Most psychologists in the U.S. treated more patients in the first six months of the coronavirus pandemic, shifting their practices to telehealth platforms. These therapists got more referrals and saw fewer cancellations, and one-third treated patients who lived in a different state from their practice site, according to Patients with Depression and Anxiety Surge as Psychologists Respond to the Coronavirus Pandemic from the American Psychological Association (APA).
 For this study, APA polled 1,787 licensed psychologists (both members and non-members in the Association) in the U.S. between late August and early October 2020.
For this study, APA polled 1,787 licensed psychologists (both members and non-members in the Association) in the U.S. between late August and early October 2020.
This year, APA has published four reports on consumers’ mental health in the pandemic. You can find links to them below, just before the Hot Points.
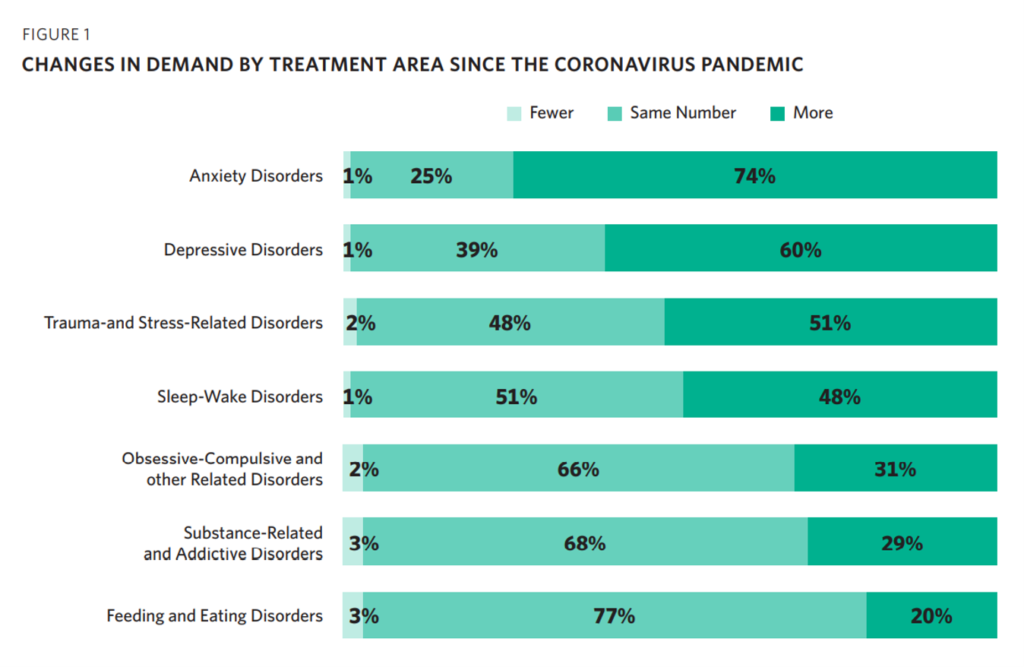
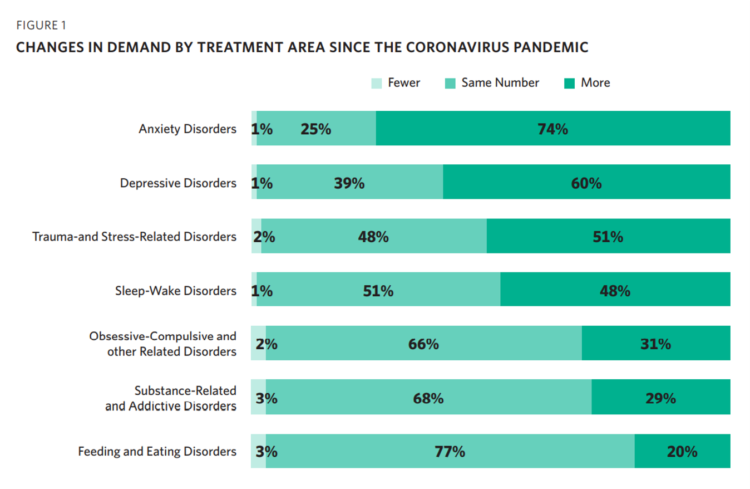
The first chart from the report illustrates that by September 2020, most U.S. psychologists saw growing demand for patients seeking help to deal with anxiety disorders, depressive disorders, and trauma-and stress-related disorders. One-half of psychologists also experienced increased demand for consumers seeking assistance with sleep-wake disorders.
