Financial Experience (let’s call it FX) is the next big thing in the world of patient experience and health care.
 Patients, as health consumers, have taken on more of the financial risk for health care payments. The growth of high-deductible health plans as well as people paying more out-of-pocket exposes patients’ wallets in ways that implore the health care industry to serve up a better retail experience for patients.
Patients, as health consumers, have taken on more of the financial risk for health care payments. The growth of high-deductible health plans as well as people paying more out-of-pocket exposes patients’ wallets in ways that implore the health care industry to serve up a better retail experience for patients.
But that just isn’t happening.
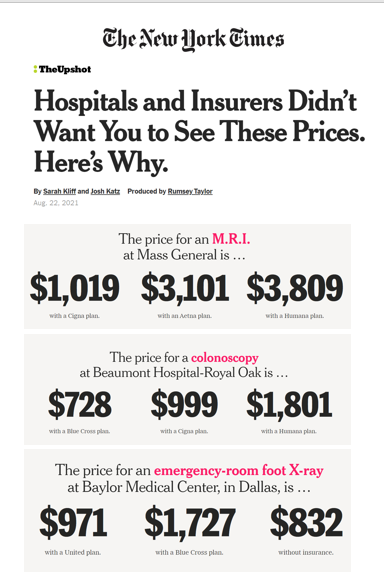
One of the challenges has been price transparency, which is the central premise of this weekend’s New York Times research-rich article by reporters Sarah Kliff and Josh Katz: Hospitals and Insurers Didn’t Want You to See These Prices. Here’s Why.
The first chart presents data from the research which the Times has been gathering over time, nationally, from patient reports and requests to hospitals.
Patients have been much more forthcoming than hospitals, the journalists have found.
As you can see, the range of prices for various services can vary by as much as four times for, say, and MRI within the Mass General hospital system, depending on the payer. When we think about health care pricing variations, then, it’s not just between hospitals in a particular geography or ZIP code, but it happens within institutions based on contract negotiations with health plans.
The article provides, “numerous examples of major health insurers — some of the world’s largest companies, with billions in annual profits — negotiating surprisingly unfavorable rates for their customers. In many cases, insured patients are getting prices that are higher than they would if they pretended to have no coverage at all,” Sarah and Josh learned.
And with more patients-as-consumers with more financial skin-in-the-game, “high-deductible plans [that] leave them responsible for thousands of dollars in costs before coverage kicks in,” the article explains. “Even when workers reach their deductible, they may have to pay a percentage of the cost.”
With that challenge comes the opportunity for health information technology developers to focus on patient financial experience (PFX).
Patient experience and engagement were a trending topic at the recent HIMSS 2021 conference, a growing portion of panels and presentations focusing on patient billing, revenue cycle management, and health consumers’ financial literacy.
In the weeks preceding #HIMSS21, my email inbox and Google alerts received a virtual library of reports and studies from vendors and researchers offering solutions and scenarios to expose and address the patient financial experience. One descriptor noted “a strategic partnership to humanize the healthcare financial experience.” Another talked about the concept of “patient-centered billing.” A third riff on the PFX theme was a new FinTech Award given to Patientco for the “Best Patient Financial Engagement Platform” in 2021.
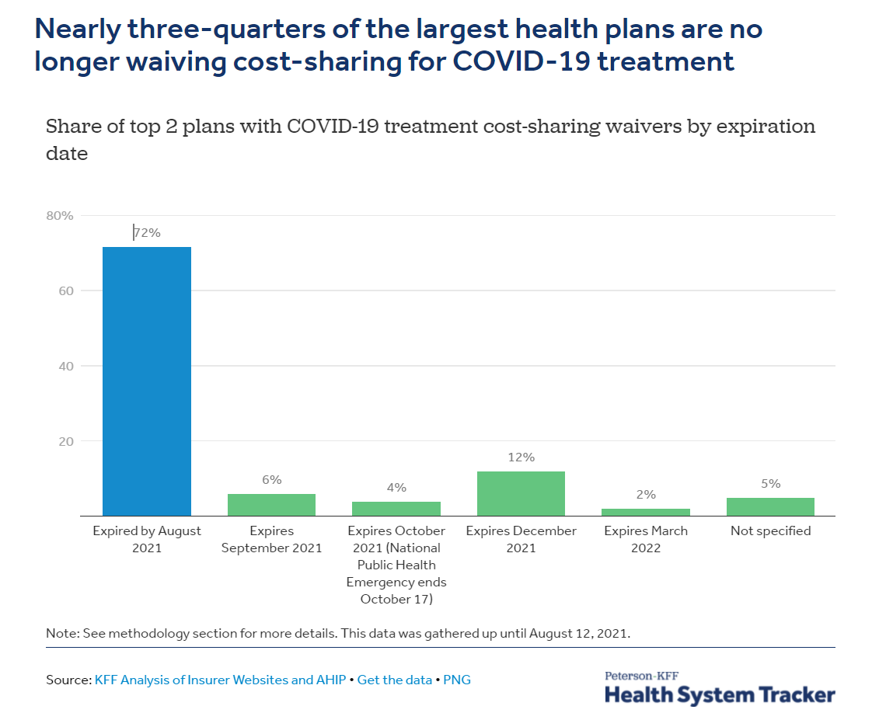 The coronavirus pandemic has further added to the challenge of transparency and patient life-flows for medical cost management which can erode trust and an engaging patient-provider relationship.
