There’s more evidence that doctors and patients, both, want to use telehealth after the COVID-19 pandemic fades.
 Doximity’s second report on telemedicine explores both physicians’ and patients’ views on virtual care, finding most doctors and health consumers on the same page of virtual care adoption.
Doximity’s second report on telemedicine explores both physicians’ and patients’ views on virtual care, finding most doctors and health consumers on the same page of virtual care adoption.
For the physicians’ profile, Doximity examined 180,000 doctors’ who billed Medicare for telemedicine claims between January 2020 and June 2021.
Telemedicine use did not vary much across physician age groups. Doctors in specialties that manage chronic illnesses were more likely to use telehealth: endocrinology (think: diabetes), gastroenterology, rheumatology, urology, nephrology, cardiology, ENT, neurology, allergy, and hematology/oncology were the top 10 adult specialties using telemedicine in Doximity’s research.
Doximity asked physicians an important question on trust: that is, whether telemedicine could bolster trust with patients, especially those who have long been under-served by the healthcare system.
Two in three physicians said that access tot Lee medicine helped to build or maintain trust with patients.
One direct quote from a physician illustrates the upside of telehealth and trust:
“Building trust requires a human connection and genuine empathy/compassion. If we can demonstrate that with our words and time, trust can be built even via video,”
Dr. Maulik Patel, a specialist in Geriatrics, told the Doximity team.
For the patients’ insights, Doximity surveyed 2,000 people, 1,000managing chronic conditions and 1,000 who were not.
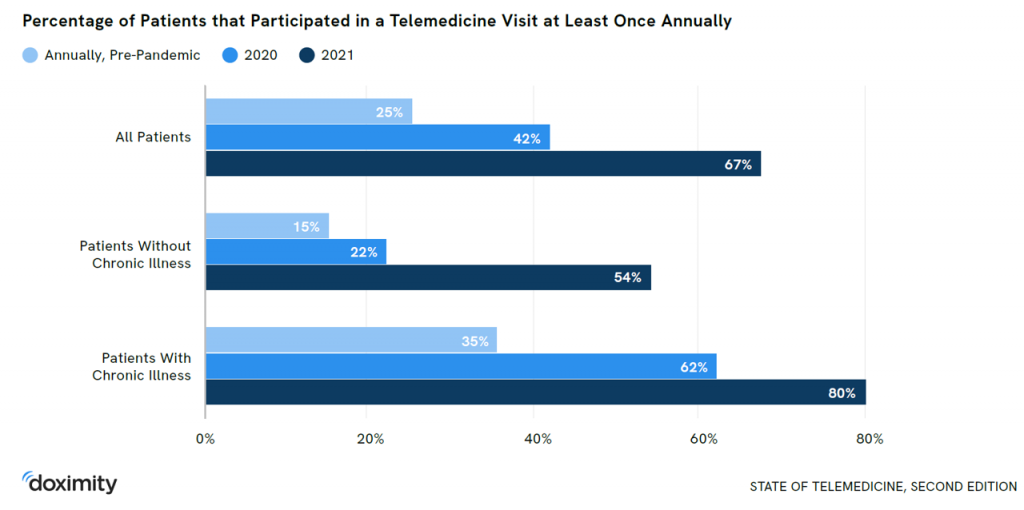 Two-thirds of all patients had at least one telemedicine visit in 2021, compared with 42% in 2020 and 25% before the pandemic. Within each patient category:
Two-thirds of all patients had at least one telemedicine visit in 2021, compared with 42% in 2020 and 25% before the pandemic. Within each patient category:
- In 2021, 80% of patients with chronic conditions participated in at least one telemedicine visit, compared with 62% in 2020 and 35% pre-pandemic.
- Over one-half of people without chronic illness had at least one telehealth visit in 2021, versus 22% in 2020 and 15% before COVID-19 emerged.
“For the majority of patients, telemedicine is now a part of the new normal in healthcare,” the report asserts.