Most psychologists said the level of patients looking to deal with obsessive-compulsive disorders, substance-related and addictive issues, and feeding and eating challenges stayed the same.
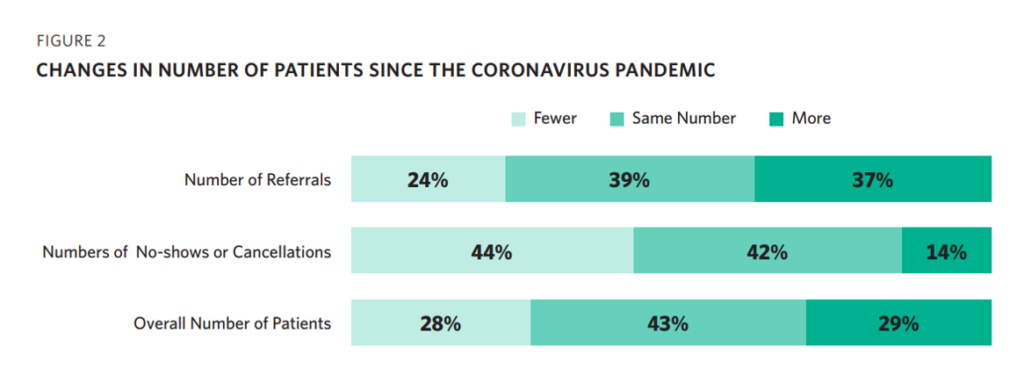 The second chart sparks an important insight into therapy-seeking patients’ mindsets: 44% of therapists had fewer cancellations or no-shows. Over one-third had more referrals for their services, and 29% of therapists served more patients:
The second chart sparks an important insight into therapy-seeking patients’ mindsets: 44% of therapists had fewer cancellations or no-shows. Over one-third had more referrals for their services, and 29% of therapists served more patients:
- By age group, 29% of therapists saw more adult patients 18 to 64 years of age
- 21% saw more adolescent patients ages 13-17
- 17% saw more older adults, ages 65-79
- 30% of psychologists saw more children under 13.
This last data point, that one-third more therapists saw more kids for mental health issues, speaks to the growing burden of depression and anxiety in younger people due to the feelings of social isolation and stress among the under-13 age group.
By race,
- 19% of therapists saw more White patients
- 11% saw more Asian patients
- 8% saw more Hispanic patients
- 11% saw more Black patients.
These numbers raise questions about peoples’ access to mental health services, particularly among people of color more disproportionately negatively affected by COVID-19: Black and LatinX health citizens.
The issue of clinician burnout has gotten a lot of deserved attention in this later phase of the COVID-19 pandemic. Sunday’s New York Times newspaper featured a detailed story from Reed Abelson explaining how Doctors Are Calling It Quits Under Stress of the Pandemic.
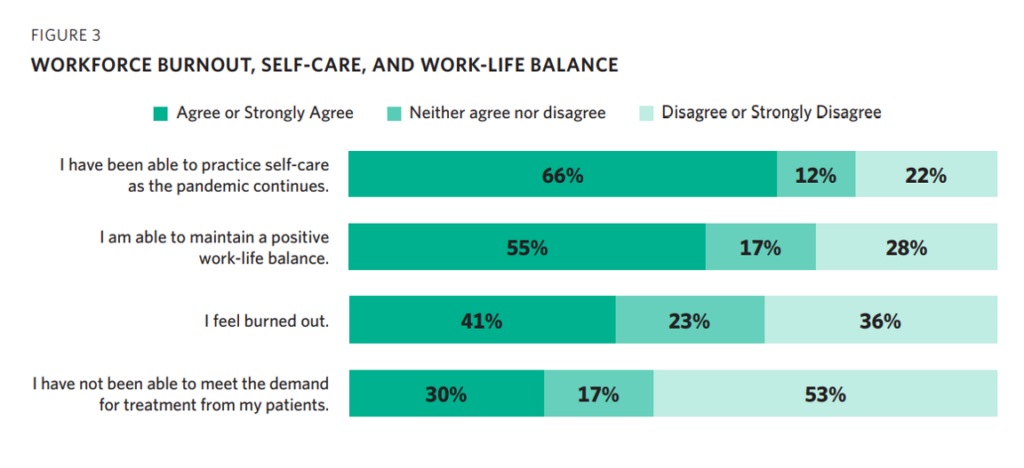
APA gauged psychologists’ feelings of burnout, shown in the third graph. Two-thirds of therapists said they have been able to practice self-care, and just over one-half able to maintain a positive work-life balance.
