 A special report on patient engagement and digital technology was published this month in the New England Journal of Medicine (NEJM). Based on a survey of doctors and healthcare executives, the research found that clinicians and managers welcome the opportunity to use digital tech — when it makes financial sense.
A special report on patient engagement and digital technology was published this month in the New England Journal of Medicine (NEJM). Based on a survey of doctors and healthcare executives, the research found that clinicians and managers welcome the opportunity to use digital tech — when it makes financial sense.
That conclusion inspired the title of the article, Patient Engagement Survey: Technology Tools Gain Support – But Cost Is a Hurdle. NEJM polled 595 members of the NEJM Catalyst Insights Council, which included healthcare executives and clinicians who deliver healthcare.
Here is NEJM’s scenario on patient-engaging health IT, a Holy Grail of sorts:
“Patient engagement technology tools encourage patients to be accountable for their own health and to identify and curb the behaviors that result in poor health. They form a link between the provider, patient, and third-party information, creating feedback loops, offering insights about disease and disease management, and building support systems. Ideally, patient engagement technology tools fill the gap between patient visits; they could even preclude unnecessary office visis, trips to the ER or hospitalization.”
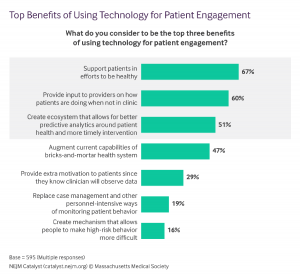
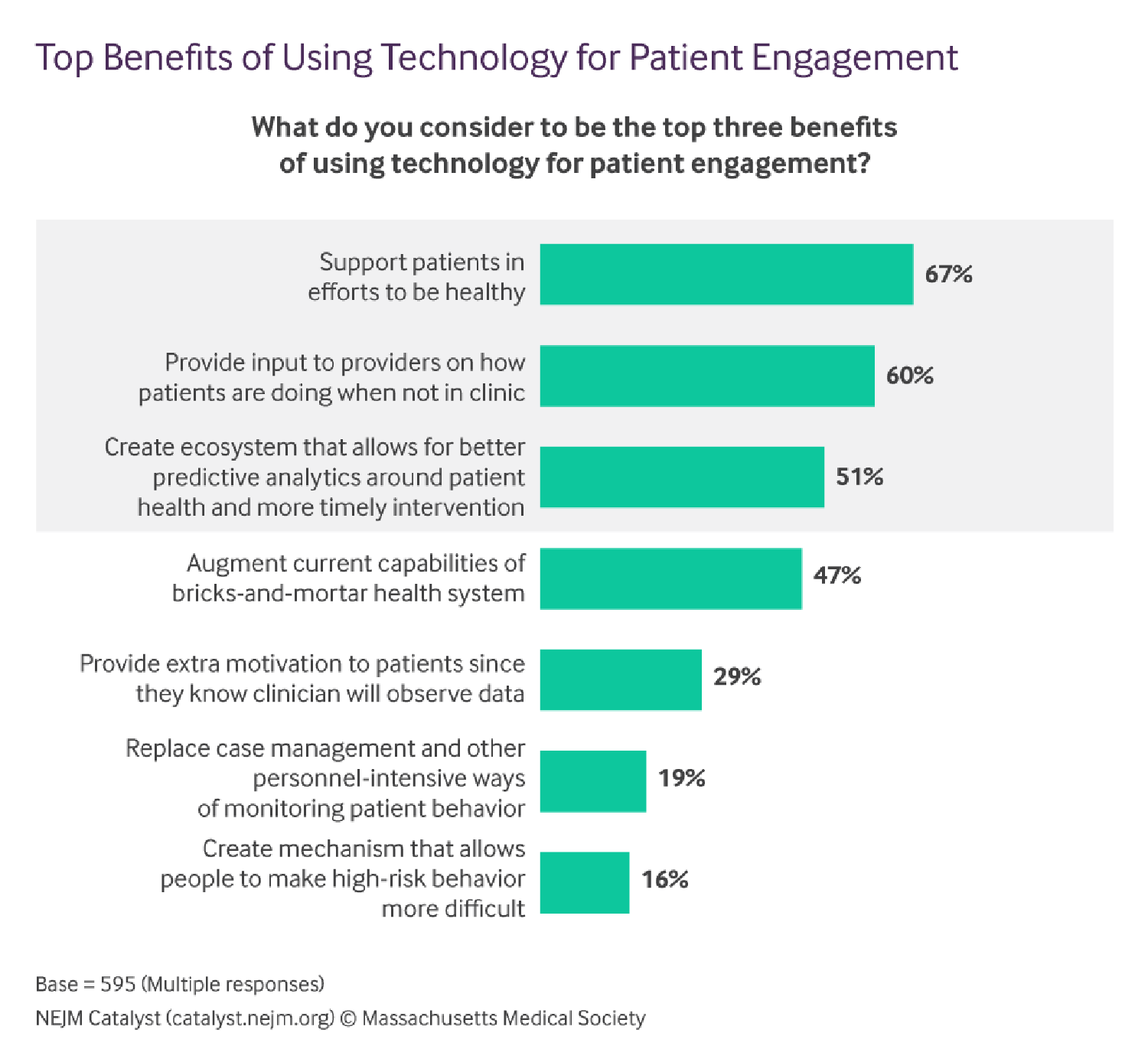
Supporting patients in efforts to be healthy, and providing input to providers on how patients are doing when not in clinic, are the two top benefits of using tech for patient engagement cited by clinicians and health managers. Underneath that top-line are some differences in benefit-perceptions by doctors and execs:
- Executives are keenest on these two issues, as well as creating an ecosystem allowing for better predictive analytics around patient health leading to more timely intervention.
