“The COVID-19 pandemic…has highlighted like never before the pitfalls of paying for healthcare based on the number of patients seen and services rendered,” a Modern Healthcare article asserted in mid-June 2020.
 In other words, the U.S. health care financing regime of volume-based payment didn’t fare well as millions of patients postponed or cancelled procedures and visits for fear of contracting the virus in the halls, offices and clinics of hospitals and doctor’s offices.
In other words, the U.S. health care financing regime of volume-based payment didn’t fare well as millions of patients postponed or cancelled procedures and visits for fear of contracting the virus in the halls, offices and clinics of hospitals and doctor’s offices.
“Just imagine if you were 100% fee-for-service,” commented Dr. Fuad Sheriff, a primary care physician whose practice is based on capitated payments. “You would have been dead meat.”
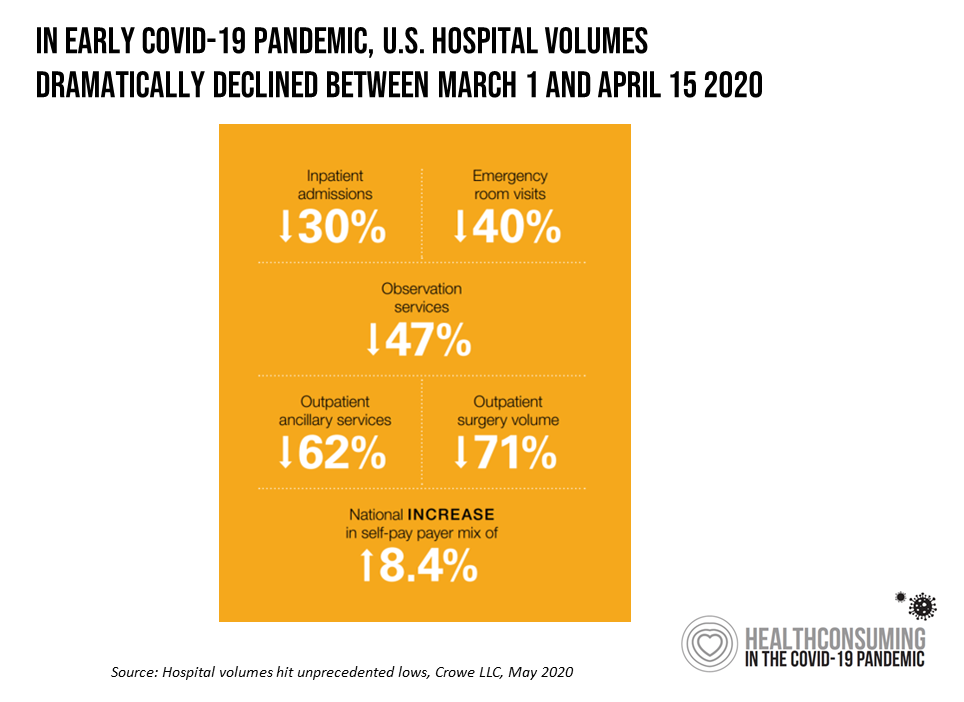
Crowe LLC estimated that U.S. hospitals were losing $1.4 billion a day in March 2020 based on declining patient volumes. The title of their analysis, Hospital volumes hit unprecedented lows, is subtitled, “revenue losses mean long recovery ahead.” This $1.4 billion is an underestimate because it does not include health systems operating in New York City and San Francisco. Nor does the number include the “equally dramatic decline in physician visits,” Crowe comments.
Value must be baked into health care financing as the nation wrestles through economic downturn and, at the same time, the pandemic’s challenges to both the health care system and societal needs
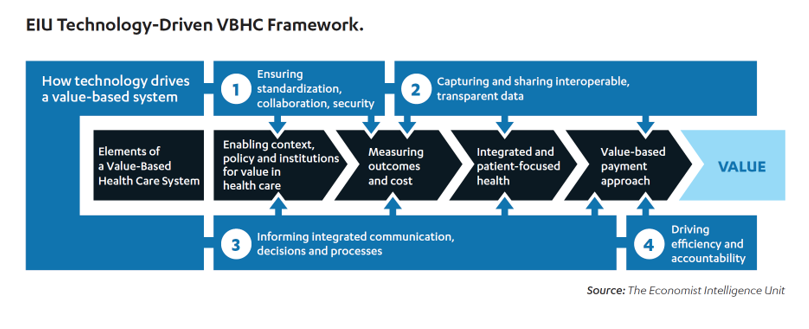 The Consumer Technology Association (CTA) collaborated with The Economist Intelligence Unit (EIU) on the research report, Reinvigorating Value-Based Health Care: Exploring the Role of Technology Innovation.
The Consumer Technology Association (CTA) collaborated with The Economist Intelligence Unit (EIU) on the research report, Reinvigorating Value-Based Health Care: Exploring the Role of Technology Innovation.
EIU defines value-based health care (VBHC) as, “the creation of a health system that explicitly prioritizes health outcomes that matter to patients, relative to the costs of achieving those outcomes.” Such a system depends on a technology infrastructure, tools and processes that enable the delivery of quality, effective and enchanting care.