The coronavirus pandemic has further added to the challenge of transparency and patient life-flows for medical cost management which can erode trust and an engaging patient-provider relationship.
Most commercial health plans have begun to pass COVID-19 medical costs on to patients, according to the latest Peterson-KFF Health System Tracker. Specifically, “We find that 72% of the two largest insurers in each state and DC (102 health plans) are no longer waiving these costs, and another 10% of plans are phasing out waivers by the end of October,” the Peterson-KFF research quantified.
Patients-as-consumers in the U.S. are also facing the possibility of inflation for some household spending categories. These concerns have contributed to Americans’ precipitous drop in consumer sentiment timed with the realization that the COVID-19 Delta variant was spiking infections throughout the U.S.
The University of Michigan’s consumer sentiment index fell to 70.2 from 81.2 in July 2021, the lowest read since December 2011.
One category of household spending expected to inflate is out-of-pocket health care costs. These are projected to grow nearly 10% a year through 2026, Kalorama has estimated in a recent forecast.
Multiple drivers are contributing to significant out-of-pocket spending growth, Kalorama identified, including regulatory and policy changes, health insurance actions, and demographic trends such as aging and growing burden of multiple chronic conditions among U.S. health citizens.
 From PYMNTS.com, an essay that makes it clear that payments are an integral part of the customer experience. For healthcare,
From PYMNTS.com, an essay that makes it clear that payments are an integral part of the customer experience. For healthcare,
“New payment capabilities are addressing critical needs by providing increased visibility to expected patient costs pre-treatment to avoid billing surprises, and automatically setting up payment plans before care is delivered. This is increasing patient satisfaction while also preventing lost revenues and reducing AR and collection costs.”
COVID-19 accelerated patients’ expectations of more contact-less payments and online patient financial apps and tools, from scheduling appointments to payment options, plans, and transactions.
Elavon, a unit of US Bancorp (the fifth largest bank in the U.S. at the time of this writing), process medical payments across the health care ecosystem, and published the company’s 2021 Healthcare Payments Insights Report.
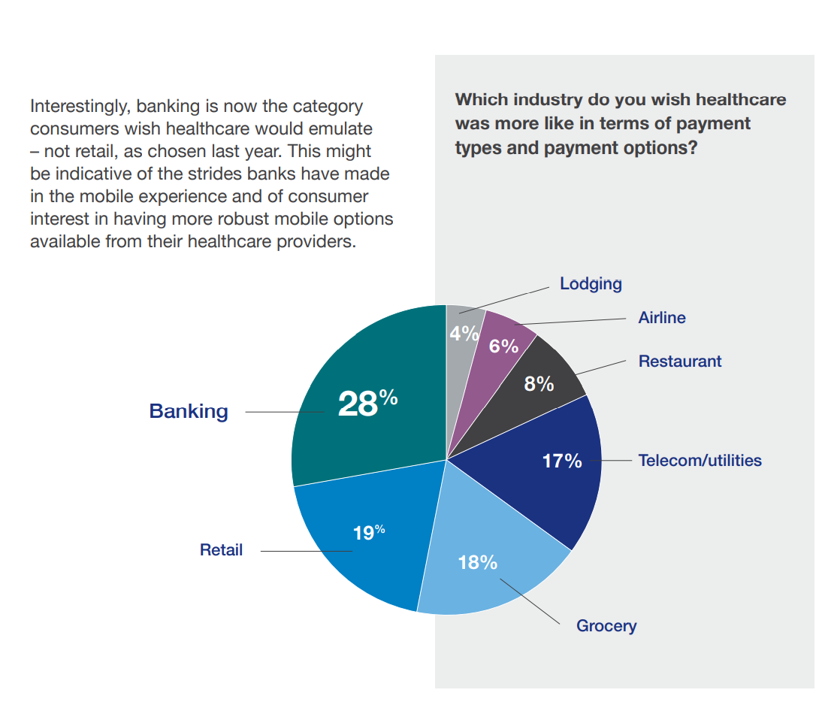
The graphic from Elavon’s consumer survey findings summarizes that patients increasingly expect more convenience and more support from health care providers for financial experience workflows, from clean payment devices and touchless check-ins to bill discounts and recurring payment options.