- For clinicians, providing extra motivation to patients (since they know the doctor will observe the data); and, creating a mechanism that allows people to make high-risk behavior more difficult, resonate more than with health executives.
Biometric measurement tools, such as Wi-Fi enabled scales, apps, texting, and wearable technology are all seen as potentially effective technologies to use for engaging patients in their own care.
The top three applications for which patient engagement tools are best suited would be:
- Chronic disease management
- Support for medication adherence
- Fitness tracking
- Readmission prevention.
Mental health and behavioral health tech, and risk behavior mitigation techs, are seen as the least suited for patient engagement.
Not surprisingly, cost is the top barrier preventing widespread adoption of patient engagement technologies: 51% of the survey respondents said if the tech isn’t covered by insurance, it’s a key barrier, followed by 46% of people who said lack of integration is a key barrier, and 45% who pointed to cost to the patient. 37% of the respondents noted that “unclear benefit” would be a top barrier to adopting patient engagement tools. Security ranked lower, with 21% of respondents noting that as a barrier.
To mitigate the cost barrier, 61% of providers and executives agree that payers should cover the cost of patient engagement tools. [Health Populi observation: this could speak to the fact that payers garner financial benefits to patient engagement in that more activated patients yield lower healthcare costs].
Clinicians also don’t know what digital health tools to recommend: 67% of people surveyed say this is the top barrier to “prescribing” digital health tools. The second greatest barrier to recommendation is not knowing tech’s impact on quality outcomes.
Finally, the issue of interoperability ranks high on areas of desired focus for vendors: one-half of clinicians and management say better integration of technology with engagement strategies, integration with clinical workflows, and easier-to-use products are top aspects of digital health tools vendors should address.
Health Populi’s Hot Points: It is encouraging to see a majority of doctors and healthcare executives agree that patient engagement leveraging digital health tools is valuable. The role for patient self-care is a key to driving the Triple Aim: boosting health outcomes, improving health care delivery, and lowering health care costs per patient. Digital health tools, when designed with and for consumer life-flows and values, bridge the gap between time in the doctor’s office a few minutes each year, and time IRL (in real life) the other 364+ days where people live, work, play, pray, and learn.
It is important to note the difference in perceptions of value/benefit between healthcare executives and clinicians: management sees greater value in the ecosystem of data for predictive analytics and timely intervention; doctors see digital health tools’ role in individual patient behavior change to move the needle on individual health outcomes.
This speaks to population health vs. personal health. Digital tools appropriately “prescribed” (recommended) by clinicians can indeed help improve patient health and quality of life. Consider WellDoc, the FDA-approved remote health monitoring device that is prescribe-able and, thus, reimburseable, recently getting FDA approval for marketing a consumer-facing, non-prescription version. This device is used by people with diabetes to help manage health daily and streamline a person’s workflow which, for People with Diabetes, consists of over 2 hours of tasks every day.
Healthcare managers’ look at the emerging era of risk-bearing and Medicare payments based on value and consumer ratings. Digital health tools play roles here, too, at scale beyond the patient N of 1.
“Cost as a hurdle” aren’t such a hurdle in this value-based payment mode. The pace of change toward value from volume will be a prime factor in the adoption of digital tools for patient engagement.




 Thank you FeedSpot for
Thank you FeedSpot for