The EIU VBHC framework addresses four aspects of how technology can underpin value-based care:
- Ensuring standardization
- Capturing and sharing interoperable and transparent data
- Informing integrated communication, decisions, and processes
- Driving efficiency and accountability.
 To gain insights into the framework and promise of VBHC, EIU interviewed 152 respondents for the primary research, including 50 primary care physicians and 50 specialists, 20 health plan executives, and 30 health care administrators.
To gain insights into the framework and promise of VBHC, EIU interviewed 152 respondents for the primary research, including 50 primary care physicians and 50 specialists, 20 health plan executives, and 30 health care administrators.
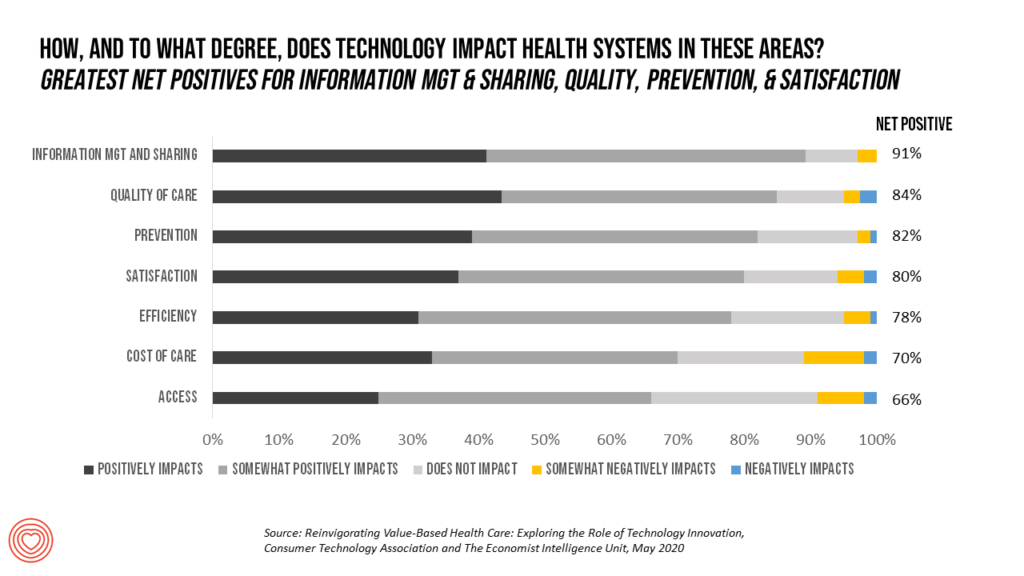
CTA asked these health care executives and clinicians how, and to what degree, did technology impact health systems across seven areas? The results of this question are shown in this bar chart, which I’ve reorganized to tally net positive responses in percent of total respondents.
The top areas garnering greatest net positive responses for technology impacts were information management and sharing; quality of care; prevention; and satisfaction, closely followed by efficiency.
Nine in ten of the respondents cited “information management and sharing.” The implementation of electronic health records, spurred on by the HITECH Act which was embedded in the 2009 American Recovery and Reinvestment Act (aka the Stimulus Bill) resulted in lots of EHRs deployed in hospitals and doctor’s offices, with huge gaps in interoperability and data liquidity.
By now, this gap has been well-recognized, both in terms of work-flow and productivity as well as management’s ability to “manage what we measure.” Both of these EHR implementation deficits have led to learning, which this 91% rate represents.
The COVID-19 pandemic has also taught clinicians and health care administrators about the value of data at the ready. A comment from one of the study respondents colors this in: “You can’t implement VBHC without real-world data, because that is the information needed to understand outcomes and costs, reduce low-value care, build solutions that measurably enhance value, and construct value-based payment models. VBHC starts and ends with outcomes,” explained Jason Arora, Medtronic’s Director of Value-Based Healthcare for Latin America.
 Health Populi’s Hot Points: With the coronavirus pandemic’s Great Lockdown and the shock of the economic shut-down, the U.S. entered a recession that is eroding the nation’s tax base for both business and workers payments into the country’s coffers in and beyond 2020.
Health Populi’s Hot Points: With the coronavirus pandemic’s Great Lockdown and the shock of the economic shut-down, the U.S. entered a recession that is eroding the nation’s tax base for both business and workers payments into the country’s coffers in and beyond 2020.
