Doctors heads and hearts are jammed with concerns beyond curing patients’ medical conditions: U.S. physicians are worried about big social issues, according to a Medscape survey report, Physicians’ Views on Today’s Divisive Social Issues 2022.
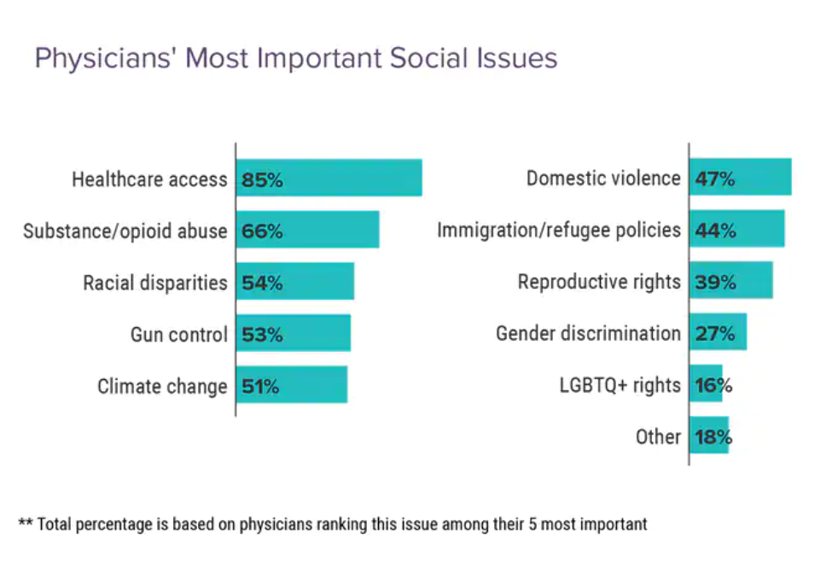
Topping physicians’ list of their top-five most important social issues, far above all others ranked healthcare access.
Underneath that top-line statistic, it’s important to note that:
- 52% of doctors are “very concerned” about healthcare access,
- 28% are “concerned,” and
- 13% are “somewhat concerned.”
Medscape underscores that in 2020, 31 million U.S. residents had no health insurance coverage, and another 38 million people were enrolled in “inadequate” health plans — deemed to be “under-insured.”
This has led to some patients avoiding care due to cost – for doctors’ visits, treatment for chronic conditions, recommended tests, or prescription drug fills.
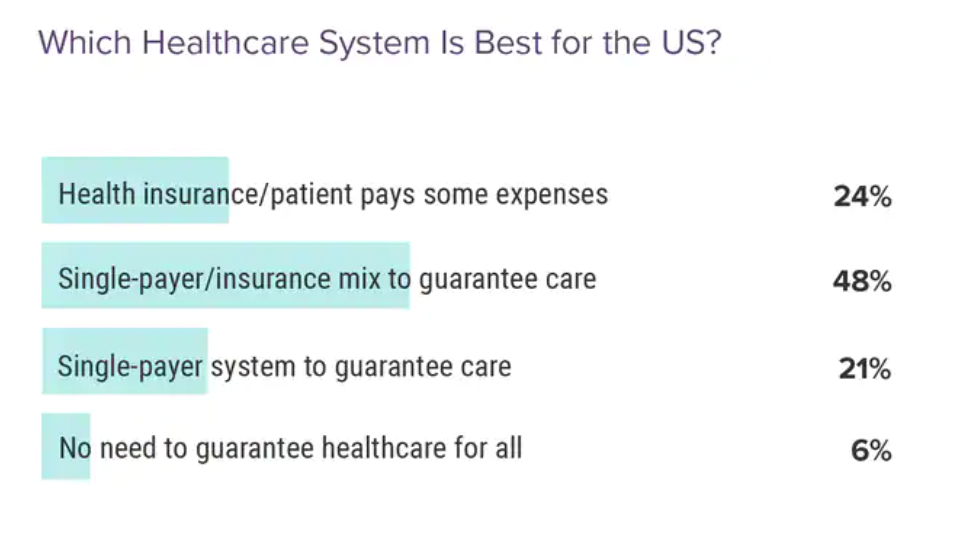
Nearly one-half (48%) of U.S. physicians believe that a single-payer combined with insurance coverage would be the best healthcare system for the country.
