While nurses were in short supply before 2020, the coronavirus pandemic and stress on front-line health care workers exacerbated the shortage of nursing staff globally. This urgent call-to-action became the rallying cry and objective for this weekend’s #NurseHack4Health, “The Front Line Is Shrinking,” with the goal of building a sustainable workforce of the future.
 I’m grateful to the nurse leadership teams at Johnson & Johnson, Microsoft, and Sonsiel for inviting me to participate in another round of the #NurseHack4Health hackathon pitches over the past weekend.
I’m grateful to the nurse leadership teams at Johnson & Johnson, Microsoft, and Sonsiel for inviting me to participate in another round of the #NurseHack4Health hackathon pitches over the past weekend.
This year inspired nearly 800 registrants from at least 48 countries to convene via Microsoft Teams for one huge, timely and profound purpose: to acknowledge and improve the state of nursing for nurses, for patients, and for health care. Whether working in rural America, urban Britain, central Mumbai or suburban Auckland, the nursing profession s in a world of hurt.
And this hurts Everyone.
The nurse-hackers organized in teams across four tracks of themes to address the sustainable nurse workforce:
- Diversity in practice and care
- Education, upskilling, professional development
- Driving administrative efficiency in nursing care delivery, and
- An Open Track which hosted new-new innovations to restore and re-imagine sustainability for now and future nurses and nursing.

I collaborated on Track 4, which featured four fascinating and creative solutions with unique and compelling approaches for their hacks.
- Team Empower, which went right for the Quadruple Aim — that fourth leg of the health sustainability stool of clinician-nurse burnout — and a solution incorporating “3 C’s” of clarity (of role and validating work), comfort, and community. This solution leveraged consumer-facing digital platforms like the Apple Watch and Fitbit trackers, and sought sponsorships in the larger health/care/retail ecosystem like meal preparation channels and retail coupons that fit into nurses’ everyday life-flows.
- Nurse Wellness in the Digital Age, focusing on the severe anxiety and stress that precede trauma in the moment at work when a nurse is dealing with a patient acutely in in what becomes an acute moment-of-truth for the nurse. This solution confronted the datapoint that two in three nurses working in critical care are considering leaving their jobs. One of the tool’s outcomes created a kind of heat map that illustrated just where and when the most high-anxiety sites in an organization were emerging. At the same time, the care provider would receive personalized messages to breathe, to feel acknowledged, and to take a moment to pause.

