COVID-19 exacted a toll on health citizens’ mental health, worsening a public health challenge that was already acute before the pandemic.
 It’s World Mental Health Day, an event marked by global and local stakeholders across the mental health ecosystem.
It’s World Mental Health Day, an event marked by global and local stakeholders across the mental health ecosystem.
On the global front, the World Health Organization (WHO) describes the universal phenomenon and burden of mental health on the Earth’s people…
- Nearly 1 billion people have a mental disorder
- Depression is a leading cause of disability worldwide, impacting about 5% of the world’s population
- People with severe mental disorders like schizophrenia tend to die as much as 20 years earlier than the overall population
- One in every 100 deaths is by suicide, the fourth leading cause of death for young people aged 15-29 years.
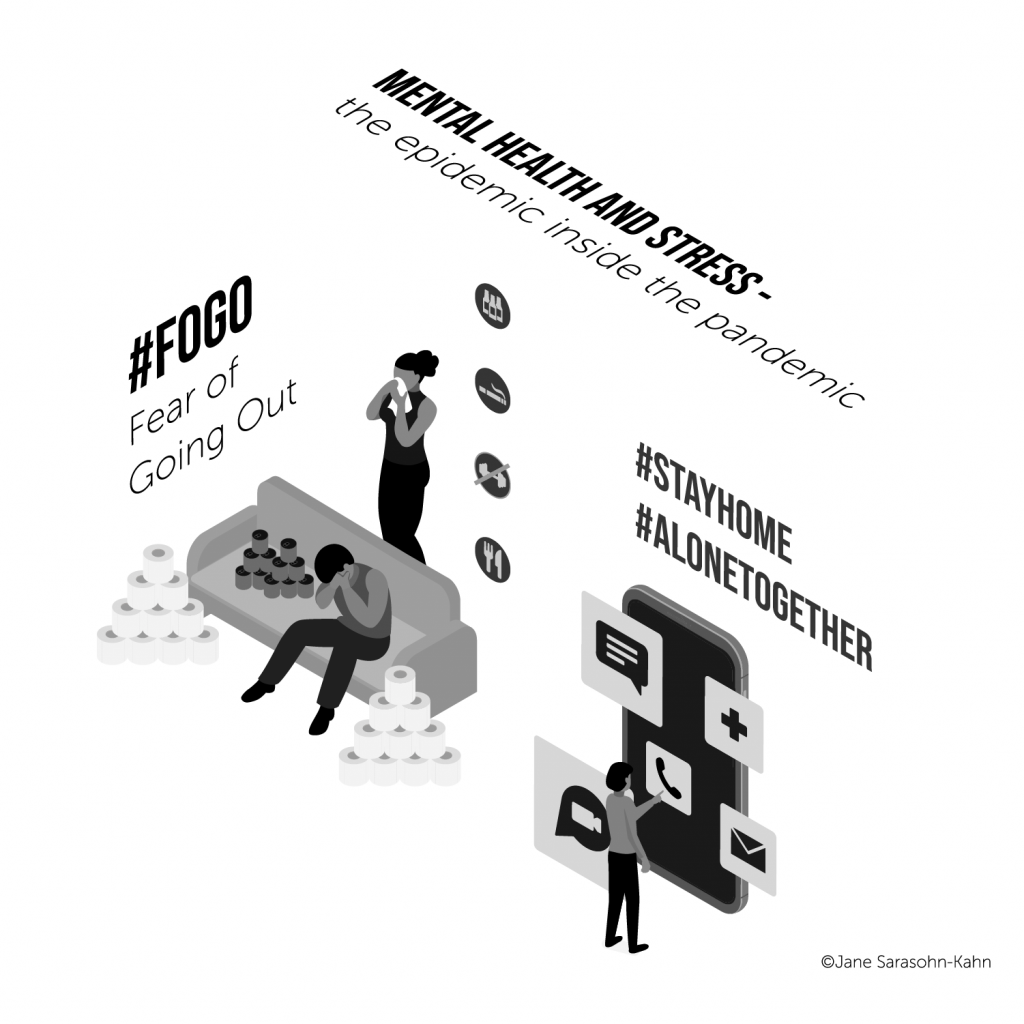 And of course, the COVID-19 pandemic exacerbated the world’s mental health.
And of course, the COVID-19 pandemic exacerbated the world’s mental health.
On the promising front,
- There are available therapies, medications, and digital therapeutic combinations that successfully address the most common mental health conditions — notably, anxiety and depression
- There is a solid return-on-investment (ROI) for anxiety and treatment measured in the US of $1 spent on these conditions yielding a $5 return (5:1 ROI)
- For drug dependency in the U.S., there is an ROI of 7:1 for every $1 invested, reducing crime and criminal justice costs.
Still, as there are seemingly intractable disparities for physical health in the U.S. and much of the world, so, too, does mental health bear the burden of inequities.
As WHO notes, “the gap between demand for mental health services and supply remains substantial,” resulting from chronic under-investment over decades in mental health promotion, prevention, care, and continued stigma and discrimination.
 Health Populi’s Hot Points: This year’s theme for World Mental Health Day focuses on “Mental health in an unequal world.”
Health Populi’s Hot Points: This year’s theme for World Mental Health Day focuses on “Mental health in an unequal world.”
COVID-19 shined a blindingly bright light on inequalities in health and health care, and this blurred onto mental health care and access, as well.
Across the world, the impact of ethnicity and race, poverty and income inequality as well as job security, shaped how one person fared against the coronavirus compared with another who bore greater risks to the social determinants of health.
At least 75% of people with mental disorders living in low and middle-income nations are unable to access mental health services according to the World Federation for Mental Health.
That access challenge extends to low and middle-income communities in the U.S., too. Encouragingly, we’ve seen tele-mental health and therapy, along with digital therapeutics expanding for mental health in the U.S. and abroad, with more therapies under review for regulatory approval as well as clinical trials to bolster evidence and ROI cases.
There is no health without mental health, Surgeon General Dr. David Satcher asserted working with President Bill Clinton and President George W. Bush. Dr. Satcher was a pioneering Civil Rights leader, especially for public health for all health citizens. He knew the power of integrating mental health in the context of overall health, and the role of socioeconomic factors and adverse childhood events both academically and first-hand as a child barely surviving whooping cough.
 Dr. Ruth Shim wrote about mental health inequities in the context of COVID-19 in JAMA in September 2020,
Dr. Ruth Shim wrote about mental health inequities in the context of COVID-19 in JAMA in September 2020,
The emergence of COVID-19 has brought renewed attention to disparities and inequities in health outcomes that exist for US residents who are most commonly oppressed and marginalized in US society. These inequities in outcomes are persistent across many conditions but are particularly salient when considering mental illnesses and substance use disorders. Ample data support the understanding that the social determinants of health and mental health are most responsible for health disparities and inequities…[and] how these social determinants of mental health are associated with inequities in the incidence and prevalence of depression in the context of the COVID-19 pandemic.
Chronic under-investments in mental health can be addressed by,
- Embedding mental and behavioral health questions into the primary care visit
- Expanding health citizens’ access to broadband connectivity and evidence-based, well-designed health apps for cognitive behavioral therapy
- Ensuring access to services through parity in mental health coverage and payment, especially for long-underserved populations (say, in Medicaid programs)
- Funding clinical trials to build the evidence base for mental and behavioral health therapies
- Continuing to break down the stigma associated with mental health conditions and seeking care to treat them, and
- Nurturing a civil society that bolsters community, kindness, and respect.
There is no health without mental health.




 I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for