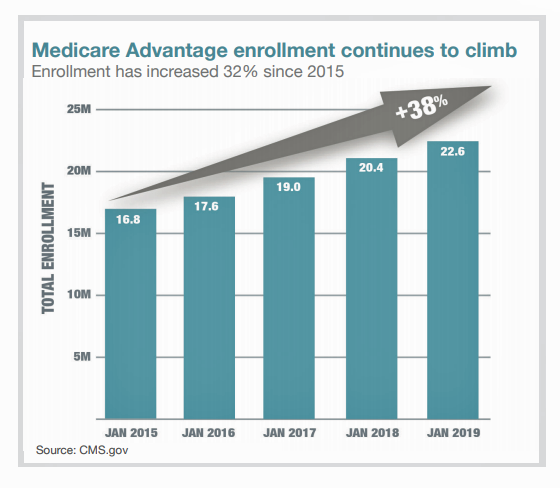
There are over 60 million enrollees in Medicare in 2019, and fully one-third are in Medicare Advantage plans. Medicare is adding 10,000 new beneficiaries every day in the U.S. Medicare Advantage enrollment is fast-growing, shown in the first chart where over 22 million people were in MA plans in January 2019.
Better understanding this group of people will be critical to helping manage a fast-growing health care bill, and growing burden of chronic disease, for America.
To that end, HealthMine conducted a survey among 800 people enrolled in Medicare Advantage plans ag 65 and over with at least one diagnosed chronic condition in April and May 2019. I worked with HealthMine to develop the questionnaire and analyze the results of the study which you can access through the report, A Call for Care That’s Personal, Accessible and Social: HealthMine’s 2019 Survey of Medicare Advantage Beneficiaries.
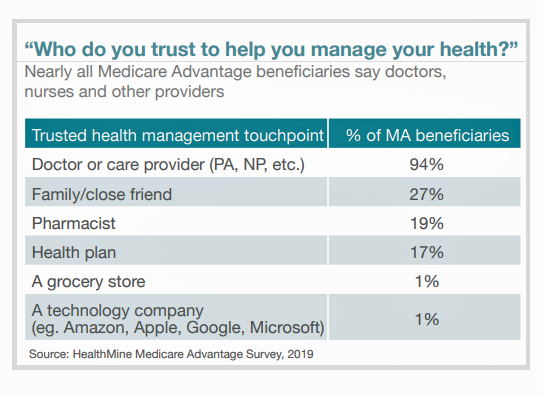
The survey asked MA beneficiaries their views on their health plans, trusted touch-points in their personal health care ecosystems, use of digital technology, social determinants of health, and health care finances.
The most-trusted touch-point among Medicare Advantage members, by far, is the doctor or care provider valued by virtually everyone polled (94%). In distant second place were family and close friends (27%), the pharmacist (19%), and the health plan (17%). Among this population compared to younger people, technology companies were the least favored go-to health touch-point to help manage help by a scant 1% of MA plan members. (See this post to understand how the larger general population views tech companies as trusted health care managers).
 Other top-line findings include:
Other top-line findings include:
- Men enrolled in Medicare Advantage are more digitally engaged than women, noting that
- Younger Medicare beneficiaries are more digitally engaged (connected) than their older peers
- Women enrolled in Medicare spend more money on healthcare than men do, yet women’s life spans are longer and they have less money saved than men as women age
- Medicare Advantage members note an overall dissatisfaction with health care portals
- One of the biggest barriers to older patients not engaging with digital technology for health care is patient’s perceived lack of utility –rooted in a lack of personalization.
And it’s personalization that’s the big opportunity we found in the survey.
Digital platforms are seen by health care providers, plans and pharma as a growing channel for serving up personalized health services. Health care organizations, whether hospitals, health plans and pharma companies, are all quickly working to develop digital health tools to better engage people in health. The patient portal is one such example.
We characterized Medicare beneficiaries as “digital immigrants,” building on the research of Marc Prensky in his seminal essay, Digital Natives, Digital Immigrants. As digital immigrants, older people are, in the words of Prensky’s 2001 observation, “now in the process of learning a new language.” That is, through a 2019 consumer health care tech lens, learning how to sign up for Medicare Part D online, download and use mobile health apps, understand privacy regulations like HIPAA or GINA, and emailing a physician on a patient portal.