One in 4 support a health insurance system where patients pay “some expenses,” and 21% view a single-payer system that guarantees care-for-all to be the bet system.
Only 6% of doctors said there is no need to guarantee healthcare for all.
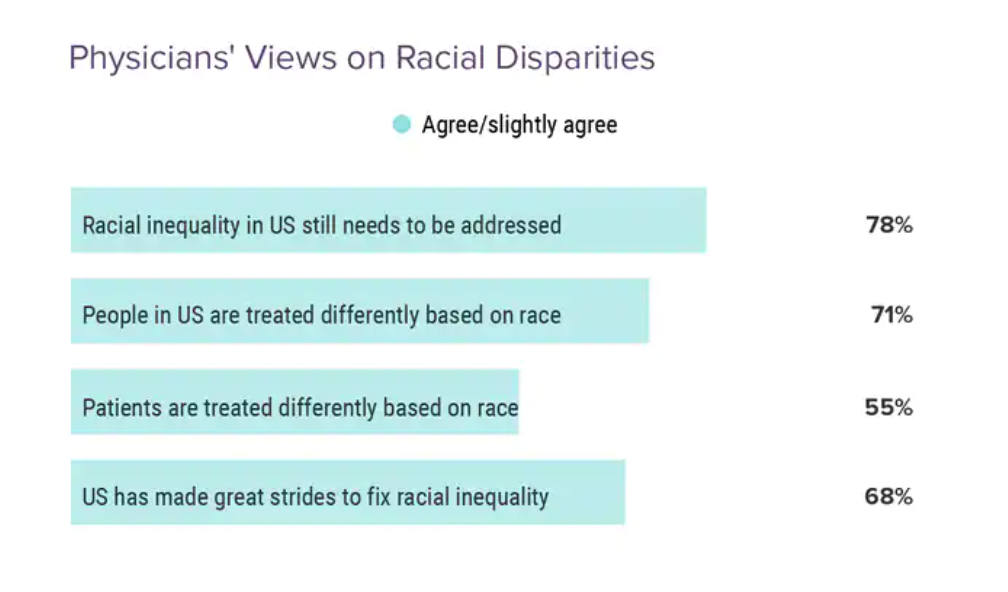
Over one-half of physicians ranked racial disparities a top-5 social issue.
Regarding racial disparities,
- 78% of doctors agreed that racial inequality in US still needs to be addressed and
- 68% of doctors said that the U.S. has made great strides to fix racial inequality.
Check out the two middle bars in the chart, showing that 71% of doctors saying people in the U.S. are treated differently based on race, but 55% thought that patients are treated differently based on race.
The implication here is that physicians believe the health system treats people more equitably across race and ethnicity than general society does.
We can’t stop at healthcare access and health equity in our understanding of and empathy with physicians’ social/health concerns.
Substance abuse continues to be a top-five concern for 2 in 3 doctors practicing in the U.S.
Several other very current and profoundly personal front-of-the-media and family life issues also rank high in doctors’ top-five social issue concerns: gun control, domestic violence, and reproductive rights.
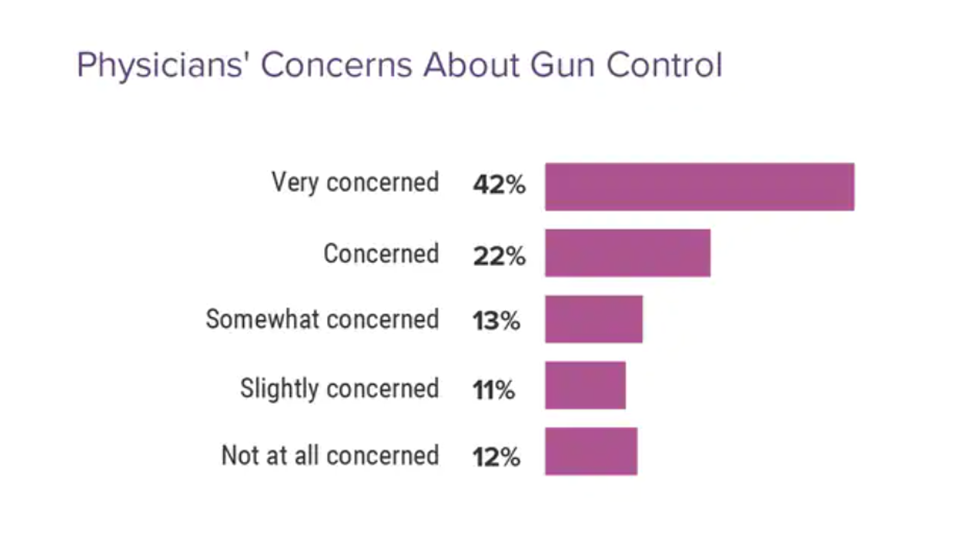
64% of doctors are “very concerned” or “concerned” about gun control.
