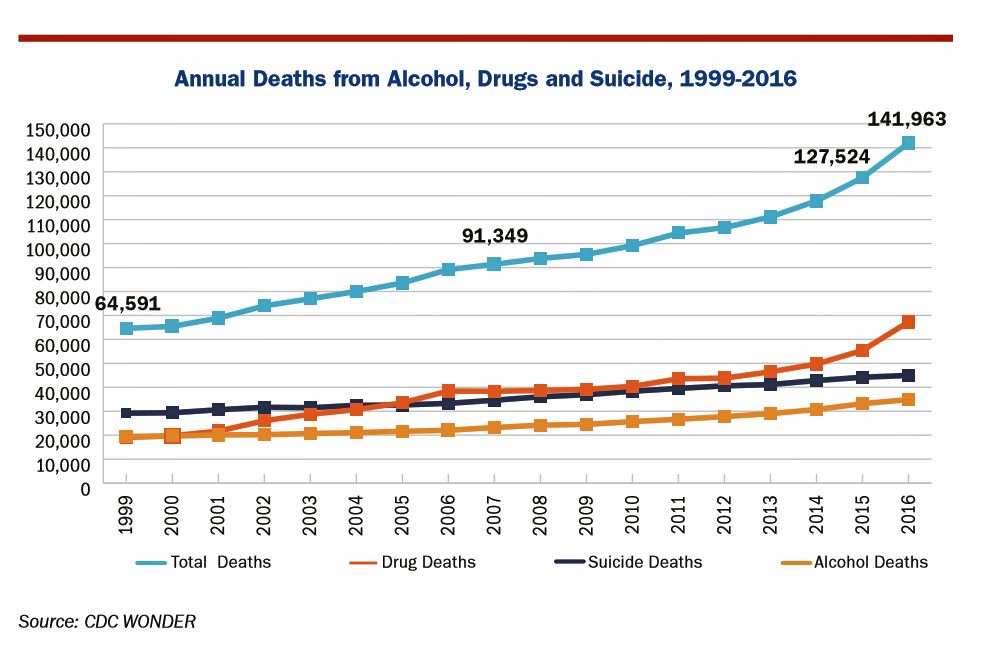
American saw the greatest number of deaths from suicide and alcohol- and drug-induced fatalities was recorded in 2016. That statistic of nearly 142,000 equates to deaths from stroke and exceed the number of deaths among Americans who died in all U.S. wars since 1950, according to Pain in the Nation Update from the Well Being Trust and Trust for America’s Health.
The line graph soberly illustrates the growing tragic public health epidemic of mortality due to preventable causes, those deaths of despair as Anne Case and Sir Angus Deaton have observed in their research into this uniquely all-American phenomenon.
While this is a national challenge, there are regional differences underneath these numbers. The Northeast and Midwestern U.S. states had the biggest increases in alcohol, drug and suicide deaths between 2015 and 2016, and in six states and Washington DC the death rates grew by over 20% — particularly in the Mid-Atlantic region.
The report’s forecast calculates that on the current growth path, deaths from alcohol, drugs and suicide could reach 2 million in 2025 based on a worst-case scenario.
Deaths due to synthetic opioids like fentanyl (100 times more potent than morphine) and carfentanil (10,000 times more potent than morphine) doubled from 2015 to 2016, surpassing mortality due to heroin and prescription opioids. For context, carfentanil is used as a large animal tranquilizer for example in elephants.
