 The first year of the coronavirus pandemic in America was a kind of stress test on the U.S. health care system, revealing weak links and opportunities for bad behavior. “These are not just about individual instances or bad apples,” Dr. Vikas Saini, President of The Lown Institute, explained, referring to them as “cautionary tales” of the current state of U.S. health care.
The first year of the coronavirus pandemic in America was a kind of stress test on the U.S. health care system, revealing weak links and opportunities for bad behavior. “These are not just about individual instances or bad apples,” Dr. Vikas Saini, President of The Lown Institute, explained, referring to them as “cautionary tales” of the current state of U.S. health care.
Dr. Saini and his colleague Shannon Brownlee released the annual Lown Institute 2020 Shkreli Awards this week, highlighting their ten most egregious examples of the worst events in U.S. health care that happened in the past year — 2020, the year the coronavirus changed our lives and livelihoods.
A quick sidebar for context: The Awards are named for Martin Shkreli, the so-called “Pharma Bro” who managed hedge funds and pharma companies. When he led Turing Pharmaceuticals in 2015, he acquired a license for the drug Daraprim (an anti-malarial therapy also used for HIV/AIDS), raising the drug price from $13.50 a pill to $750 a pill. Shkreli was ultimately convicted on securities fraud (not related to the Draprim pricing strategy).
 Vitas and Shannon counted down the ten Awards, with Dr. Don Berwick and Dr. Mona Hanna-Attisha providing commentary on the events in the context of the coronavirus pandemic and the U.S. health care system.
Vitas and Shannon counted down the ten Awards, with Dr. Don Berwick and Dr. Mona Hanna-Attisha providing commentary on the events in the context of the coronavirus pandemic and the U.S. health care system.
Pediatricians, both Berwick and Hanna-Attisha represent larger public health perspectives beyond medical care, with Berwick having a long history with health care safety, quality, and equity, and Hanna-Attisha best-known for her advocacy of Flint, Michigan, residents facing the city’s sick water crisis as she observed children’s blood lead levels doubling in 2014.
Among the ten awards, I’ve selected three to highlight to synthesize one systemic issue that has plagued America’s response to the public health crisis. (The complete list is included below the digital fold in the Hot Points).
#7: Hospitals punish professionals for wearing personal protective equipment (PPE) in institutions. Early in the pandemic, many hospitals around the country took various punitive actions against staff who spoke out about safety issues on the front line of caring for patients diagnosed with COVID-19. In some cases, hospital management said that wearing masks was unnecessary and “would scare patients.” In other instances, some staff was fired for speaking out on safety issues like the lack of PPE and long test turnaround times. Dr. Berwick asserted that we need an atmosphere of openness, transparency, and leadership that doesn’t chill front-line workers from speaking up about patient and employee safety as well as quality of care.
