 “Consumers expect to have their data available and shareable.”
“Consumers expect to have their data available and shareable.”
Two essays in two issues in the past two weeks of The New England Journal of Medicine point to the importance of patients – people, caregivers, consumers, all — in the morphing “health information economy,” a phrase used in the title of one of the published pieces.
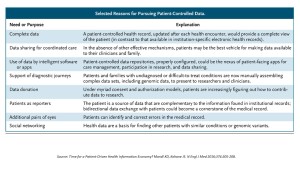
In Time for a Patient-Driven Health Information Economy, Dr. Ken Mandl and Dr. Isaac Kohane, who are both affiliated with the Department of Biomedical Informatics at Harvard, discuss peoples’ growing interest in engaging with their personal health information, noting frustrating barriers to doing so: HIPAA, which can be seen as a lever for engagement but too often serves as an excuse to block patients’ information access; health providers’ concerns about security breaches and data leakage; and, a fragmented technology infrastructure that limits “data liquidity,” the ability for the totality of an individual’s personal health information to move out of their data silos into one convenient, understandable format for the patient. “Where is the easy button?” people wonder, the kind they have from banks, investment companies and airlines? [The authors point to the Blue Button initiative at the VA which has been very useful, but has not gained significant market traction beyond the VA].
But there’s a convergence of factors that can reset the on-ramp and provide traction for people to get their health information, Mandl and Kohane explain. The proliferation of smartphones and apps, the internet cloud, and the growth of value-based payment for health care are driving forces for the new scenario of a patient-driven health economy on the supply side. On a wonkier (hugely important) front, data standards like FHIR and SMART are being deployed within traditionally closed electronic health records systems to enable data liquidity.
On the demand side, people – patients, caregivers – are pressing up to the providers from the grassroots, needing this information so they can take on their mantle as new health consumers. And a growing cadre of switched-on providers are adopting an Open Notes approach to sharing information with patients.
Shared Decision-Making — Finding the Sweet Spot from Dr. Terri Fried of the Yale School of Medicine complements Mandl’s and Kohane’s vision of the patient-driven health information economy. Fried discusses the importance of physicians’ listening to patients’ concerns and values in the process of the clinician-patient shared decision-making process. Too often, clinicians’ approach to weighing therapeutic treatment decisions — say, in dealing with guidelines for treating cancer or heart disease — do not account for patients’ preferences. Yet, she notes, eliciting patient priorities about their own lives can yield quite different choices between therapeutic options. “Clinicians’ recommendations can cause them [patients] to make choices contrary to what they would otherwise prefer,” Fried recognizes.
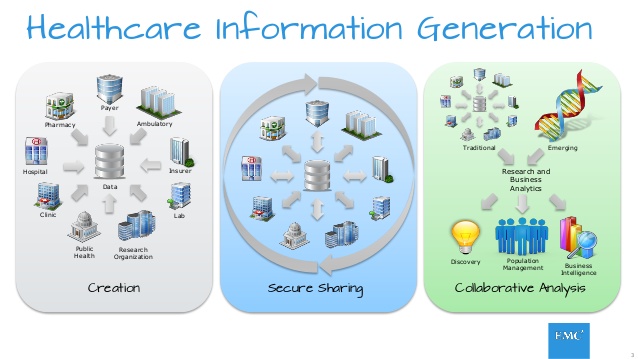
 Health Populi’s Hot Points: The new health consumer is of the genus homo informaticus, whom I’ve called out since learning about from EY’s look into the multi-channel consumer in 2014. EMC;s new latest thought leadership on Information Generation looks into the always-on phenomenon across many vertical markets, including healthcare, as they phrase it, “at the speed of now.”
Health Populi’s Hot Points: The new health consumer is of the genus homo informaticus, whom I’ve called out since learning about from EY’s look into the multi-channel consumer in 2014. EMC;s new latest thought leadership on Information Generation looks into the always-on phenomenon across many vertical markets, including healthcare, as they phrase it, “at the speed of now.”
89% of health providers say technology has changed patient expectations, EMC’s survey found. Most patients want faster access to healthcare services, 47% want personalized experiences, 45% seek 24/7 access and connectivity, and 42% would like access on more devices: here comes homo informaticus to health care, on mobile phones and tablets.
That these two essays on patient-centered information appeared on January 14th and January 21st, 2016, respectively, in the nation’s most prestigious peer-reviewed medical journal – NEJM – attests to the growing embrace of patients by physician leaders like Drs. Mandl, Kohane and Fried. While the private sector is innovating innumerable patient-facing technologies in the forms of portals, personal health records, and mobile apps (which we’ll see next month at #HIMSS16 in Las Vegas), the public sector — regulators and the health IT policy framers — must quickly move to promote and support the transition to true patient-and-person centered health information.




 Thank you, Trey Rawles of @Optum, for including me on
Thank you, Trey Rawles of @Optum, for including me on  I was invited to be a Judge for the upcoming
I was invited to be a Judge for the upcoming  For the past 15 years,
For the past 15 years,