 The HITECH Act, part of the Stimulus Bill (officially, the 2009 American Recovery and Reinvestment Act, ARRA) invested $35 billion of U.S. taxpayer funds to incentivize health care providers (doctors and hospitals) to acquire and use electronic health record systems (EHRs).
The HITECH Act, part of the Stimulus Bill (officially, the 2009 American Recovery and Reinvestment Act, ARRA) invested $35 billion of U.S. taxpayer funds to incentivize health care providers (doctors and hospitals) to acquire and use electronic health record systems (EHRs).
Most providers have taken advantage of these financial incentives, so that EHRs are now part of mainstream medical practice and workflow among providers.
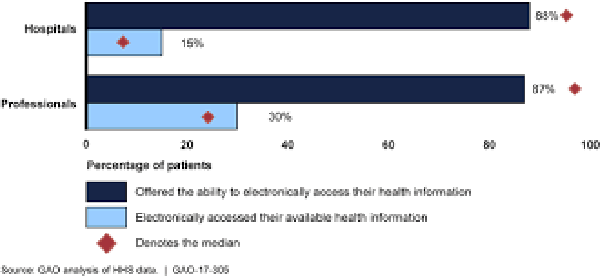
For patients, and particularly those enrolled in the government programs of Medicare and Medicaid, personal access to their personal data in EHRs has been largely elusive. While nearly 9 in 10 doctors and hospitals have offered these patients access to their personal health information via EHR systems, only a fraction of patients have taken advantage of this service.
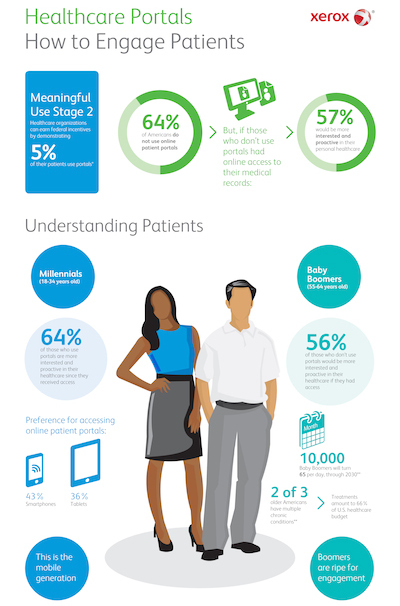
Xerox’s fifth annual electronic health records survey reveals differences between how Millennials and Baby Boomers view healthcare portals.
Only 30% of patients enrolled in Medicare and Medicaid plans have access their personal health data from doctors, and only 15% of these patients have accessed their health data from hospitals, according to the GAO report, Health Information Technology: HHS Should Assess the Effectiveness of Its Efforts to Enhance Patient Access to and Use of Electronic Health Information, written for members of the U.S. Congress.
The bar chart illustrates the GAO’s findings. This report was researched and written as a response to Congressional representatives requesting this information; the list of requesters included Lamar Alexander, Chairman on the Committee of Health, Education, Labor, and Pensions (HELP) in the U.S. Senate; John Thune, Chairman of The Committee on Commerce, Science, and Transportation in the Senate; Michael Enzi, Chairman of the Subcommittee on Primary Health and Retirement Security (in HELP); and Senators Richard Burr and Pat Roberts.
The most common areas of information access included, in order of availability to patients:
- Lab results (by 94% of hospitals, 77% of doctors)
- Allergies (92% of hospitals, 81% of doctors)
- Current medications (92% of hospitals, 82% of doctors)
- Problems and conditions (91% of hospitals, 80% of doctors)
- After-visit summary (85% of hospitals, 77% of doctors)
- Immunization history (82% of hospitals, 67% of doctors),
among others data items with lower levels of availability.
Most providers believe that it’s helpful for patients to, in particular, review their lab values, current meds, allergies, immunization history, clinical history, and after-visit summary. Lower on providers’ perceived value for patient review are radiology images and clinician notes.
Perspectives of patients were also part of the GAO study, which were limited to interviews with 33 patients who were members of the Patients Like Me community. The interviews asked patients about their electronic health information access, challenges they encountered when trying to access their information, benefits they experienced, and improvements they’d like.
The GAO found that older patients may be less likely to electronically access their health information compared with younger patients. Younger patients and people managing chronic conditions are most likely to demand access to their health information.
There are also design issues that patient face when trying to access their personal health information on provider portals, such as technical difficulties and confusing user interfaces.
 Health Populi’s Hot Points: We’re all familiar with the Field of Dreams scenario from the movie about the baseball field, a mystic call to Shoeless Joe Jackson and other players to reunite on the holy ground: “If you build it, he will come,” a mysterious voice whispers. And, eventually, these baseball players do come to play.
Health Populi’s Hot Points: We’re all familiar with the Field of Dreams scenario from the movie about the baseball field, a mystic call to Shoeless Joe Jackson and other players to reunite on the holy ground: “If you build it, he will come,” a mysterious voice whispers. And, eventually, these baseball players do come to play.
This Field of Dreams effect isn’t so responsive when it comes to patients accessing their personal health information, even though most healthcare providers have installed EHR systems. I wrote about Xerox’s (now Conduent’s) fifth annual electronic health records survey back in December 2014, over two years ago, with respect to the Field of Dreams. Xerox’s infographic appears here, noting that most patients were not yet using patient portals, with some generational differences. Among people who hadn’t used a portal, 57% felt they’d be more proactive and engaged in their health care if they did indeed access their health data.
This leads to how to design that baseball field — in this case, the patient portal. In fact, patients don’t tend to like “portals,” per se. People, however, like health, and they are keenly interested in their own lives. So user-centered design must speak to peoples’ real lives, their values, their local social determinants of health, their life-flows…and not repeat online what a clinician’s EHR dashboard looks like.
Good design, like broadband, is emerging as a crucial underpinning for individual and population health. Start by getting smart on my treasured colleague Juhan Sonin’s Design Axioms for health information and engagement linked here. They include:
- Let data scream
- Go as high fidelity with real data as fast as possible
- If Everything is Important, Nothing is
- Real data is truth
- Prototype like crazy
- Design is not a theoretical exercise
- Gantt charts are the illusion of management
- Prototypes aren’t the end; they’re the means
- What Interface?
- Let the ink, UI, and lines disappear
- Reduce the distance between users and content
- Forget the pretty pictures, help people do what they want
- Know thy Code
- You should be as familiar with code as design
- Make Things
- Don’t design it if you don’t know how it’s going to be built.
Perhaps begin with the last, #16: that’s about the user’s (patient’s, person’s, consumer’s, caregiver’s) life flow and values. And eventually, “let data scream!”




 I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for