There’s been a “clear lack of progress on health equity during the past 25 years in the United States,” asserts a data-rich analysis of trends conducted by two professors/researchers from UCLA’s School of Public Health. The study was published this week in JAMA Network Open.
 The research mashed up several measures of health equity covering the 25 years from 1993 through 2017. The data came out of the Centers for Disease Control and Prevention’s Behavioral Risk Factor Surveillance System looking at trends by race/ethnicity, sex and income across three categories for U.S. adults between 18 and 64 years of age.
The research mashed up several measures of health equity covering the 25 years from 1993 through 2017. The data came out of the Centers for Disease Control and Prevention’s Behavioral Risk Factor Surveillance System looking at trends by race/ethnicity, sex and income across three categories for U.S. adults between 18 and 64 years of age.
The study analyzed the data through two lenses: healthy days and self-reported health. “Healthy days” were defined as the average of physical and mental healthy days over the past 30 days. People scored “general health” on a five-point scale: excellent, very good, good, fair, and poor.
 Four measures of health equity were calculated:
Four measures of health equity were calculated:
- Black-white disparities
- Income disparities
- Health justice (the extent to which health outcomes were correlated with identified social attributes of sex, income and race/ethnicity)
- Health equity metric, which integrated health inequality, health disparities, and mean health into a single metric. The researchers note that calculating this metric was important because traditional health disparity measures
haven’t typically accounted for the experience of particular social groups such as Muslim individuals, LGBTQ individuals, undocumented immigrants, and people identifying with groups of statistically small sizes (e.g., Native American people).
 I’ve clipped one of the figures above, summarizing the scatterpoints and trends for health equity expressed by healthy days.
I’ve clipped one of the figures above, summarizing the scatterpoints and trends for health equity expressed by healthy days.
The table shows the health equity measures and trends over the 25 years. Mean health trended downward between 1993 and 2017, based on healthy days and self-reported health. Income disparities grew and healthy days and self-reported health declined. On the upside, black-white disparities trended downward a bit for both days and health.
Health justice decreased over the 25 years for healthy days, slightly improved between 2012 and 2015, then declined again by 2017. The health justice trend was overall downward.
Based on these 25 years’ of data, the researchers soberly conclude: “the overall pattern is one of stagnation mixed with unambiguous decline.”
Health Populi’s Hot Points: Growing income disparities in wealthy countries around the world correlate with health disparities, research from the OECD and other organizations has shown.
Within the U.S., we see these income/health disparities as well from U.S. State to State. A study in the April 2019 issue of the journal Demography found that mortality associated with low education varied across states, with most pronounced growth in the South and the Midwestern states.
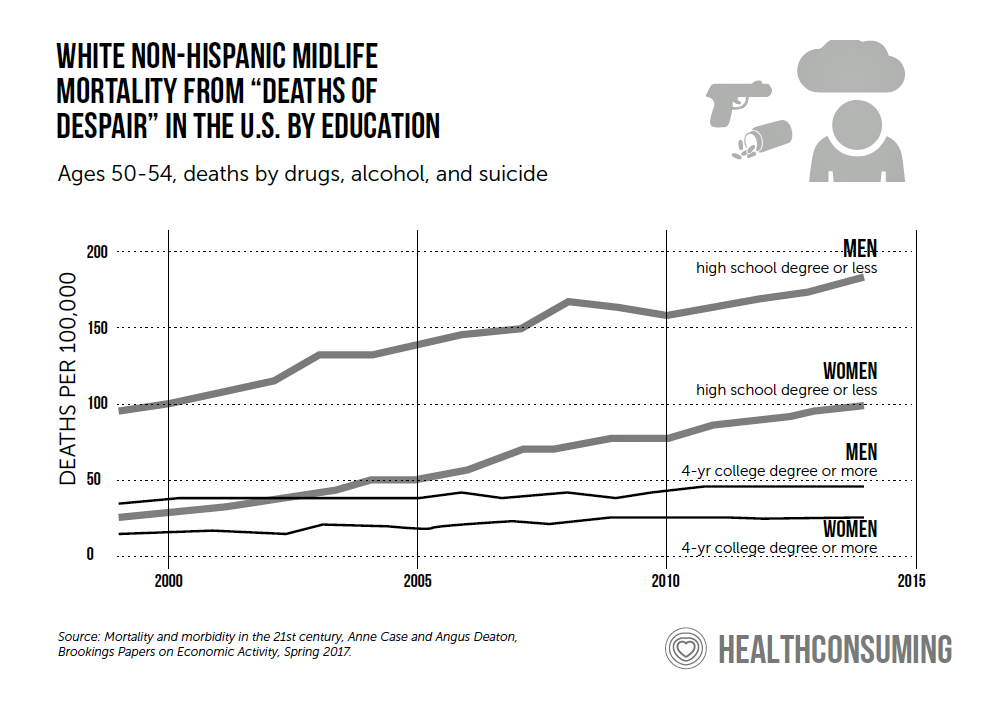
Level of education has been a major factor that Case and Deaton have identified for the so-called “deaths of despair,” which I discuss in my book, HealthConsuming: From Health Consumer to Health Citizen. This is why I argue — as do many other people more focused on social determinants of health as more an investment in human capital development and a productive civil society than a sunk cost.
The last line graph illustrates Case and Deaton’s data point connecting the statistical dots between the relationship between level of education for men and women and mortality due to drugs, alcohol and suicide.
Education is one of the key SDOH’s that can bolster health equity and a more civil, productive society.
The last 25 years have been a sunk cost and exercise in health injustice and health disparities in America. We’ll continue on that downward trajectory in the U.S. unless we re-define what health reform can really mean to the macroeconomy of the nation and the microeconomy of health care. It will require re-investment in education, healthifying food systems, aggressively addressing climate change, and promoting dialogue and inclusion among health citizens.






 Grateful to Gregg Malkary for inviting me to join his podcast
Grateful to Gregg Malkary for inviting me to join his podcast  This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're
This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're