However, 41% of therapists felt burned out, with one-third unable to meet the demand for treating their patients. The converse of that is that only 53% of psychologists said they were able to meet patients’ demand for treatment.
While most psychologists have been treating patients remotely in the pandemic, they report virtual care being more challenging than treating patients face-to-face. Nearly 6 in 10 therapists reported a few barriers including internet access or connectivity, general technical difficulties, and privacy issues as the top challenges.
Stress in America series here in Health Populi earlier this year. Here are the links to those studies, together painting a picture of the epidemic accelerated in the pandemic: eroding mental and behavioral health in America.
Stress in America – COVID-19 Takes Toll on Finances, Education, Basic Needs and Parenting – Volume 1, May 2020
Stressed Out By COVID and Civil Unrest – the APA’s Stress in America Survey, Part 2, June 2020
Stress in America, Like COVID-19, Impacts All Americans – Political Stress impacts, October 2020
 Health Populi’s Hot Points: Since well before the COVID-19 public health crisis, there has been a shortage of mental health providers in the U.S. Some of the supply side challenges has been related to geographic distribution, under-serving rural areas. Some of the challenges relate to payment and reimbursement, and dis-connects with primary care as an on-ramp to diagnosing emotional health as a co-morbidity with chronic conditions and new diagnoses of acute diseases.
Health Populi’s Hot Points: Since well before the COVID-19 public health crisis, there has been a shortage of mental health providers in the U.S. Some of the supply side challenges has been related to geographic distribution, under-serving rural areas. Some of the challenges relate to payment and reimbursement, and dis-connects with primary care as an on-ramp to diagnosing emotional health as a co-morbidity with chronic conditions and new diagnoses of acute diseases.
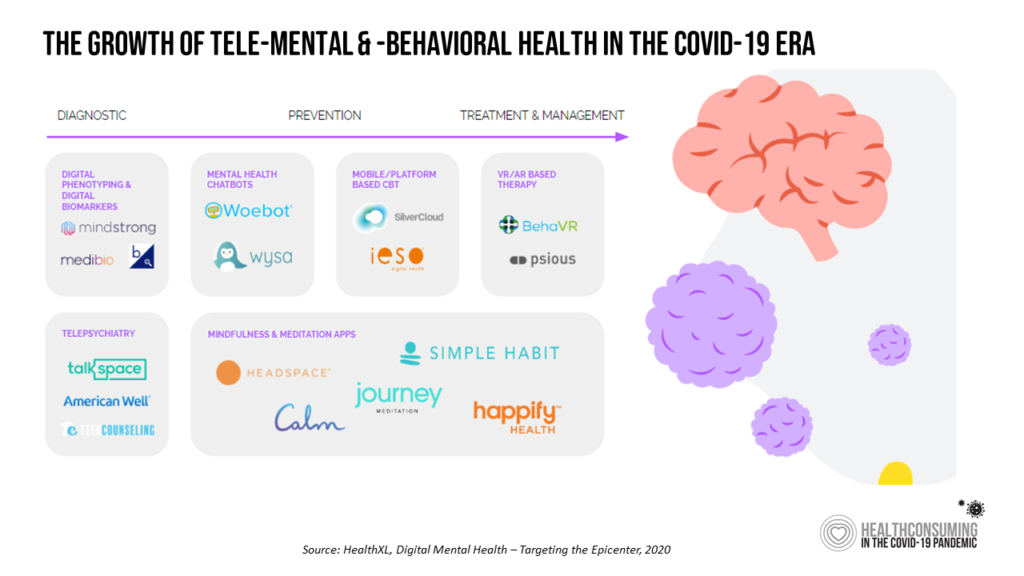
Our great friends at HealthXL put together the chart shown here, illustrating the many flavors emerging for digitally-enabled mental and behavioral health. Beyond the “online couch” of client-to-therapist therapy, we find mindfulness and meditation apps (such as the Calm app that collaborated with CNN on Election night), VR and AR-based therapies that have been powerful in helping people deal with traumatic stress and pain, and chatbots, among other emerging applications.
Digital platforms can help scale mental health supply where it needs to meet growing demand among health citizens profoundly impacted, mind, body, and soul, in and beyond the coronavirus pandemic. Watch this space for more evidence-based tools to help all of us deal with the toxic side effects of the public health crisis, ongoing.





 Grateful to Gregg Malkary for inviting me to join his podcast
Grateful to Gregg Malkary for inviting me to join his podcast  This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're
This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're