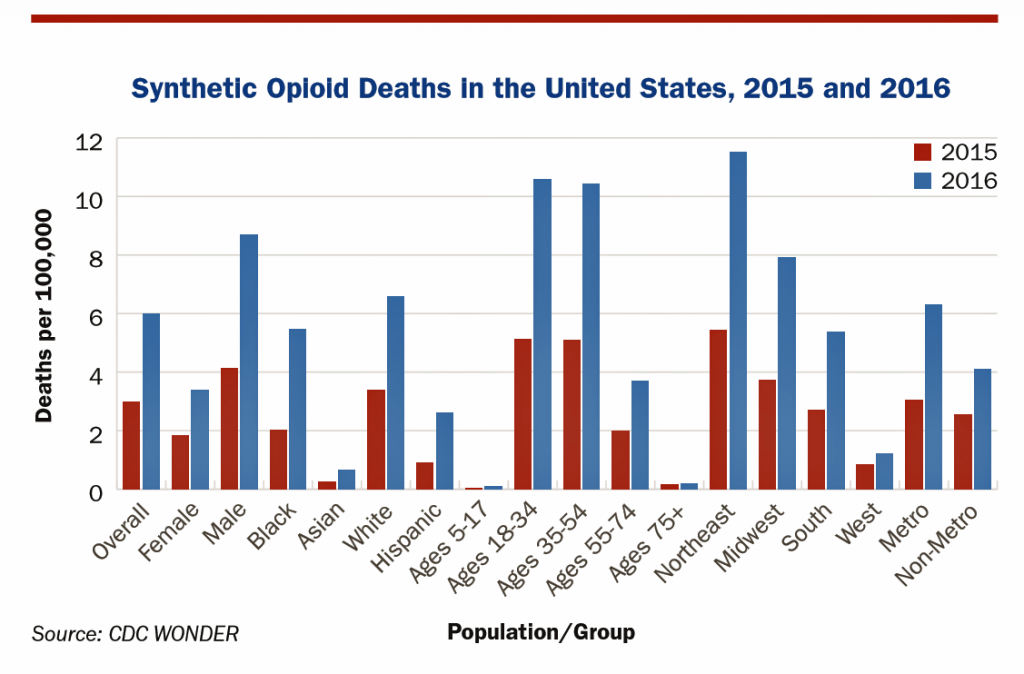 Deaths due to the use of synthetic opioids were most common in the Northeast region of the U.S. (11.5 deaths per 100,000), and in people between 18 and 54 years of age (about 10.5 deaths per 100,000). While the overall deaths-per-100,000 people due to synthetic opioids was 6 per 100,000 in 2016, deaths in the White male population exceed those of women and people of color. Nonetheless, deaths across all demographic groups are increasing due to these “despair” causes. The second chart details the demographic differences in synthetic opioid deaths by gender (far and away male-dominated), race and ethnicity (Whites more than people of color, although significant growth among the Black population), people ages 18 to 54, and the Northeast as the virtual capital of opioid deaths, followed by the Midwest.
Deaths due to the use of synthetic opioids were most common in the Northeast region of the U.S. (11.5 deaths per 100,000), and in people between 18 and 54 years of age (about 10.5 deaths per 100,000). While the overall deaths-per-100,000 people due to synthetic opioids was 6 per 100,000 in 2016, deaths in the White male population exceed those of women and people of color. Nonetheless, deaths across all demographic groups are increasing due to these “despair” causes. The second chart details the demographic differences in synthetic opioid deaths by gender (far and away male-dominated), race and ethnicity (Whites more than people of color, although significant growth among the Black population), people ages 18 to 54, and the Northeast as the virtual capital of opioid deaths, followed by the Midwest.
The impact of these deaths of despair is that U.S. life expectancy fell, again, in 2016. While the country has done a great job at addressing and preventing deaths due to heart disease and cancer, this trend of alcohol, drug and suicide mortality has reversed the positive gains made in the nation…indeed, a Nation in Pain.
The Trust for America’s Health is a non-profit, non-partisan organization focused on public health and healthy communities. The Well Being Trust is a non-profit organization devoted to peoples’ social, spiritual, and mental wellness.
Health Populi’s Hot Points: How to deal with this think-the-unthinkable public and personal health reality?
The Trust detailed a National Resilience Strategy in 2017 with elements of:
- Improving pain management and treatment
- Stemming the opioid crisis with a comprehensive approach integrating responsible prescribing and provider education, public education about safe disposal of unused drugs and proper use, anti-trafficking to stop the flow of these substances, and expanding use of rescue drugs and sterile syringes
- Addressing the impact of opioids on children, targeting multi-generations, services for children and families including grandparents, and expanding support for the foster-care system
- Expanding and modernizing mental health services and treatment in U.S. healthcare
- Lowering excessive alcohol use especially among minors
- Preventing suicides via school and Veterans programs
- Prioritizing prevention and resilient communities
- Rebooting school prevention and mental health programs.
That’s a heavy lift, and one that would require a re-boot, indeed, of how the U.S. allocates dollars and resources from healthcare to health, wellness, prevention, and social services.
Regular readers of Health Populi will tire of my continued reminder that the U.S. allocates an inverse proportion of spending to healthcare versus social care, but in the case of deaths of despair, it’s so obvious a mindset/paradigm to raise. This changing resource allocation is a central tenet of health economics – how to allocate resources in a resource-scarce environment. Will there be political will at the national level in America, and in the healthcare system, to face the underlying causes of the deaths of despair? We will need to hold many truths in our collective hearts, souls, and minds, and work on many parallel tracks, to effectively deal with this American epidemic.




 Thank you FeedSpot for
Thank you FeedSpot for