A coalition of health care providers, health plans, technology innovators, NGOs, and medical societies has come together as the Public Health Tech Initiative (PHTI), endorsed by the Consumer Technology Association (CTA) with the goal of advancing the use of trustworthy digital health to proactively meet the challenge of future public health emergencies….like pandemics.
 At the same time, CTA has published a paper on Advancing Health Equity Through Technology which complements and reinforces the PHTI announcement and objective.
At the same time, CTA has published a paper on Advancing Health Equity Through Technology which complements and reinforces the PHTI announcement and objective.
The paper that details the PHTI program, Using Heath Technology to Response to Public Health Emergencies, identifies the two focus areas:
- Digital health care solutions that are especially appropriate to address public health emergencies as well as the barriers to prevent their adoption and persistent use; and,
- Data and privacy concerns, the lack of data sharing, and fragmentation of the public health system that underpins operational barriers to data liquidity and access.
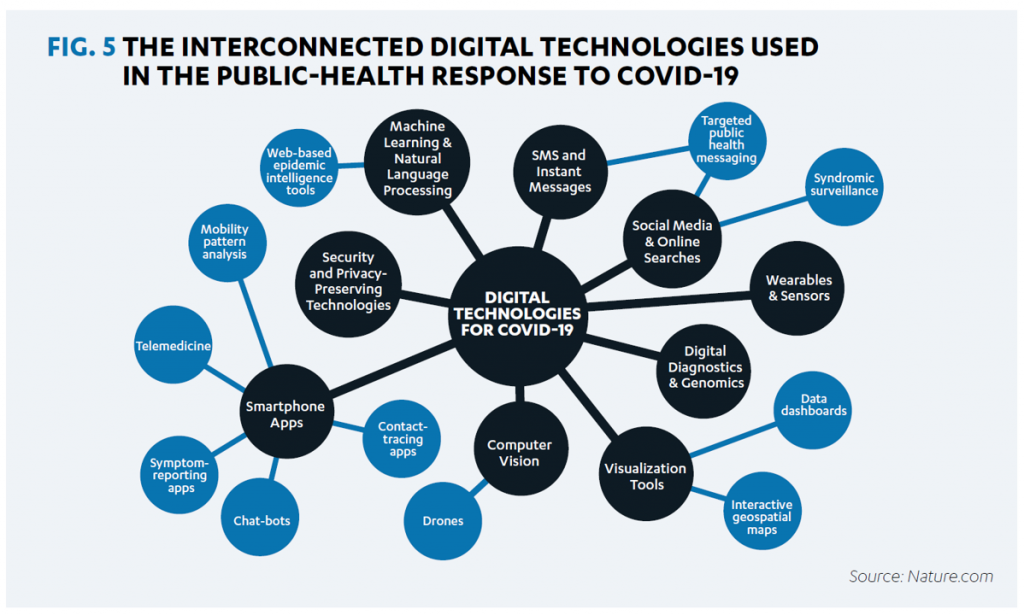
That second point is illustrated by the first diagram, showing the interconnected nature of data sources that are generated by the U.S. health/care ecosystem of:
- Some 3,000 health departments and boards of health
- 59 state and territorial health departments
- Tribal health departments
- Over 160,000 public and private labs
- Hospitals and health care providers
- Health plans
- Volunteer organizations, along with other data-creating entities for public health.
