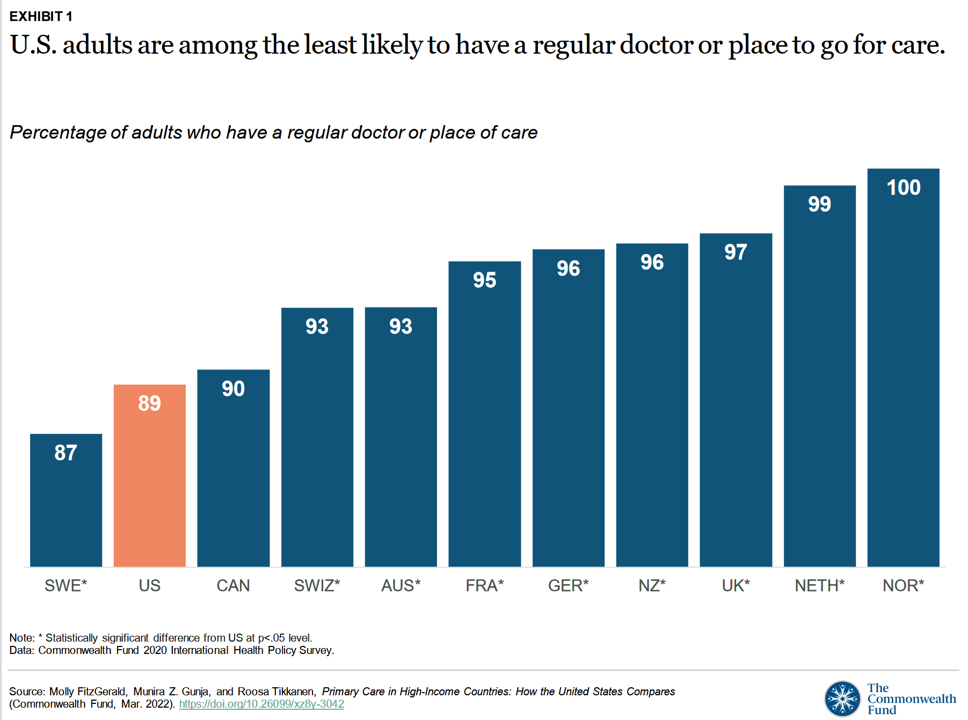
Compared with health citizens living in other wealthy countries, people living in the U.S. are still among the least likely to have a regular doctor or place to go for care.
Thus, millions of Americans continue to lack access to primary care compared with peers in other nations, according to a report from The Commonwealth Fund.
The Commonwealth Fund has tracked primary care access for many years, and over time has found the United States to lack the kind of primary care “backbone” that many wealthy nations have — whose health citizens also enjoy much better health outcomes that relate to easier access to health care. [The link in the previous sentence will take you to my post on the Fund’s 2009 report, citing a déjà vu experience of evidence that sounds all too similar to the 2022 profile].
The 2022 Fund report, Primary Care in High-Income Countries: How the U.S. Compares, assesses four aspects of primary care for health citizens living in eleven wealthy nations:
- Accessibility
- Continuity
- Comprehensiveness
- Coordination.
The high-income nations surveyed include Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the United Kingdom, and the United States.
Related to the likelihood of having an ongoing place to receive health care, Americans are also the least likely people to have a longstanding relationship with a primary care provider; only 43% of people in the U.S. have a PCP relationship, compared with 71% of health citizens in Germany and the Netherlands.
Access to primary care, or lack thereof, can also be measured in terms of a patient’s ability to see a primary care provider after “regular office hours,” in the phrasing of the Fund’s survey. Only 45% of U.S. PCPs reported offering after-hours arrangements for their patients seeking care “off-hours.”
