
“Do no harm” has been the professional and ethical mantra of physicians since the Hippocratic Oath was first uttered by medical students. The origins of that three-word objective probably came out of Hippocrates’ Corpus, which included a few additional words: “to do good or to do no harm.”
The proliferation and evolution of digital technologies in health care have the potential to do good or harm, depending on their application.
Doing good and abstaining from doing harm can engender trust between patients, providers, and other stakeholders in health. Trust has become a key currency in provider/patient/supplier relationships: 94% of health executives say treating customers as partners is important to gain trust, according to the Digital Health Tech Vision 2018 from Accenture.
Accenture’s vision this year is built on five pillars:
- Citizen AI
- Extended Reality
- Data Veracity
- Frictionless Business, and
- The Internet of Thinking.
Together, these factors can bolster personalization and improve consumers’ experience in healthcare, but also have the power to invade, disrupt, and encroach on peoples’ physical and intimate lives in unwelcome ways.

The first trend is Citizen AI. Artificial intelligence, AI, is fast becoming part of the workflow across all industries. AI enables enterprises to take in a lot of data and make sense of it, with the power of better informing decisions. “The more data an AI is given, the better its predictions become,” Accenture notes.
But there’s a data stewardship role that’s crucial when an organization takes in peoples’ personal information: 81% of health executives agree that organizations aren’t prepared to deal with societal and liability issues that AI-based decisions may raise. How to be responsible, equitable, transparent as a good AI citizen? That’s part of “doing no harm” with data in healthcare. And the more good AI behavior will lead to greater adoption and more trust, in a virtuous cycle of data-sharing, data-using, greater productivity, and better health outcomes. That’s why 73% of health executives told Accenture they plan to develop internal ethical standards related to the use of AI to bolster responsible use of patients’ personal health information.
Extended reality here covers three forms of technology “realities:” virtual reality (VR), augmented reality (AR), and extended reality (XR). Together, these three concepts blur lines across physical and simulated, immersive worlds. For healthcare, these platforms enable virtual and telehealth in new ways that transcend bricks-and-mortar settings, getting care and new forms of it to people where they live, work, and play. Accenture classifies XR’s potential in three ways: as,
Distance to people, so “patients can enjoy the removal of distance when it comes to their care,” extending telehealth and virtual care to people regardless of that distance.
Distance to information and insights, bringing patients’ information to clinicians’ fingertips wherever that clinician is located.
Distance to experiences, enabling virtual reality that helps both clinicians and patients gain insights and empathy for healthcare – for example, how the progression of Alzheimer’s disease might feel, or what PTSD seems like. 83% of health executives believe that XR will provide a new foundation for interaction, communication and information, Accenture learned, and most agree that XR will impact every industry over the next five years.
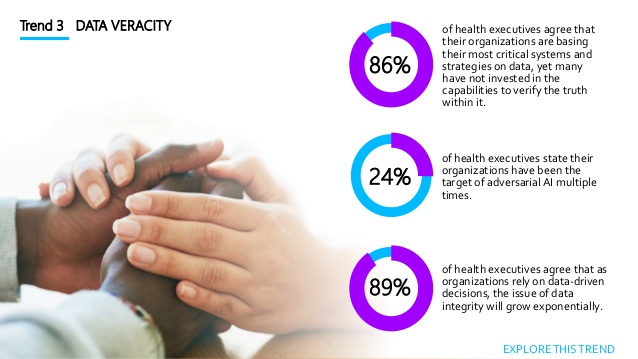 Data veracity speaks to the old adage, “garbage in, garbage out.” The quality of data is more important than its volume of “Big”-ness. “Inaccurate data leads to corrupted insights and skewed decisions,” Accenture warns. One in 4 health care executives say they’ve been the target of AI bad behaviors like falsified location data and bot fraud more than once. Unsurprisingly, then, 3 in 4 health execs aren’t ready to deal with the “impending waves” of corrupted insights as faked data comes into healthcare databases.
Data veracity speaks to the old adage, “garbage in, garbage out.” The quality of data is more important than its volume of “Big”-ness. “Inaccurate data leads to corrupted insights and skewed decisions,” Accenture warns. One in 4 health care executives say they’ve been the target of AI bad behaviors like falsified location data and bot fraud more than once. Unsurprisingly, then, 3 in 4 health execs aren’t ready to deal with the “impending waves” of corrupted insights as faked data comes into healthcare databases.
The solution calls for “data intelligence,” which is a must-do as more artificial intelligence is adopted as a normal course of business. Here, blockchain may be a valuable tactic to underpin cybersecurity and manage risks.
Frictionless business is the vision for streamlining healthcare and lubricating the value-chain for healthcare collaborators. As organizations come together from different parts of the healthcare ecosystem, there’s the potential for the partnerships to become cumbersome and complicated. “Legacy systems weren’t built to support this kind of rapid and robust expansion” we expect to help improve healthcare, so Accenture points to two approaches to deploy that can address friction: blockchain and microservices.
The microservices mindset looks at a program, project, or service in a modular way so that solutions can be created more nimbly. Consider the use of APIs (application programming interfaces) that help to make data more liquid from one application to another.
Why is this trend so important? Because the use of data exchanged between health/care ecosystem partners will increase in the next two years, Accenture learned from 9 in 10 health executives. These technologies will be key for healthcare stakeholders who want to collaborate, cross-business, and more quickly and effectively scale solutions.
 Finally, the Internet of Thinking rounds out Accenture’s five themes in the 2018 Health Tech Vision. Consider the “Internet of Things” morphing to the “T” of “Thinking” (IoTh). In healthcare, this IoTh envisions embedded intelligent tools “everywhere,” and especially “at the edge.” I’m not talking about U2’s outstanding lead guitarist and songwriter, David Howell Evans, but the phenomenon that doing healthcare better requires data accessed where patients and people “are.” Data can be processed and stored at the edge or in the cloud.
Finally, the Internet of Thinking rounds out Accenture’s five themes in the 2018 Health Tech Vision. Consider the “Internet of Things” morphing to the “T” of “Thinking” (IoTh). In healthcare, this IoTh envisions embedded intelligent tools “everywhere,” and especially “at the edge.” I’m not talking about U2’s outstanding lead guitarist and songwriter, David Howell Evans, but the phenomenon that doing healthcare better requires data accessed where patients and people “are.” Data can be processed and stored at the edge or in the cloud.
This concept is important because bandwidth, storage and computational power costs resources, and healthcare is notoriously cost-constrained. But healthcare decisions can be better informed through AI, and AI requires a lot of data to feed the analytics process. Consider “the edge” as a strategic asset will help healthcare organizations engage with greater intelligence, Accenture believes. The report discusses the opportunity-example for an Alexa-like device to alert a person, living and aging at home, of an elevated heart rate (or it could be blood glucose other medical metric) and alert the patient to sit, rest, eat, or phone 9-1-1. “The technology is liberating for the patient, and potentially lifesaving,” Accenture says.
The vast majority of health executives see the important role of computing at the edge, where data is generated.
Health Populi’s Hot Points: Join Dr. Kaveh Safavi, MD, JD, Senior Global Managing Director with Accenture Health, Lisa Suennen, Managing Director for GE Ventures, and me on July 24th when we brainstorm these ideas, live via webcast at 11 am Eastern time, from Accenture studios on Wednesday, July 18, 2018. You can register here on this link.





 Grateful to Gregg Malkary for inviting me to join his podcast
Grateful to Gregg Malkary for inviting me to join his podcast  This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're
This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're