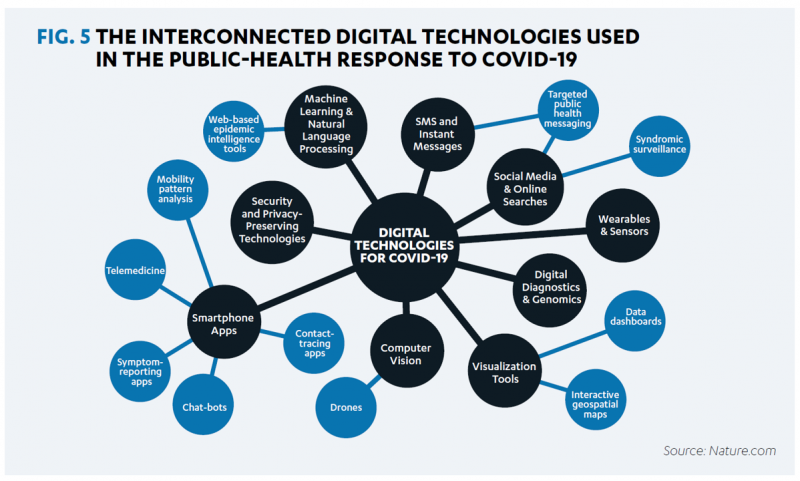
 From the emergence of the COVID-19 pandemic in the U.S. during the first quarter of 2020, digital health rose to the occasion: namely telehealth, remote and virtual care mounted by health care providers across the nation within days of the WHO calling the virus a global pandemic.
From the emergence of the COVID-19 pandemic in the U.S. during the first quarter of 2020, digital health rose to the occasion: namely telehealth, remote and virtual care mounted by health care providers across the nation within days of the WHO calling the virus a global pandemic.
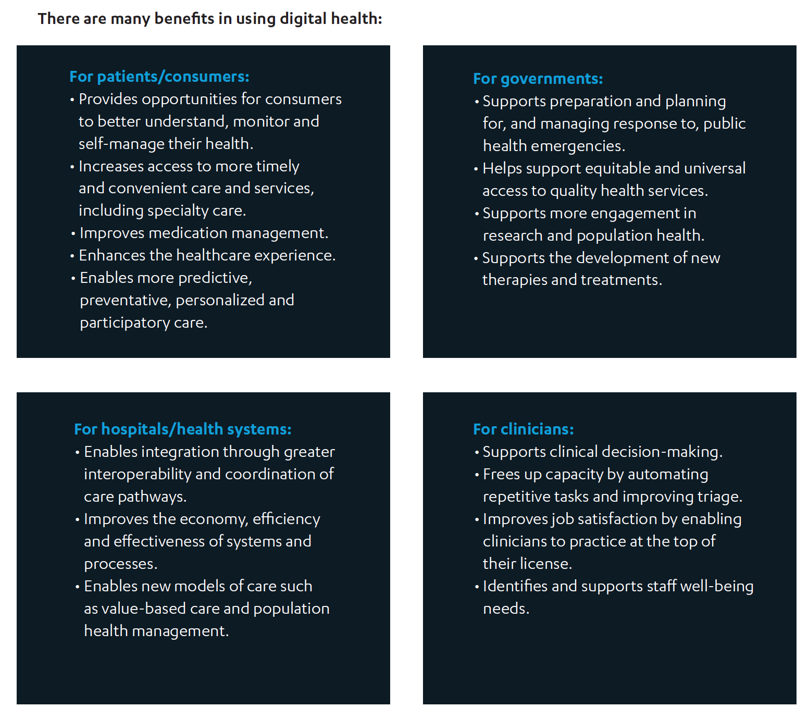
The PHTI notes many benefits from using digital health, organized in this second chart captured from the report:
- For patients, the ability to self-care at home, more timely and convenient access to services (both primary and specialty care), improving medication management, and enhancing the healthcare experience (when well-designed)
- For hospitals and health systems, better integration and interoperability with coordinated care, improved efficiency, and enabling new models of care delivery (esp. value-based)
- For public sector payors, better responses to public health emergencies, supporting universal equitable access to services, and supporting research, population health, and development of new therapies and treatments
- For clinicians, freeing up capacity and improving triage, improving job satisfaction to enable high-touch in person care for patients who most need face-time with clinicians, and more effectively supporting staff well-being.