Following the Uvalde, Texas, school shootings, many healthcare advocacy organizations, professional societies, and health system executives came out loud, clear, and assertive about the role of guns in public health and impact on the health system.
As one example, Dr. James Madara, CEO of the American Medical Association, wrote a letter to the U.S. House Committee of the Judiciary leads Rep. Jerrold Nadler (D-)) and Rep. Jim Jordan (R- ) imploring Congress to take immediate action to address the epidemic of gun violence in America:
“On behalf of the physician and medical student members of the American Medical Association (AMA), I am writing to express our strong support for H.R. 7910, the “Protecting Our Kids Act,” an omnibus package of eight previously introduced bills focused on preventing firearm violence. In addition to the horrific massacres within ten days in Buffalo and Uvalde, there have been at least 17 mass shootings in the past week across the country according to the Gun Violence Archive….Gun violence is a public health crisis, and as with other public health areas, evidence-based interventions are needed for reducing deaths and injuries. As physicians, our mission is to heal and to maintain health. Most firearm injuries and deaths are preventable.”
These words were written on June 1st, 2022….just when yet another such event was happening in Oklahoma.
Marking the 233rd mass shooting in America on June 1, 2022, five people died due to gunshot wounds at a Tulsa medical center.
Note that the Medscape study was fielded between late January and early March, 2022.
At that point, 96% of doctors in the study agreed with the policy of requiring background checks to own firearms, 90% that only someone 18 or older should own a firearm, and 70% requiring a psych evaluation to own a firearm.
Health Populi’s Hot Points: This Medscape study into physicians’ thoughts and feelings complements other research the organization has conducted with doctors earlier this year: specifically, the Medscape Physician Burnout & Depression Report 2022, which I covered in Health Populi here in January 2022.
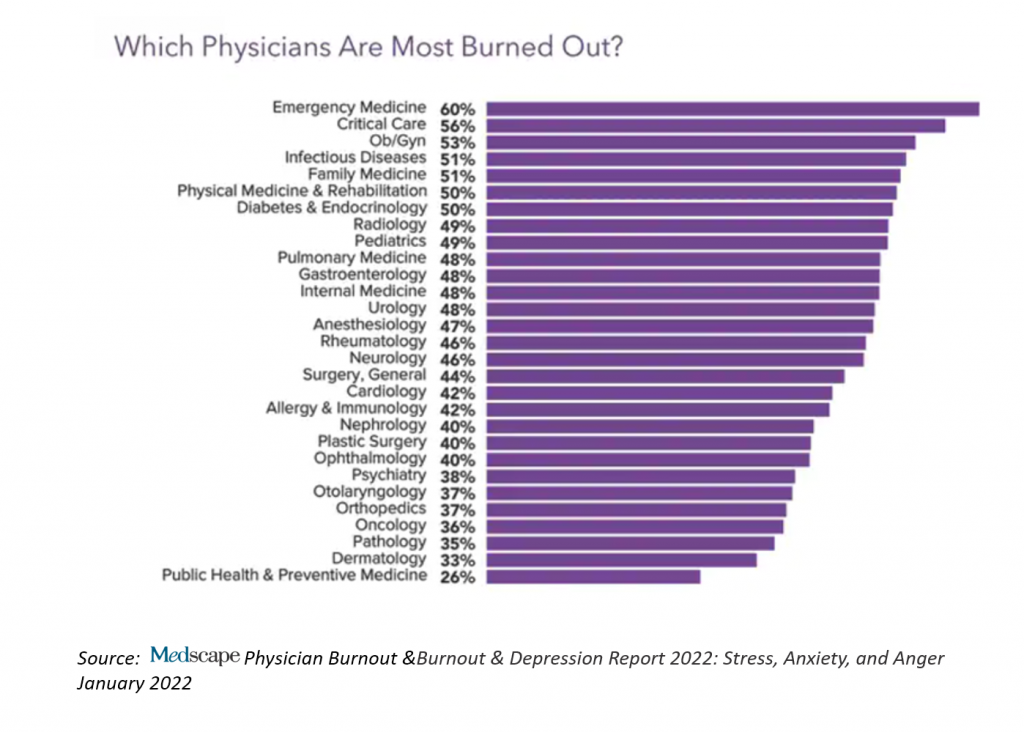
The study discovered a five percentage point increase in physician burnout, growing from 42% in 2020 to 47% in 2021 — especially acute for emergency department physicians, rising 43% in burnout to 60% in 2021.
