 Electronic health records (EHRs) broaden access to patient data and provide the platform for pushing evidence-based decision support to clinicians at the point-of-care. This promotes optimal care for patients, reduces medical errors, optimizes the use of labor, reduces duplication of tests, and by the way, improves patient outcomes. When done in aggregate across all health providers, a team from McKinsey estimates that $40 billion of costs could be saved in the U.S. health system.
Electronic health records (EHRs) broaden access to patient data and provide the platform for pushing evidence-based decision support to clinicians at the point-of-care. This promotes optimal care for patients, reduces medical errors, optimizes the use of labor, reduces duplication of tests, and by the way, improves patient outcomes. When done in aggregate across all health providers, a team from McKinsey estimates that $40 billion of costs could be saved in the U.S. health system.
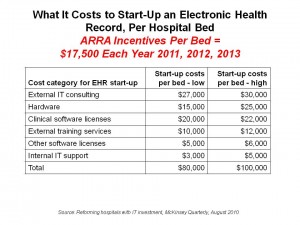
Reforming hospitals with IT investment in the McKinsey Quarterly talks about the American Reinvestment and Recovery Act’s (ARRA) $20+ billion worth of stimulus funding under the HITECH Act and estimates that 80% of existing hospital IT applications will be affected by the regulation. Hospitals will be spending about $120 billion to meet the adoption and meaningful use provisions of the Act. This equates to $80,000 to $100,000 per hospital bed. ARRA incentive payments will cover roughly 20% of this cash outlay, meaning that $60-80K won’t to covered.
But McKinsey says, “Hold on!” There are ways to recoup the spending gap between HITECH incentives and cash-out-of-the-hospitals-budget. McKinsey’s research calculates that optimizing labor, reducing adverse drug events and duplicate tests, and adopting revenue cycle management can help the average hospital save $25,000 to $44,000 per bed each year. That gets to the $40 billion in annual savings when multiplied across all hospital beds in the U.S.
In operational terms, the savings accrue through:
- Managing inpatient beds more efficiently using equipment-scheduling software
- Optimizing the use of clinical equipment
- Determining optimal staffing
- Reducing administrative waste
- Reducing adverse drug reactions through computerized-physician-order-entry (CPOE) which cost $8,000 to $15,000 per bed each year (up to $3 million for a 200 bed hospital)
- Managing the revenue cycle by billing unbilled services, equivalent to 0.4% of hospital services, or $4,000 per bed.
Health Populi’s Hot Points: The McKinsey team rightly points to three critical success factors for maximzing health IT investments that the most wired, effective hospital-adopters have learned: get critical buy-in among clinicians and hospital execs early in the HIT adoption process; ‘radically’ simplify health IT architecture; and, elegantly plan and execute.
It’s the implementation phase in health IT adoption that so often gets short-shrift. McKinsey notes that Canada’s hospital system devoted 30% of its entire budget to change management. That’s a big number, but it’s also where rubber meets road: a capital outlay of $N million is the easy part of HIT adoption. The follow-on implementation resources, both in terms of sheer dollar volume and labor/staffing, along with disruption of clinical workflow, is the hard part. But getting to meaningful use will require no small amount of implementation effort in the form of evangelism, education and training, and ongoing assistance and support.




 Thank you, Jared Johnson, for including me on the list of the
Thank you, Jared Johnson, for including me on the list of the  I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a