Health consumers also would like medical providers to offer and support payment methods across a range people are used to using in their everyday lives via contactless credit/debit card (48%), using online money transfer services like PayPal, Venmo and Zelle (31%), Think of mobile wallet (26%), paying by text (17%), or through a QR code (13%).
Think of this as omni-channel payment the same way we’re seeing health care evolve through omni-channel “sites” both face-to-face/brick-and-mortar and virtual, through telehealth, remote health monitoring at home, via mobile apps, and other digital front doors.
Given consumers’ growing omni-channel muscles in retail and other industries, Elavon wondered how health care payments stacked up compared with peoples’ other payment experiences. The best FX experiences. consumers told Elavon, were found in banking (28%), retail (19%), and grocery (18%), which those patients said should be role models for health care providers in designing patient financial experience programs.
Health Populi’s Hot Points: As if on cue, Geisinger Health System launched a zero-interest payment plan for patients’ out-of-pocket costs, on August 19, 2021. Claiming to be the first system of its kind, Geisinger is working with PayZen to use AI in developing the technology that will allow consumers to make medical payments over time.
Geisinger is responding to the consumer experience factor where patients are more concerned about billing than the quality of care, Waystar learned in their consumer research on post-COVID healthcare consumers.
The Elavon consumer survey also covered patients’ views on affordability — where concerns remain high. Patients’ perspectives on affordability of health care — or lack thereof — colors peoples’ overall experience with health care financing.
Two-thirds of U.S. adults worry about unexpected medical bills, and another 2 in 3 are afraid they won’t be able to afford health care in 2021.
Thus, consumers welcome the availability of receiving a discount for paying their entire medical bill in one lump sum, Elavon found: 75% of patients said they’d be likely to pay that medical bill all at once with a discount. Without a discount, six in ten patients would likely take advantage of a recurring payment plan, via the Elavon study.
 In putting together this post, I searched on the term “financial experience and FX” and happened upon the first search result written by Edwin Chong on LinkedIn: FX: The financial experience. [Edwin reminds us that FX in this instance isn’t the acronym for our friends in the FOREX financial markets, or in cable television network-land, but a shorthand for “financial experience”].
In putting together this post, I searched on the term “financial experience and FX” and happened upon the first search result written by Edwin Chong on LinkedIn: FX: The financial experience. [Edwin reminds us that FX in this instance isn’t the acronym for our friends in the FOREX financial markets, or in cable television network-land, but a shorthand for “financial experience”].
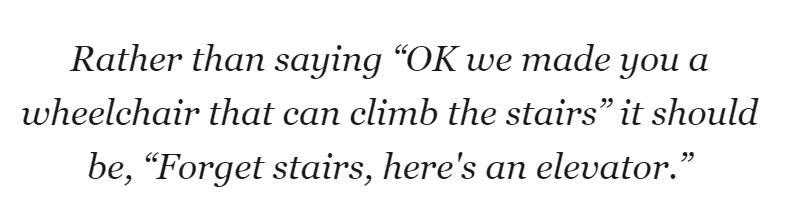
Edwin came to write his post drawing from his participation on a panel about financial inclusion. That’s synchronicity at work, as #financialinclusion is underneath so much health care financial toxicity, hitting people of lower income and social determinants’ risks than other health citizens in the U.S.
This quote comes out of Edwin’s essay: “Rather than saying ‘OK we made you a wheelchair that can climb the stairs’ it should be, ‘Forget stairs, here’s an elevator.'”
Would that we can keep this mantra and mindset in our UXhealth design heads, looking to improve patients’ health care experiences, from the physical and clinical to the financial.
That’s the short-to-mid-term wish, if I were Healthcare Reform Queen.
Beyond the short-to-mid-term, my broader more audacious objective and Health/care Holy Grail is to imagine a U.S. where people are full-on health citizens, not worrying about where their health care is covered, what their co-pays are, or how to navigate through a challenging, bureaucratic, opaque medical payments landscape. For now, we live in the present, wrestling with getting systems and processes right for our fellow health citizens, and at the same time work toward building an equitable health future for all.




 Thank you, Jared Johnson, for including me on the list of the
Thank you, Jared Johnson, for including me on the list of the  I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a