By shifting primary care visits by 5 minutes, moving some administrative tasks and self-care duties to patients, the U.S. could conserve billions of dollars which could extend primary care to underserved people and regions, hire more PCPs, and drive quality and patient satisfaction.
Accenture’s report, Virtual Health: The Untapped Opportunity to Get the Most out of Healthcare, highlights the $10 bn opportunity which translates into conserving thousands of primary care providers. PCPs are in short supply, so virtual care represents a way to conserve precious primary care resources and re-deploy them to their highest-and-best-use.
The analysis looks at three scenarios for extending primary care:
- Shaving a few minutes off of a typical office visit via consumers’ use of sensors, using patient portals for administrative transactions like completing forms before a visit, and following up via video visits where they can be most appropriately done.
- Ongoing patient management using eVisits for people with hypertension.
- Patient self-management for chronic conditions such as diabetes.
While the macro numbers for the U.S. health system total nearly $10 billion under these three scenarios (which represent but a few of the total possibilities for virtual health care), the financial and clinical human resource impact for the enterprise — say, an integrated delivery system — are compelling. Accenture calculates that the 5 minutes saved per visits for these three scenarios in a single health system with 1,800 affiliated or employed PCPs could conserve 320 PCPs, equal to about $63 mm of primary care resource.
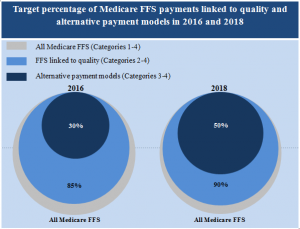 Health Populi’s Hot Points: Virtual health care will underpin hospitals’ and health care providers’ ability to move from getting paid based on the volume of patient visits and procedures to being paid on the basis of value — population health outcomes, individual patient diagnostic bundles, episodes of care, among the various flavors of value-based reimbursement evolving in healthcare in America. Remember that Medicare plans to move 50% of fee-for-service payments into value-based funding by 2018. The time between “now” and “then” will fly, in terms of health systems’ ability to shift Medicare workflows into this Brave New Payment Paradigm.
Health Populi’s Hot Points: Virtual health care will underpin hospitals’ and health care providers’ ability to move from getting paid based on the volume of patient visits and procedures to being paid on the basis of value — population health outcomes, individual patient diagnostic bundles, episodes of care, among the various flavors of value-based reimbursement evolving in healthcare in America. Remember that Medicare plans to move 50% of fee-for-service payments into value-based funding by 2018. The time between “now” and “then” will fly, in terms of health systems’ ability to shift Medicare workflows into this Brave New Payment Paradigm.
Accenture’s report details but three kinds of encounters that can be shifted, in not-too-dramatic ways, toward the virtual visit paradigm. These models emphasize the paradigm that health care will be both digital AND analog — not one nor the other, mutually exclusively. High-tech can marry appropriately and effectively with high-touch. The art of figuring out the best mix can integrate with the science of what’s best for clinical care, based on clinicians’ coming together with each other and with financial and management staff in delivery systems.
We brainstormed this idea in my meet-up with the Group Practice Improvement Network in San Antonio on 15 October 2015, in the context of the new consumer in the value-based health economy. The theme of the event was “What Matters Most.” In our discussion, a representative from a well-known, respected group practice in the Pacific Northwest commented that her organization has brilliant minds working within — a rich trove of intellectual capital that, if deployed for this kind of discussion, can make these value-based delivery scenarios work toward The Triple Aim.
FYI, my firm, THINK-Health, had the pleasure of collaborating on this Accenture analysis.
For more on the impact of virtual healthcare on hospitals, see Accenture’s Dr. Kaveh Safavi’s essay in U.S. News & World Report’s special coverage for the 2015 Hospital of Tomorrow meeting in Washington, DC.




 I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for