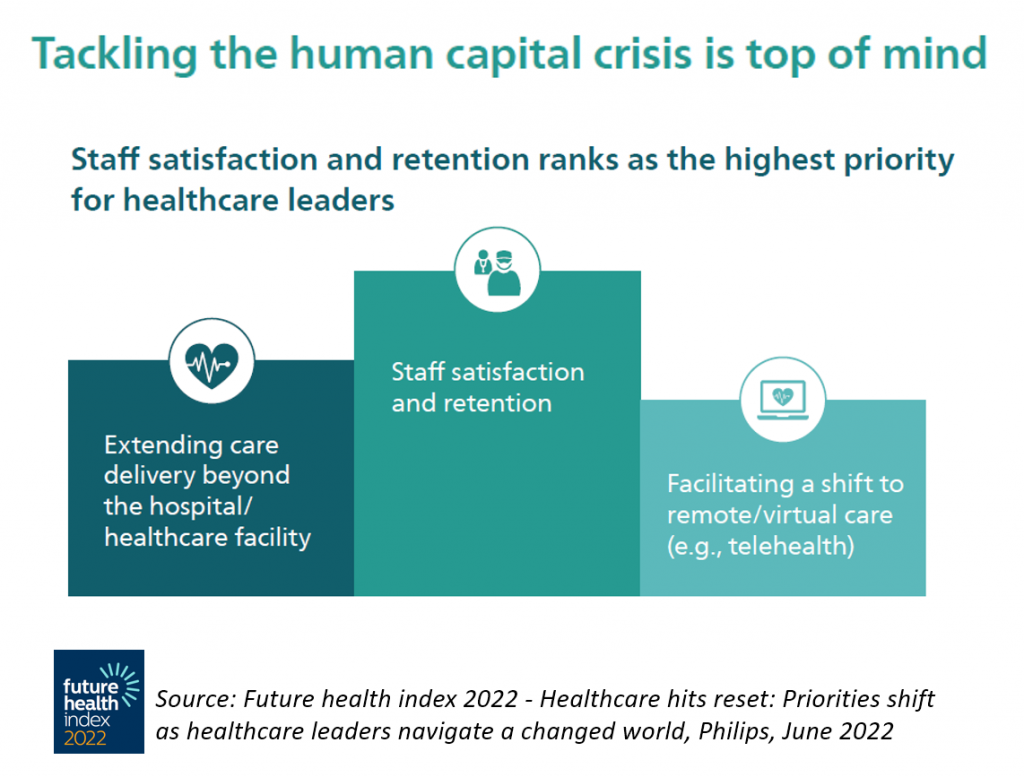
In the just-released Philips Future Health Index 2022, the study conducted among some 3,000 healthcare leaders in 15 countries identified 3 key priorities to, in the words of the report, “navigate a changed world.”
The first of these priorities is Emerging from the pandemic, healthcare leaders reassess their needs.
And the first must-do tactic underneath this strategic pillar is that healthcare leaders refocus on staff satisfaction and retention.
This imperative recognizes that tackling healthcare’s human capital crisis is top of mind among those who lead healthcare enterprises. The Great Resignation has had real, material impacts in health systems the world over.
In the U.S., the growing use of traveling nurses, for example, has led to greater labor costs, eroding financial operating margins and some hospitals’ fiscal viability.
This chart comes from the Philips report, noting that staff satisfaction and retention is the highest priority for healthcare leaders.