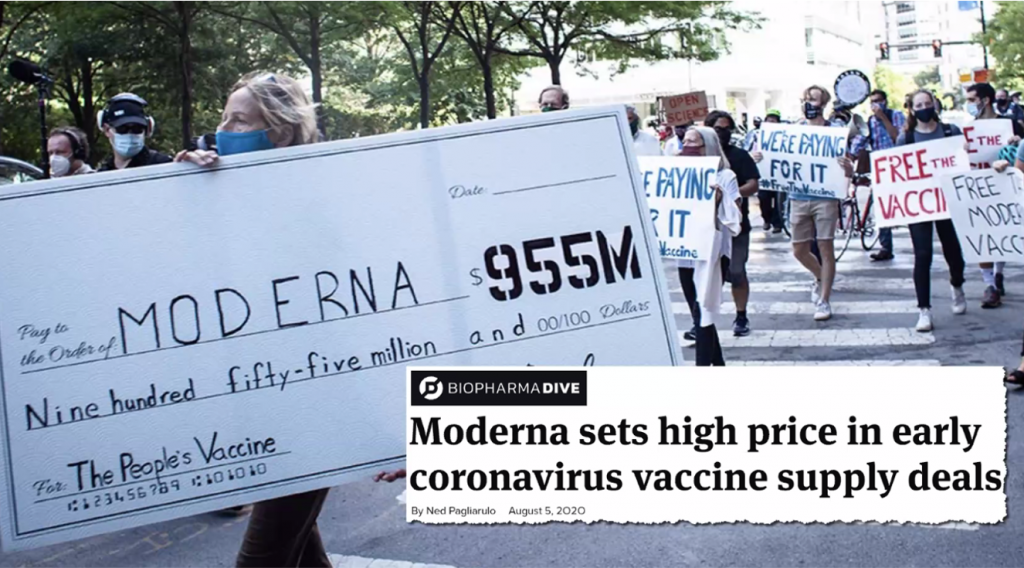 #2: Moderna, funded with nearly $1 billion in taxpayer dollars to develop a COVID-19 vaccine, sets the highest prevailing market price for the product. The price set was $32 to $37 per dose, requiring 2 doses for the full immunity coverage. The controversy here is that this was the highest price set although the company received 100% of the development costs for the vaccine covered by the U.S. government. (In total, U.S. agencies committed about $2.5 billion to help develop Moderna’s vaccine and buy doses based on New York Times reporting).
#2: Moderna, funded with nearly $1 billion in taxpayer dollars to develop a COVID-19 vaccine, sets the highest prevailing market price for the product. The price set was $32 to $37 per dose, requiring 2 doses for the full immunity coverage. The controversy here is that this was the highest price set although the company received 100% of the development costs for the vaccine covered by the U.S. government. (In total, U.S. agencies committed about $2.5 billion to help develop Moderna’s vaccine and buy doses based on New York Times reporting).
“This was not illegal; it’s the system,” the speakers noted in various ways. Dr. Saini followed up saying that this was, “a weird form of socialism,” with Dr. Berwick asking the question, “How much money is enough?” which is a current issue that will face the Biden Administration’s drug pricing reform strategies.
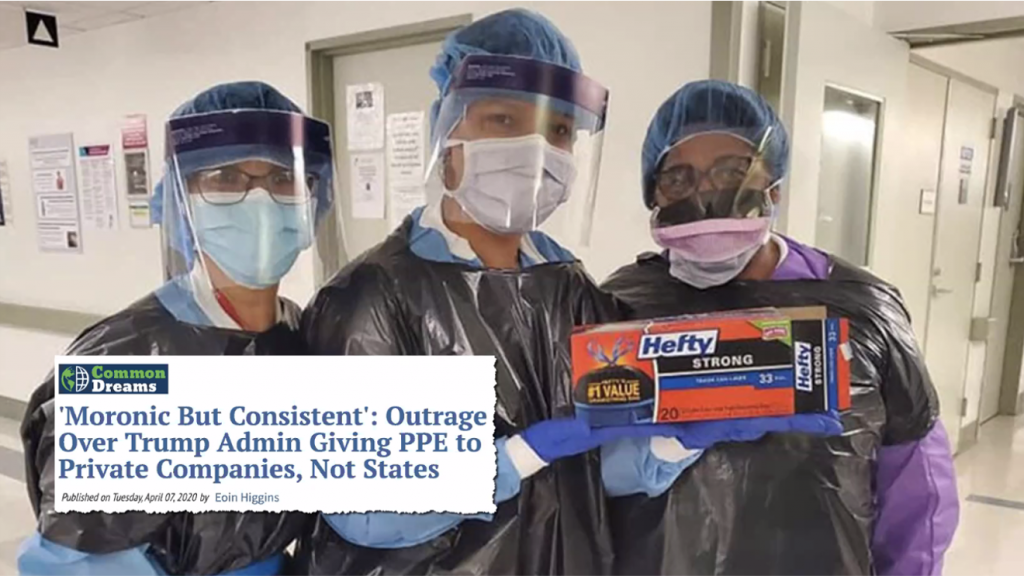
#1: The 50 U.S. States were forced to compete to buy PPE from six private companies as health care providers faced critical shortages of the equipment.