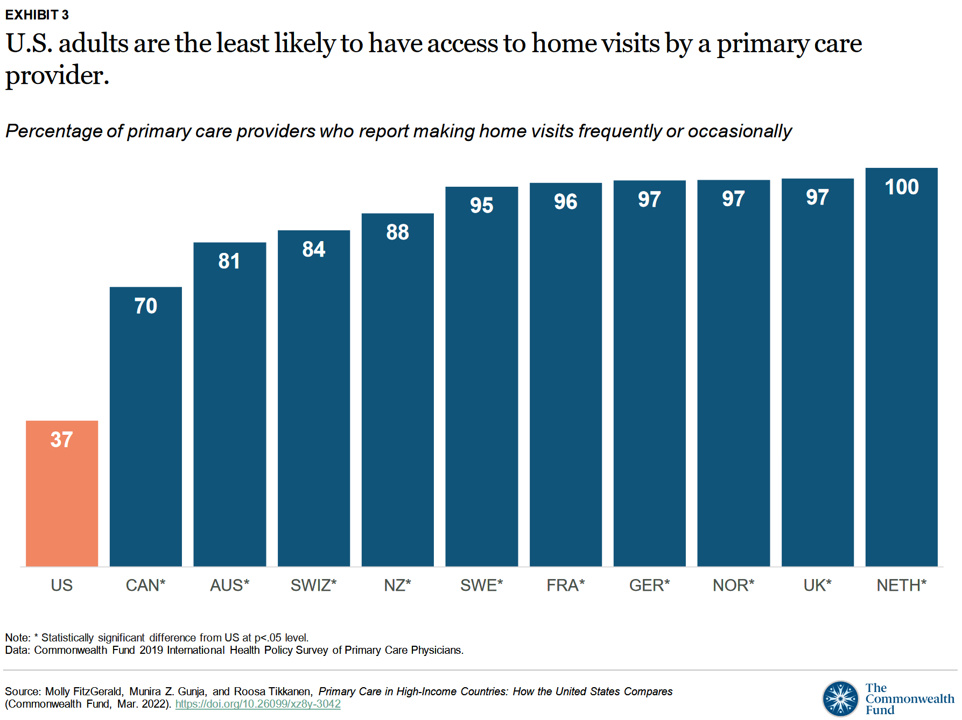
Next, check out the second bar chart here showing American PCPs’ huge gap in providing home visits compared with doctors in the ten other countries studied.
Only one in three U.S. PCPs offer some sort of home visit in contrast with 70% of Canadian physicians — the second-lowest position in this table — 81% of Australian doctors, all the way up to 100% of Dutch PCPs making home visits.
 There are other important metrics in the Fund’s report that illustrate primary care gaps in the U.S.
There are other important metrics in the Fund’s report that illustrate primary care gaps in the U.S.
I’ll point to one that’s become a key learning in the wake of the COVID-19 pandemic, which is mental health care. Only one-third of PCPs in the U.S. have a mental health provider in their practice, compared with 9 in 10 Dutch and Swedish primary care practices.
The third chart illustrates that the U.S. is not alone in under-serving patients for mental health access compared with other high-income countries. The U.S. ranks higher on this measure than Germany, Switzerland, and Norway.
It is important to note that the U.S. ranks highest for the metric of PCPs likely to screen patients for social needs — at 30% of PCPs doing so. This proportion is higher than France at 29% of PCPs screening for social needs, 25% of German doctors, 22% of Canadians, 21% of British physicians, and 20% of Swedish PCPs.
The Fund’s report discusses this finding, recognizing that,
“In some countries, like the United States, higher rates of receiving such information may be a response to higher rates of material hardship, along with a weaker social safety net. In addition to having universal health care, robust welfare states like Sweden offer free or low-cost education, subsidized childcare and transportation, generous parental leave policies, and guaranteed pension payments,”
and
“PCPs in Canada and the U.S. are the most likely to have social workers on their care teams, while this is almost never the case with German or Swiss PCPs. The relatively higher rate of social workers on U.S. primary care teams may be a function of underinvestment in certain types of social services. For example, comparatively less U.S. funding is directed to meeting the needs of young and working-age people through early childhood education and parental leave allowances.”
The Commonwealth Fund offers several policy prescriptions for the U.S. to consider in bolstering a strong primary care backbone for the nation’s health citizens:
- To narrow the wage gap between primary care/generalist doctors and specialists, noting that the U.S> has the highest tuition fees for medical schools across the countries as well as the largest wage disparity.
- To invest in telehealth that provides an on-ramp for patients to access primary care, especially important for rural residents and people with lower incomes.
- To expand payment reforms rewarding health care providers accountable for continuity of care (and outcomes).
- Embracing and embedding social services by expanding our definition of health and well-being. More U.S. patients are concerned about social needs than health citizens in Germany, the Netherlands, Norway, and Sweden — four countries that allocated resources for social care complementing medical services.
The Fund concludes its discussion of the primary care data, finding this year’s report “consistent with prior research” for the U.S. — “an outcome of chronic underinvestment in primary care in the United States,” the Fund asserts. The continued underinvestment in America’s primary care backbone also falls disproportionately on communities of color and residents in rural U.S. communities, worsening health disparities that grew in the COVID pandemic.
Health Populi’s Hot Points: Two obvious places for our Hot Points to focus her are the issues of front-loading mental health and social care into primary care, and how to re-imagine primary care placing people/patients at home in the center of that dynamic.
