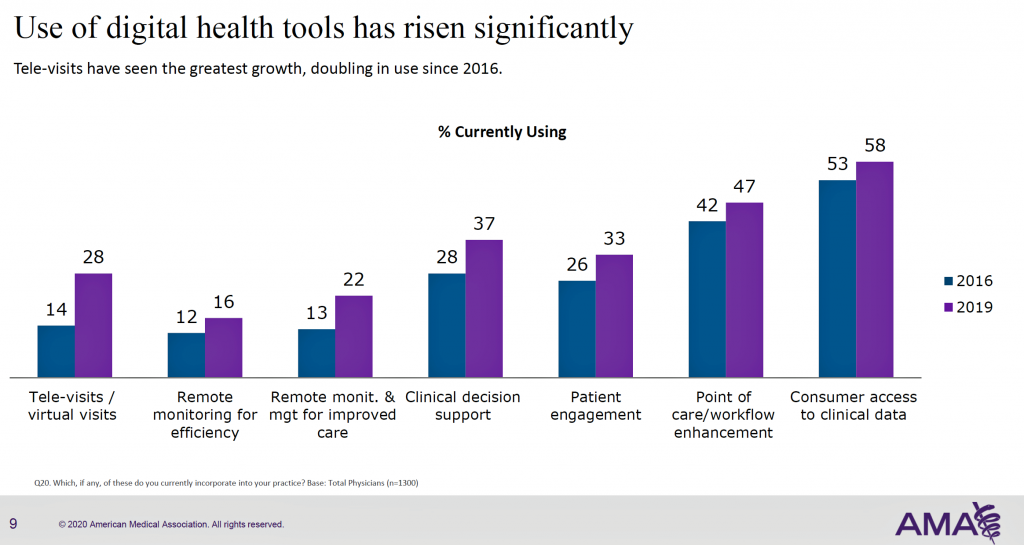
More U.S. doctors are using digital health tools in patient care, with quickening adoption of telehealth and remote monitoring technology, according to a study from the American Medical Association (AMA).
This survey, conducted in 2019 among 1,359 U.S. physicians, follows up AMA’s research conducted in 2016 and largely reflects the original questionnaire to be able to understand real changes among doctors’ use of tech in practice.
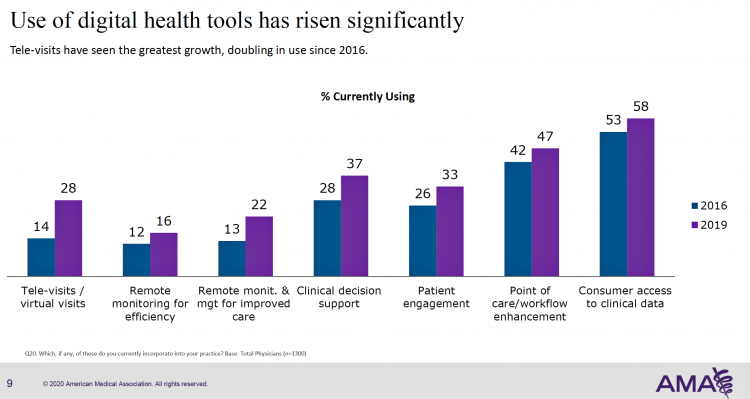
As part of this rigorous study design, AMA used particular definitions for the seven tools the study gauged: remote monitoring for efficiency, remote monitoring and management for improved care, clinical decision support, patient engagement, tele-visits/virtual visits, point of care/workflow enhancement, and consumer access to clinical data.
 For example, “patient engagement” tools were defined as, “solutions to promote patient wellness and active participation in their care for chronic diseases,” e.g., adherence to treatment regimens. Note that “remote monitoring” was split into two types: “for efficiency,” defined as, “smart versions of common clinical devices such as thermometers, blood pressure cuffs, and scales that automatically record readings in the patient record so you do not have to type it;” and, remote monitoring “for improved care,” defined as, “Apps and devices for use by chronic disease patients for daily measurement of vital signs such as weight, blood pressure, blood glucose, etc. Readings are visible to patients and transmitted to the physician’s office. Alerts are generated as appropriate for missing or out of range readings.”
For example, “patient engagement” tools were defined as, “solutions to promote patient wellness and active participation in their care for chronic diseases,” e.g., adherence to treatment regimens. Note that “remote monitoring” was split into two types: “for efficiency,” defined as, “smart versions of common clinical devices such as thermometers, blood pressure cuffs, and scales that automatically record readings in the patient record so you do not have to type it;” and, remote monitoring “for improved care,” defined as, “Apps and devices for use by chronic disease patients for daily measurement of vital signs such as weight, blood pressure, blood glucose, etc. Readings are visible to patients and transmitted to the physician’s office. Alerts are generated as appropriate for missing or out of range readings.”
 The key findings on changes from 2016 to 2019 were:
The key findings on changes from 2016 to 2019 were:
- An increase in the number of physicians seeing an advantage in using digital tools, even among physicians 50 years and older
- Adoption of digital tools has grown across physicians of all ages, specialty, and gender across all technologies studied
- The largest positive change in adoption was seen in telehealth and remote monitoring, and
- Awareness of emerging tech’s like artificial intelligence is relatively high, with adoption low.
