inhibitor,” he noted.
Health Populi’s Hot Points: Like Mark Gelbert, my youth was marked with serious summer allergies: my mother drove me to the allergist’s office once a week to get an allergy shot to deal with my sensitivities to pollen, mold, and generally speaking, “summer.” The doctor’s prescription for my Dimetane pills were filled at the suburban mom-and-pop pharmacy (open something like 9 am to 5 pm). And all of this was paid-for out-of-pocket by my parents. That was the direct cost, and the time cost was substantial: 40 minutes’ drive-time each way to the doctor’s office for the shot. [I was blessed with a very patient, generous and loving mom.]
Today, the ubiquity of 24-hour pharmacies and stores, and OTC allergy drugs, saves families time and money. As cost and convenience have been driving growth of urgent care in the U.S., these factors will also increase consumer demand for OTCs. In a sense, OTCs are a form of urgent-care-in-the-home-medicine-cabinet).
An artifact of the post-Recession economy is a restructured, re-oriented consumer, globally, embracing more self-service and independence from institutions. In Eyes Wide Open, Wallet Half Shut, Ogilvy says, “Self reliance is the new insurance policy.” While Ogilvy wasn’t speaking to health insurance per se, the point is clear: people are going DIY in daily life. Sustainability is the new happiness, Ogilvy learned in its post-Recession poll. Consumers are looking to organizations that can help:
- Save me money
- Keep me healthy
- Inspire creativity
- Conserve resources.
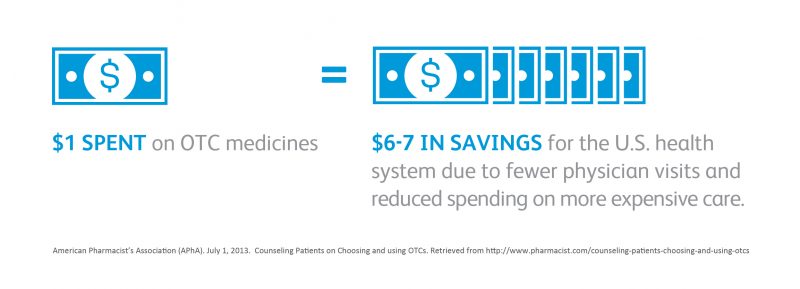
OTCs, when deemed to be safe and useful, can accomplish all 4 of these post-Recession objectives. OTCs can help people save money (especially when used as part of a medical spending account with pre-tax dollars, or as a substitute to a prescription drug); they can help keep people healthy, they inspire creativity in the DIY-sense of self-care being part of a healthy lifestyle; and they conserve resources – time, personal energy, and gas mileage, among other factors.
The American College of Preventive Medicine (ACPM) published a report which delineated benefits and drawbacks of OTCs. Benefits cited included direct, rapid access to effective medicines; wide availability; decreased healthcare system utilization (fewer physician visits, lower healthcare system costs); and, allowing individuals to be in charge of their own health. On the other hand, the ACPM pointed out risks associated with OTC use, such as incorrect self-diagnosis delaying diagnosis and treatment of serious illnesses (delay in seeking advice from a healthcare professional); increased risk of drug-drug interactions; increased risk of adverse events when not used appropriately; potential for misuse and abuse.
The growth of consumer-directed health plans, combined with consumers flexing their DIY-muscles across all aspects of life (from travel planning to financial management and accessing entertainment via streaming media), align incentives between consumers and health providers for patient engagement. OTCs already play a major role in self-care for people managing allergies, pain, heartburn and gut issues, shown in the chart.
The more primary care doctors can arm patients with self-care tools, the better physicians can manage in the value-based health care era of payment increasingly based on patient outcomes, satisfaction, and rational resource use. The opportunity for health care providers is to engage people in conversations for shared decision-making and consumer empowerment. Such conversations are recommended in the ACPM’s OTC report.
Think of this as collaborative health care, featuring greater consumer health engagement that can drive outcomes, benefit both patients and providers, and lower costs to the health care ecosystem.




 Thank you, Jared Johnson, for including me on the list of the
Thank you, Jared Johnson, for including me on the list of the  I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a