The Medscape studies (both the latest report discussed here on social issue concerns, and the previous study into physicians’ states of mind and burnout) illustrate the mental health and collective mood of doctors. Philips reminds us to put this priority on our front-burners, top-of-mind.
All the predictive analytics and well-intended and -organized data collection (pillars 2 and 3 in the Philips report) cannot supplant this first priority: our need to nurture, value, and protect healthcare’s human capital.
For a comprehensive look at staff shortages of clinicians in the U.S., check out Dylan Scott’s essay in Vox from April 7, 2022, America needs more doctors and nurses to survive the next pandemic.
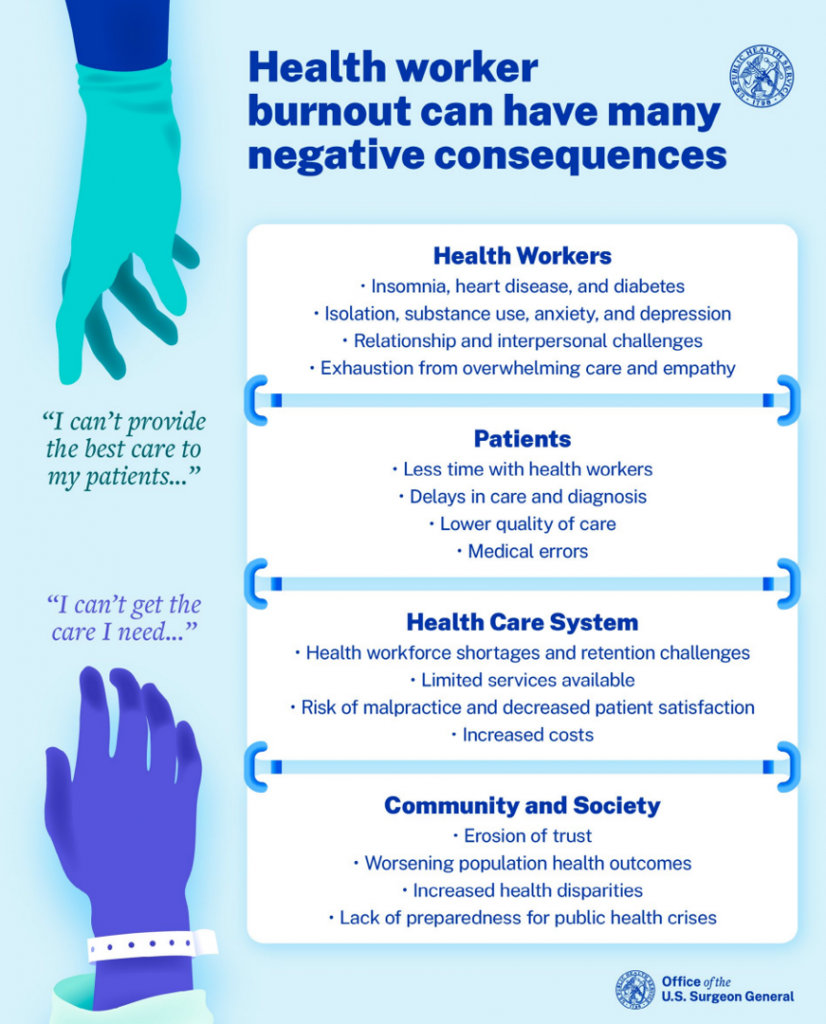
And if you don’t believe either Dylan Scott or me, perhaps the Surgeon General Dr. Vivek Murthy will convince you in his new report, Addressing Health Worker Burnout.
In particular, check out the sections on
- What technology companies can do – learning from the unintended errors/consequences of non-interoperable electronic health records and apps and digital health tools that distance providers from patients instead of empowering and enabling these relationships (from page 42); and,
- What friends, families, and communities can do to lift up our precious human capital of clinicians — physicians, nurses, pharmacists, allied health professionals, and of course, family caregivers (beginning page 52).
Dr. Murthy concludes with an ask and a hope:
“Will we step up, and meet our moral obligation to care for those who have cared for
us? It won’t be easy. Many of the recommendations in this Advisory require significant
structural change and sustained investment. They will take time and require our
continued attention and action.
But the hope of health workers has endured through far worse. Our efforts must
as well.”




 Thank you FeedSpot for
Thank you FeedSpot for