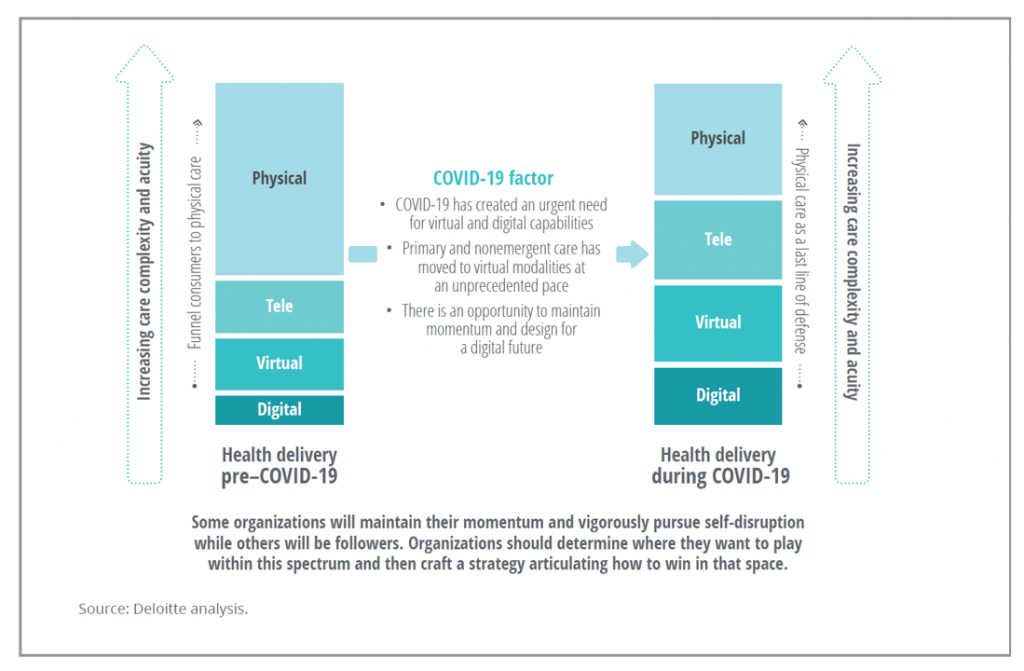 The third bar chart details the partial shift from physical face-to-face health care encounters to more tele-care, virtual care, and care delivered through digital tools.
The third bar chart details the partial shift from physical face-to-face health care encounters to more tele-care, virtual care, and care delivered through digital tools.
That’s all well and good, and when designed for clinicians’ and patients’/consumers’ best interests, values, and work-flows, the outcomes can be efficient, effective, and aligned for all stakeholders.
However, there remain several key barriers preventing the full use of digital health, the PHTI group identified. These include:
- Broadband availability and quality
- Health care workforce training
- Health consumer, patient, and caregiver literacy for and acceptance of digital health work- and life-flows
- Reimbursement for digital/telecare/virtual care services for both public and private payors
- Lack of data interoperability, and
- Health data and privacy considerations, especially due to varying state laws that fragment a Federal/national approach to personal data protection.
These barriers are an underlying theme in CTA’s paper on advancing health equity through technology, sponsored by CTA and the App Association’s Connected Health Initiative (ACT). Together, the two groups convened the Health Equity and Access Leadership Coalition (HEAL) which includes about three dozen organizations from across the health care landscape. HEAL’s objective is to advance health equity through digital technologies, focused on access to broadband and technology, digital literacy and access, and data and privacy.