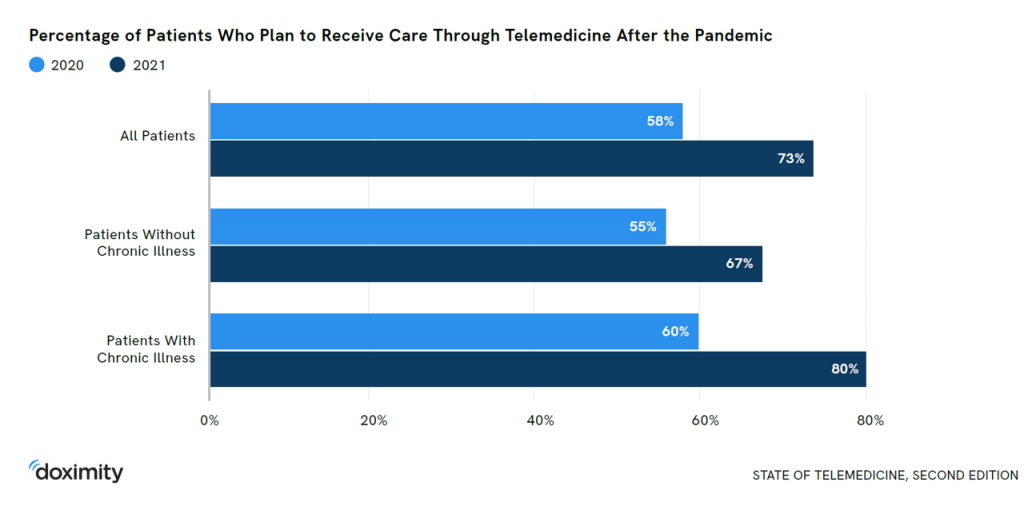 Doximity is bullish on the persistence of telemedicine post-pandemic, finding that 73% of all patients plan to receive care virtually “after the pandemic.” Even two-thirds of people without chronic illness plan to use telehealth post-pandemic.
Doximity is bullish on the persistence of telemedicine post-pandemic, finding that 73% of all patients plan to receive care virtually “after the pandemic.” Even two-thirds of people without chronic illness plan to use telehealth post-pandemic.
More patients view telemedicine’s quality on-par or better than receiving care in-person, the study found. This was especially true for patients managing chronic health issues, 63% of whom felt virtual care provided equivalent or superior quality of care versus in-person visits.
Having found a general consumer embrace for virtual care, though, Doximity found that most patients would still prefer to wait one to three days to see their current doctor “rather than a new doctor immediately.”
Most consumers would prefer a mobile device for telemedicine visits (59%) rather than use a laptop or desktop computer (38%). “Since 85% of Americans already own a smartphone,” the report notes, “telemedicine can help bridge the digital divide in medicine.”
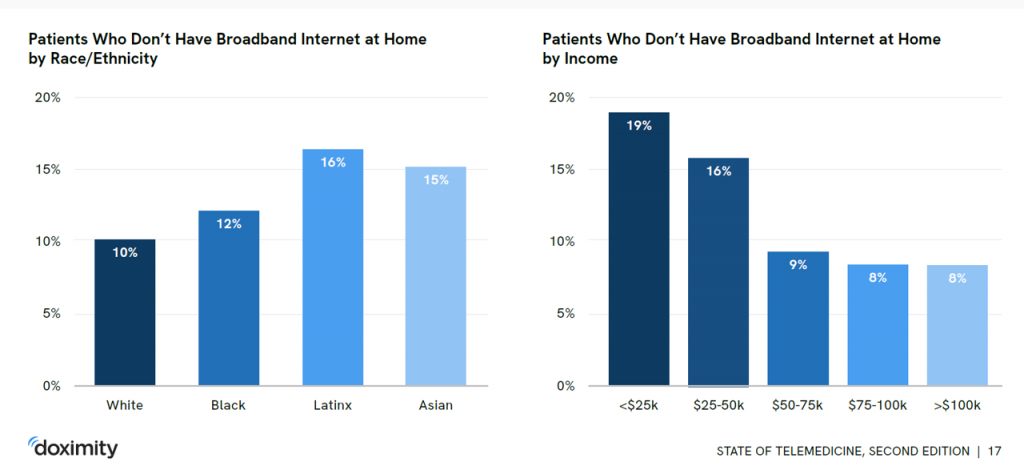 That is, for patients who have access to a mobile phone as well as broadband connectivity. The report rightly points out that lack of connectivity is a barrier to receiving virtual care. People of Hispanic ethnicity and people with lower annual incomes (under $50,000) more likely lack broadband internet at home. This aspect of health equity was made quite clear during the pandemic, and has been part of a larger constellation of social determinants of health contributors to health disparities in the U.S.