- The Price is Right, such an appropriate name for a “reverse pipeline” workforce solution that to me felt like Uber Meets eBay Meets Nursing. The team pointed out that the nursing pipeline is “linear,” yet there is so much nurse human capital outside the clinical setting — whether nurses who have retired, those in administration, or others who have left the field entirely. Yet many of these nurses would like to get back to clinical work — perhaps not full-time, but more in a gig model. This solution would/could go well beyond the reverse-pipeline model but appeal to many nurses who, in the wake of the pandemic, seek greater flexibility for their own work- and life-flows.
- Transit Care, the fourth of our track hacks, addressed the common story of a patient moving from one setting to another — say, from a memory care unit to an ER due to a fall — with the patient’s information failing to follow the patient when she’s admitted to the emergency department. Information can in fact be missing, inaccurate, conflicting, and/or incomplete, the team explained. The consequences of this information gap can result in readmission, poor outcomes, or worse — major adverse events. The solution built a QR code embedded with the patient’s full data (clinical, social determinants, and other relevant bits of information to complete the patient’s profile) with a designated caregiver at both ends of the transfer — from the originating site to the admission site.
As this circle graphic illustrates, a good hack starts with a story — which each of our four solutions on Track 4 indeed did — a tool that meets a real need, can be iterated, tested, and finally scaled.
One of the biggest benefits for those of us involved in hackathons is the community we continue to build through participating in them. So it was joyful for me — even working on this on a Sunday! we on our panel-team discussed during the process — to work in virtual arm in arm via Teams with:
- Oriana Beaudet, VP of Innovation at ANA Enterprises
- Rhonda Collins, Chief Nursing Officer with Vocera
- Lindsey Roddy, a nurse entrepreneur from Milwaukee, and
- Patrick Zummo, a health-hacker himself and innovator with the Mayo Clinic.
You can read more about these and other wonderful nurse leaders here on the panelists’ portal for #NurseHack4Health.
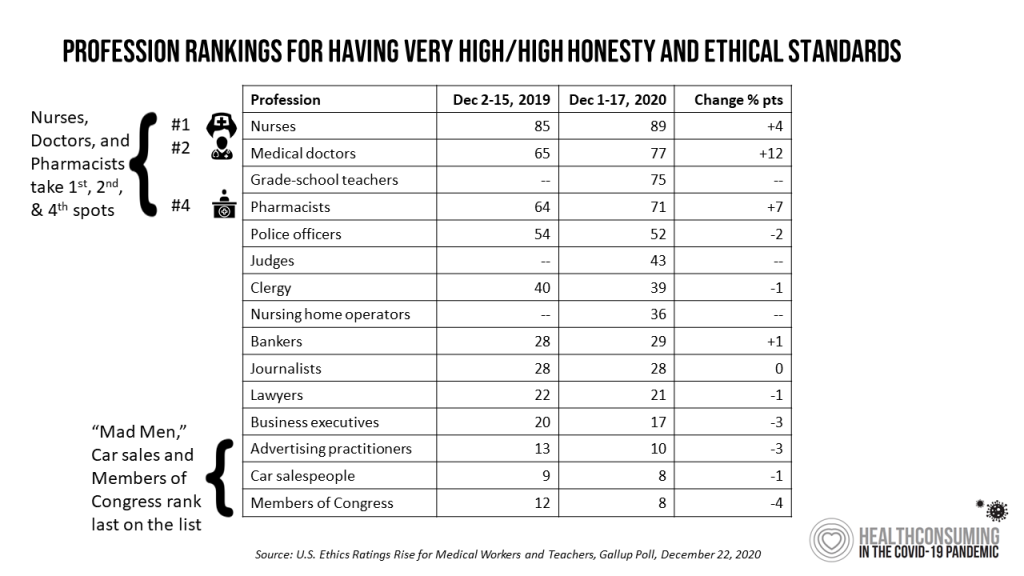 Health Populi’s Hot Points: Nurses, year after year, rank top in peoples’ minds for honest and ethical standards in the annual Gallup Poll. Doctors and Pharmacists also ranked high in the latest survey on the topic, along with grade school teachers who have been their own brand of frontline workers in the pandemic era.
Health Populi’s Hot Points: Nurses, year after year, rank top in peoples’ minds for honest and ethical standards in the annual Gallup Poll. Doctors and Pharmacists also ranked high in the latest survey on the topic, along with grade school teachers who have been their own brand of frontline workers in the pandemic era.
Even as nurses are lauded as being “the most” trusted profession in the U.S. (and globally), there is a major and dangerous disconnect between that “feeling” and the raw reality that without a strong nurse backbone, health care, public health, and individual patient health are compromised.
We see this playing out the world over with hospital inpatient beds filled with patients continuing to battle COVID-19, and clinicians begging health citizens to get vaccinated to prevent coronavirus complications that can lead to Long COVID, lifelong chronic respiratory and neurological conditions, and to be sure — death.
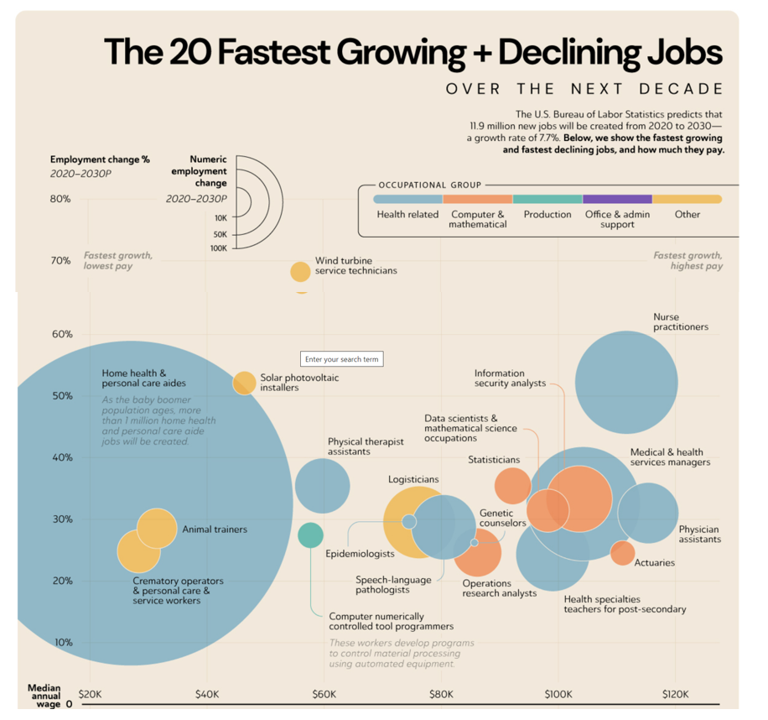 Beyond the pandemic — if we can try and think that far beyond the current and endemic phase of this public health crisis — the U.S. Bureau of Labor Statistics forecasts the fastest growing jobs looking to 2030 are health care workers — particularly those working in patients’ homes.
Beyond the pandemic — if we can try and think that far beyond the current and endemic phase of this public health crisis — the U.S. Bureau of Labor Statistics forecasts the fastest growing jobs looking to 2030 are health care workers — particularly those working in patients’ homes.
Check out all the “blue” circles on this future job map: blue = health-related.
On the digital health supply side, we see $billions of investments flowing into hospital-to-home and patient self-care technologies from wearable devices to Internet-of-Things populating the home (e.g., voice tech, smart medication dispensers, and remote health monitors).
The sustainable nursing workforce is so central as a critical success factor — a must-have — for the future sustainable health care system.
In Latin, the phrase I could use would be “sine qua non.” That translates to, “without which, there is nothing.”
That is exactly what we need to understand about the nursing workforce. Without this precious form of health care human capital, there cannot be a sustainable health/care system that scales care to every single health citizen.




 Thank you FeedSpot for
Thank you FeedSpot for