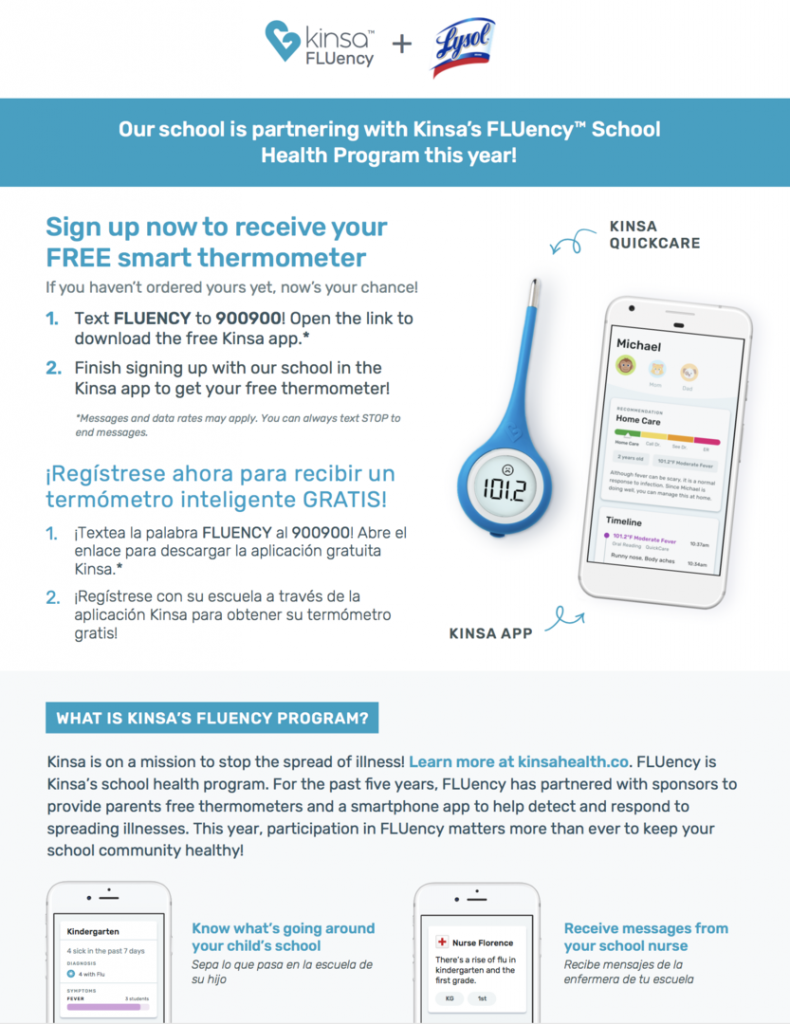 One terrific example that clearly illustrates the opportunity to address these three pillars is the Kinsa Health School Program, described in the report. Kinsa Health began to market the first FDA-cleared smartphone-connected thermometer in 2013. Instead of thinking “thermometer” in its original Webster’s Dictionary definition, let your mind consider how Kinsa describes its device: as an early warning system to detect and respond to contagious illness.
One terrific example that clearly illustrates the opportunity to address these three pillars is the Kinsa Health School Program, described in the report. Kinsa Health began to market the first FDA-cleared smartphone-connected thermometer in 2013. Instead of thinking “thermometer” in its original Webster’s Dictionary definition, let your mind consider how Kinsa describes its device: as an early warning system to detect and respond to contagious illness.
In the company’s Kinsa for Schools program, called FLUency, Kinsa operates a sponsorship program for corporate donors to fund thermometer donations in their local markets (or where employees live) to channel the devices to Title I schools (which generally serve students from lower-income households).
According to the CTA/ACT/HEAL report, the program has helped school bolster attendance and generated a treasure trove of real-time data on fever rates that are building data models that can help track illness among students and in the communities in which they live.
Health Populi’s Hot Points: CTA’s two reports dovetail and reinforce each other’s bottom-lines: that pandemic preparedness, and public health overall, are bolstered when taking a holistic approach that is inclusive for all health citizens across all geographies. We know from the coronavirus era that living in one particular ZIP code does not protect the person living there from being exposed to the tricky virus.
This was not new-news to the public health community, but was revealed once again in vivid terms when it came to COVID statistics on exposure, complications, and deaths occurring more likely in one community versus another.
The health equity paper ends with the sentences:
“The HEAL Coalition recognizes that greater and appropriate use of digital health plays a significant role in addressing and mitigating health inequities in the United States. We must ensure there is intentionality in design, distribution, and delivery.”
CTA’s CEO Gary Shapiro received the French Legion of Honor on 20th October from President Emmanuel Macron, who called Gary, a “tech pioneer who became a tech giant” with a commitment” to “people, values and principles.”
CTA is in the forefront of health/tech innovation and advocacy, which is why I plan to attend CES 2021 live, in person. I’m looking forward to speaking there on top digital health trends, along with collaborating on a panel brainstorming telehealth for mental and behavioral health access and innovation.




 I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for