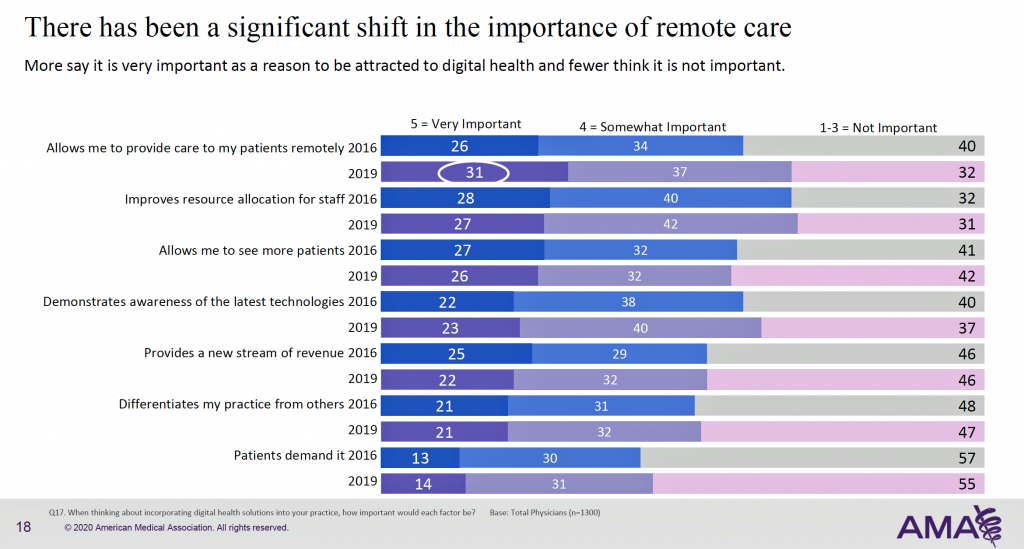
The rise of remote care is explored in the second chart. The important aspects of that is to provide care outside of bricks-and-mortar physician offices, to improve resource allocation, to demonstrate awareness of new technology, and to allow physicians to see more patients, among other underlying adoption drivers. Looking past 2020, we can also expect greater physician use of telehealth and remote care tech, based on a forward-looking question in the poll.
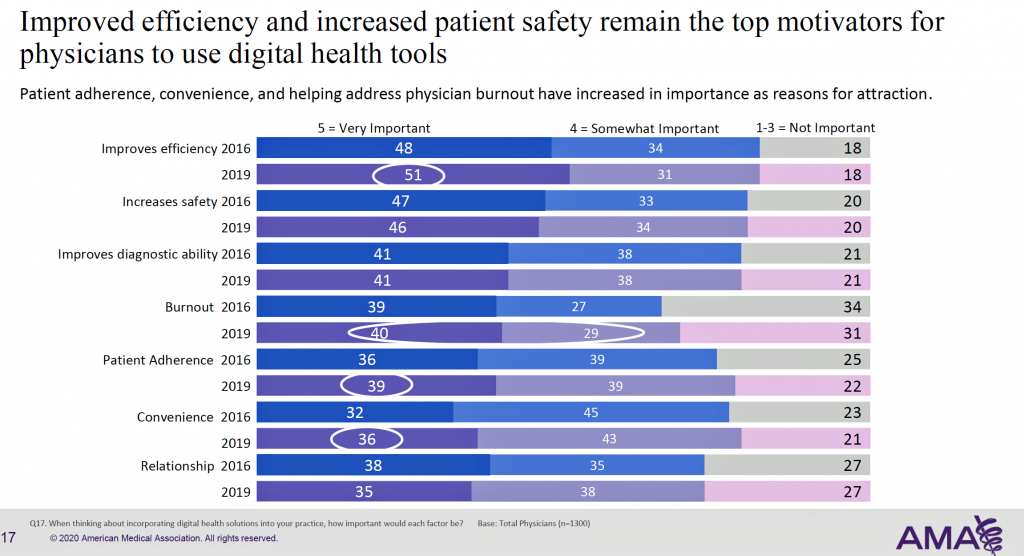
 Health Populi’s Hot Points: What’s underneath the immediate and near-term growth of telehealth and remote care modalities? The top factors supporting adoption were improving efficiency, safety, and diagnostic ability. But look further down this third chart, and you find important patient-facing factors — convenience and patient adherence. And interestingly, the “relationship” isn’t compromised by these “arms-length” care technologies, as 73% of physicians said these tools would be important reasons to use them.
Health Populi’s Hot Points: What’s underneath the immediate and near-term growth of telehealth and remote care modalities? The top factors supporting adoption were improving efficiency, safety, and diagnostic ability. But look further down this third chart, and you find important patient-facing factors — convenience and patient adherence. And interestingly, the “relationship” isn’t compromised by these “arms-length” care technologies, as 73% of physicians said these tools would be important reasons to use them.
Convenience, adherence, and relationship — these are areas that patients value, and physicians see the role of tech in bolstering these features.
I hearken back to a favorite column from JAMA published in 2015 but retaining its relevance ongoing: Value-Based Payments Require Valuing What Matters to Patients. It’s clear that physicians in this AMA study are now living and working in a more value-based payment environment, varying from geography to geography. But the overall ethos is to do more with less, provide quality care, and please patients on that journey. This is the new retail health, with the patient as payor and consumer, and clinicians getting on-board.




 Thank you, Jared Johnson, for including me on the list of the
Thank you, Jared Johnson, for including me on the list of the  I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a