Given the very limited supply of PPE stockpiled in the U.S. for health care providers facing the pandemic, the Federal Emergency Management Agency (FEMA) launched Project Airbridge in late March 2020 to source face masks, gloves, surgical gowns and masks to fill the need.
While supplies were gathered in the effort, they were then distributed not directly to the States who could then channel the goods to the care providers who most needed them, but to six private companies.
This paved the way for those for-profit firms to sell the goods to the highest State bidders, creating a real bidding war among Governors.
“The U.S. lacked a plan….and a sense of management and organization, not chaos. We needed leadership and a plan,” Dr. Berwick commented on the situation.
Health Populi’s Hot Points: A consistent theme across all ten of the 2020 Shkreli Awards is that of “the business model(s)” which underpin health care in the U.S.
Let’s count the 2020 Corona-era Awards down to see the convergences across the events, which lead to an over-arching systemic issue and question.
#10 – Medical staffing companies cut doctors’ pay while spending millions on political ads
#9- Missouri sues televangelist Jim Bakker for selling fake coronavirus cure
#8 – These towns trusted a doctor to set up COVID testing; sample patient fee = #1,944
#7 – Nurse claims North Texas Hospital fired her because she wanted to wear a medical mask (discussed above)
#6 – Brigham and Women’s president wrote opinion piece critical of efforts to control drug prices
#5 – WHO patent pool for potential COVID-19 products is ‘nonsense,’ pharma leaders claim
#4 – Leaders indicted at Soldiers’ Home where at least 76 people died in COVID-19 outbreak
#3 – Some California hospitals refused COVID-19 transfers for financial reasons, state emails show
#2 – Moderna sets high price in early coronavirus vaccine supply deals (discussed above)
#1 – “Moronic but consistent” – outrage over Trump admin giving PPE to private companies, not States.
Taken together, we can synthesize one over-arching question: “Is the U.S. capable of acting with a sense of solidarity?” succinctly posed by Dr. Berwick.
The good doctor noted that we “need a value system of solidarity.”
We have been able to mobilize in wartime, Dr. Berwick observed. FDR demonstrated readiness in World War II. “It wasn’t easy or pretty but it happened,” Dr. B said.
In the pandemic, America’s inability to do this has cost us thousands of lives.
Dr. Hanna-Attisha dove further into this idea in terms of what this says about the U.S. health care system. “Why don’t we care about our neighbors versus ourselves? How can we shift from individualism to collectivism for each other?” the way she has helped her fellow health citizens in Flint do.
“How do we get to a place where we are ‘we’ caring for each other, and not avert our eyes?” Dr. Hanna-Attisha asked.
We have that opportunity to open our eyes as we begin a New Year, calling out egregious examples of bad behavior in U.S. health care. These come from systemic issues of “business models” gone awry in U.S. health care.
As I continue to explain and push for Health Citizenship in America, these events from the past year point out at least ten arguments for building health care back better with a national, love-thy-brother-and-sister lens. Some thoughts on “we” versus “I” in a public health crisis, in a value system of solidarity…
We could have nationalized a PPE and testing strategy from the beginning.
We could have joined with our global health citizens and governments to share information and patents for what are public health products — vaccines, therapies, preventive strategies — to hasten development and goodwill.
What would the world look like if, on behalf of wellbeing for the human race, we make intellectual property available in the case of pandemic crises?
What if, in this handful of cases, corporations “acted with generosity,” as Dr. Berwick phrased the challenge.”
Considering “the concept of bottling up knowledge to save millions of lives…I don’t think there’s an economic theory withstanding scrutiny,” Dr. B. concluded.





 I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for