These issues are not mutually exclusive: if we take a value-based, ecosystem view on them, we can leverage technology to help scale social and public policy goals to ensure that health is baked across all policies.
I pointed this out in my book, HealthConsuming: from health consumer to health citizen, noting that the U.S. has historically allocated an inverse proportion of spending on medical care compared with social care. Here’s a chart from the book making that point:
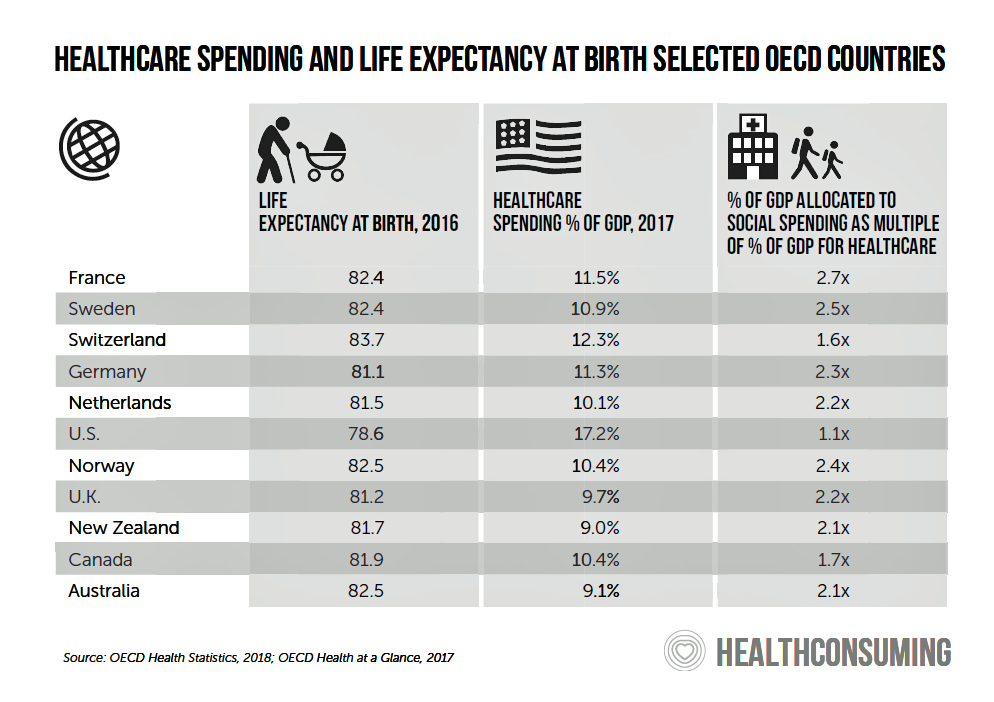
Since this chart was published, life expectancy in the U.S. has actually declined, notwithstanding health care spending nationally exceeding $4 trillion — more than any other country on Earth spends on their national medical line-item.
An intriguing look at ESG goals (environmental, social, governance) was published earlier this month in Fortune by Michelle Williams and Patricia Geli, making the case to add “H” — “health” — to the “ESG” abbreviation.
Michelle and Patricia, both affiliated with the Harvard Chan School of Public Health, are also part of the Reform for Resilience Commission, a global collaborative focused on bolstering a resilient and equitable health care system beyond COVID-19.
Adding the fourth element of health to ESG, these advocates argue, would…That’s where the ESG framework provides a model. We must make protecting and promoting health every bit as essential as environmental, social, and governance principles for any business looking to win favor with customers, investors, and employees.
In summary that translates to, in the authors’ words, “Care for the team, care for the community. and care for society.”
They believe that, “We must nurture the mindset that protecting wellbeing is a private-sector responsibility.”
In the U.S., H+ESG makes so much sense for the private sector and investment community because at least one-half of health care spending is borne by the private sector through employer-sponsored health insurance. This is why we have already seen private sector companies adopting new forms of primary care models and incentives, from Amazon (for Care and telehealth to prescription drugs and Prime for SNAP beneficiaries) to Walmart, which continues to grow its health and wellness business.
Telehealth and virtual care, with embedded mental health on-ramps, will help to scale primary care access. Designing privacy and health equity into these programs will be key to rebuilding America’s primary care backbone so that, perhaps by 2027, the Commonwealth Fund update report in this series will see the U.S. moving up and to the right of primary care access, continuity, comprehensiveness, and coordination.





 Grateful to Gregg Malkary for inviting me to join his podcast
Grateful to Gregg Malkary for inviting me to join his podcast  This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're
This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're