For most HealthMine MA plan respondents, portals aren’t viewed as very helpful at all. Only one-third of MA beneficiaries regularly accessed a health portal, we learned. But 51% of these plan members would like to engage digitally with their plan, with marked differences between younger MA members versus older people: 58% of people 65-70 would like to digitally engage compared with 45% of people 76 and older. And men, more than women, would prefer to be digitally engaged, with more women keener on using a phone versus men.
The report explains some of this resistance in the context of important research conducted by the University of Michigan National Poll on Healthy Aging and other sources. It’s complicated, but getting to the core issues which can be a mix of information privacy and security concerns, tech-intimidation and accessibility are all in play.
Do take a look at the report to learn what we found, and how these findings can inform your own plans to serve older peoples’ health in America.
 Health Populi’s Hot Points: Health plans serving Medicare beneficiaries could do better in supporting patients for their health, the third bar chart tells us. Over half of these consumers aren’t sure that their health plan knows the actual status of their health, with fully 1 in 4 people saying, “no, the health plan doesn’t know.”
Health Populi’s Hot Points: Health plans serving Medicare beneficiaries could do better in supporting patients for their health, the third bar chart tells us. Over half of these consumers aren’t sure that their health plan knows the actual status of their health, with fully 1 in 4 people saying, “no, the health plan doesn’t know.”
To personalize health to these Ns of 1 health consumers, it’s not enough to serve up a patient portal that’s generic and not rooted in research conducted among “beneficiaries” — the root word of which is “benefit.” In the continued Field of Dreams that too many health care tech projects fall into, we build shiny new things….and the people just don’t come.
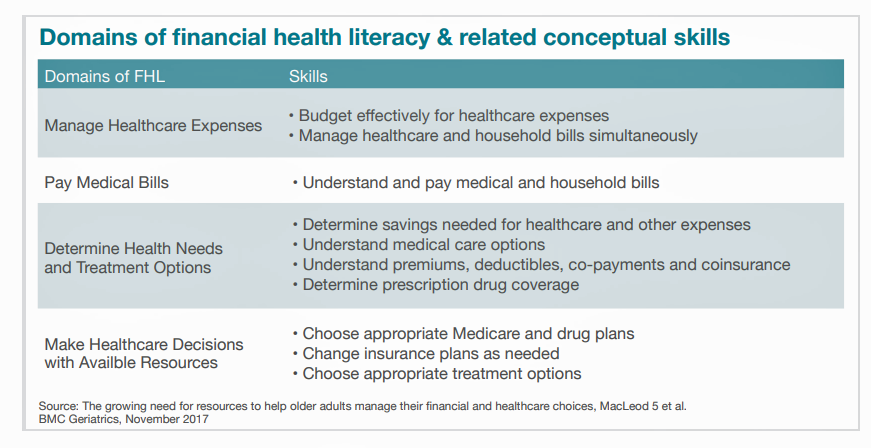 This last chart on the domains of health literacy represents a useful list of some of the underlying findings we learned from the HealthMine study. Health literacy, writ large, doesn’t just deal with knowing when, how and how many pills to take in a day. That’s certainly one form of health-care literacy that can drive good medication adherence and bolster clinical outcomes.
This last chart on the domains of health literacy represents a useful list of some of the underlying findings we learned from the HealthMine study. Health literacy, writ large, doesn’t just deal with knowing when, how and how many pills to take in a day. That’s certainly one form of health-care literacy that can drive good medication adherence and bolster clinical outcomes.
But wait! There’s more! Because patients, and in this instance enrollees in Medicare Advantage plans managing at least one chronic condition, have many other layers of challenges to the health literacy onion. There’s financial health literacy, requiring transparency that’s relevant to “my” costs, and please ma’am, I’d like those in advance of my visit or procedure. Then there’s digital literacy, like teaching me how to access a patient portal and how to use it. We know from research conducted by the California HealthCare Foundation that once frailer, older, and less educated people are actually shown how to access and use online personal health records, people tend to ask more questions and become more engaged in their health care. That form of literacy helps to bolster health outcomes, too.
The call-to-action at the conclusion of the paper is to support patients’ personal risk-management — and that is across the board in terms that patients-as-people define: for my health, my financial well-being, and my social connectivity and unique values.




 Thank you FeedSpot for
Thank you FeedSpot for