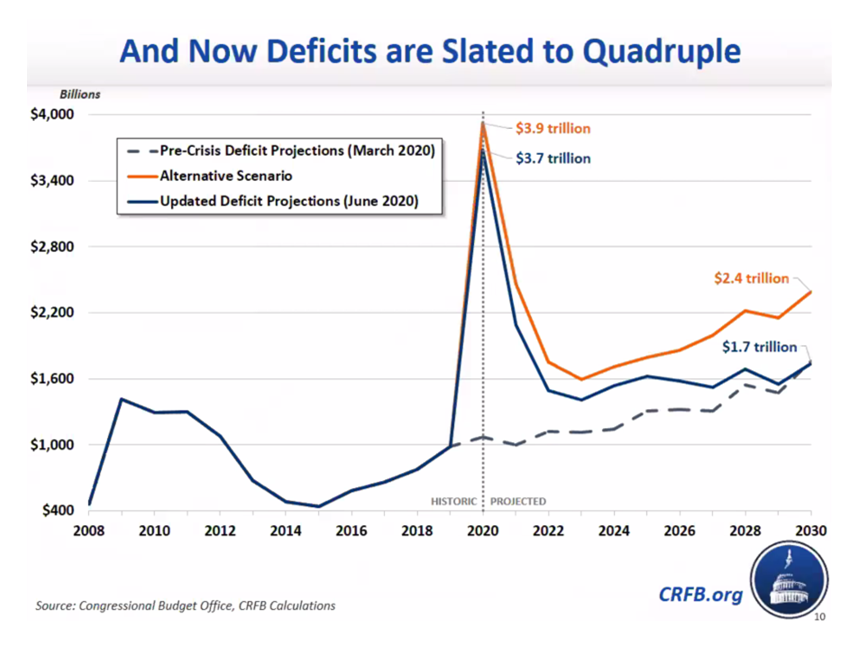
The Congressional Budget Office published an update to the U.S. economic outlook for 2020 to 2030 on July 1, 2020. The most jarring statistic in the report is dramatically illustrated by this line chart, clearly showing budget deficits will take a sharp upturn, a nearly vertical line northward, to sky-high levels well beyond CBO’s pre-crisis deficit projection from March 2020 shown in the dotted line. That number was just over $1 trillion for the year.
The updated projection, considering COVID-19’s economic impact, is at least $3.7 trillion.
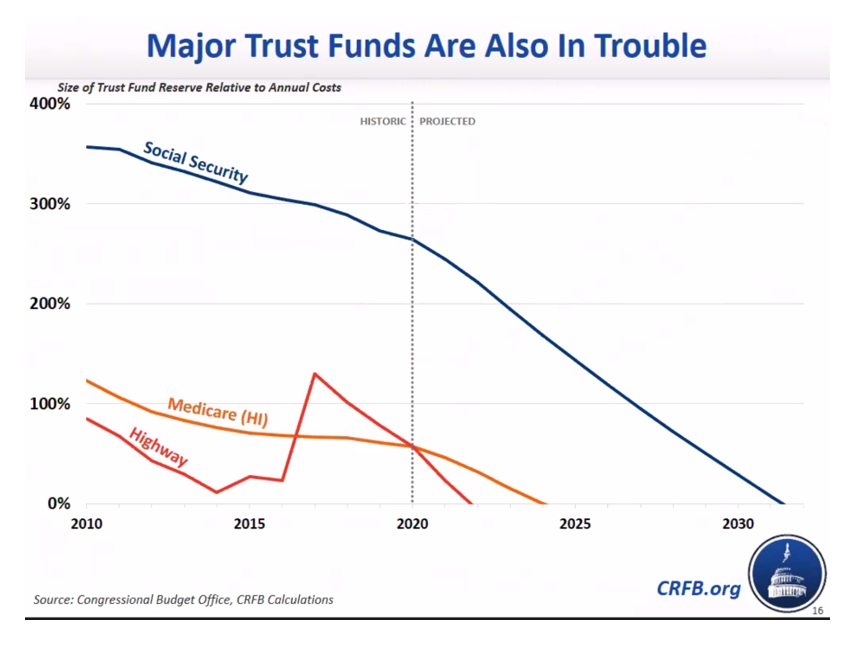
For health care, the data portrayed in the next chart will be concerning: the Medicare and Social Security Trust Funds are expected to hit “zero” (the X-access) by 2025 and just after 2030, respectively.
The Medicare Trust Fund is financed by payroll taxes, general tax revenue, and the premiums enrollees pay.
 National Health Expenditures are expected to consume 19.7% of the U.S. gross domestic product in 2020, the Centers for Medicare and Medicaid Services calculated. That would be $1 in every $5 of the American economy.
National Health Expenditures are expected to consume 19.7% of the U.S. gross domestic product in 2020, the Centers for Medicare and Medicaid Services calculated. That would be $1 in every $5 of the American economy.
In terms of return-on-investment, we don’t seem to be getting a sound ROI on that huge piece of the U.S. economy allocated to health care: in addition to the health disparities and inequities plaguing American health care outcomes, there’s the opioid epidemic, infant mortality that, in some regions, resembles that of nations generating one-fourth of the U.S. GDP, and — in this moment — the country’s growing COVID-19 caseload and death tally.
Value-based payment in itself can’t address all of these issues. But it can be a pillar for driving greater accountability, transparency, more rational spending, and improved patient outcomes and satisfaction in a health system already exhausted and burning out from the coronavirus and its financial impact.





 Thank you, Jared Johnson, for including me on the list of the
Thank you, Jared Johnson, for including me on the list of the  I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a