That is, for patients who have access to a mobile phone as well as broadband connectivity. The report rightly points out that lack of connectivity is a barrier to receiving virtual care. People of Hispanic ethnicity and people with lower annual incomes (under $50,000) more likely lack broadband internet at home. This aspect of health equity was made quite clear during the pandemic, and has been part of a larger constellation of social determinants of health contributors to health disparities in the U.S.
Audio-based telehealth — phone calls — are an important bridge to that virtual care access gap, the report points out, calling out that Latino patients are more likely than white patients to have had audio-only telemedicine visits.
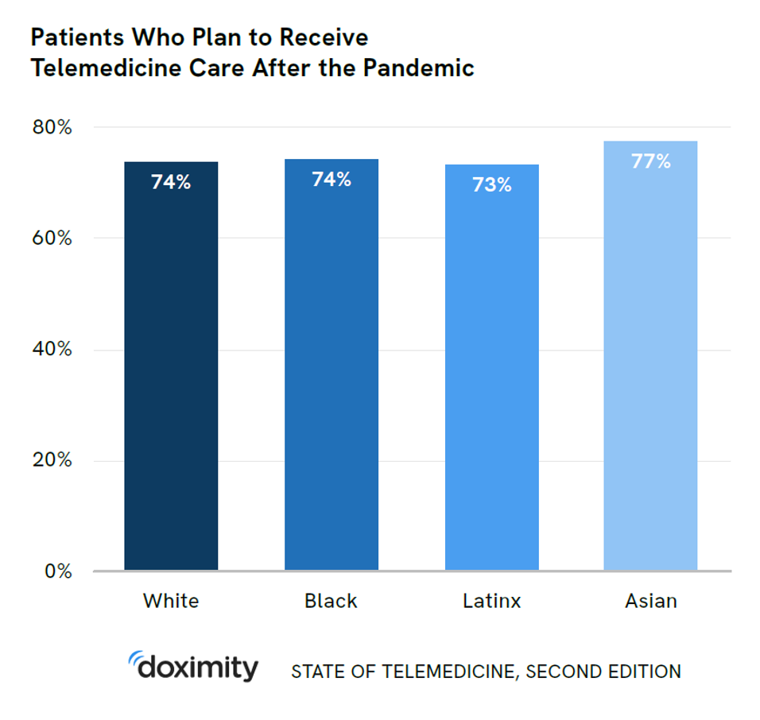
 Health Populi’s Hot Points: There’s a striking end-note to the report on patients who plan to receive telemedicine care after the pandemic, with consumer data by race/ethnicity.
Health Populi’s Hot Points: There’s a striking end-note to the report on patients who plan to receive telemedicine care after the pandemic, with consumer data by race/ethnicity.
Striking, because virtually the same percentage of patients who are White, Black, Latinx, and Asian all plan to use telehealth after the pandemic, shown in the graphic at the top of this post.
That includes 74% of White people, 74% of Black people, 73% of Latinx people, and 77% of Asian people in America.
“Taken together,” Doximity concludes, “these findings reinforce that historically marginalized groups will use telemedicine when it is accessible.”
The promise of telehealth expansion, when assurance for connectivity/broadband, affordable data plans, and delightful design that engages people as their unique selves, is that virtual care could help address health disparities and be that open, trusted front-door for primary care and care for people managing chronic conditions.
As Ann Mond Johnson, CEO of the ATA has remindsed us, “Telehealth IS health.”
At the upcoming ATA Annual Meeting, there will be a focus on creating a hybrid model for “everyday care.”
Health care’s evolution toward “hybrid” is analogous to what we are seeing at the workplace and in retail, venues evolving to meet people where we “are” in an omnichannel mode.
“Hybrid” is part of our popular culture and daily lifestyles now.
We know that health and wellbeing are made where we live, work, play, pray, learn, and shop.
And so with healthcare, everywhere, we see the same phenomenon.
Call it the New HomeCare, Digital Front Doors to Health, or Healthcare in Your Hand. Telehealth care is healthcare.

Or, borrowing the phrasing of the Whirlpool Corporation which sees clean laundry as a social determinant of wellbeing and students’ education,
“Every day, care.”





 Grateful to Gregg Malkary for inviting me to join his podcast
Grateful to Gregg Malkary for inviting me to join his podcast  This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're
This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're