 Health care cost increases are unsustainable the world over; in developed nations, the forecast is even more dire given exploding demand for health services as citizens age. Cisco polled senior leaders in health systems globally to gauge their views on the challenging state of health care in their respective nations, and prospects for health system improvement.
Health care cost increases are unsustainable the world over; in developed nations, the forecast is even more dire given exploding demand for health services as citizens age. Cisco polled senior leaders in health systems globally to gauge their views on the challenging state of health care in their respective nations, and prospects for health system improvement.
The triple-mantra for senior health leaders is access, efficiency, and quality. Access takes the form in this survey in maldistribution and insufficient number of health professionals. Efficiency looks like patients referred for unnecessary care coupled with long lines (queues) for needed services. Quality measurement continues to challenge all nations, as discussed in Cisco’s survey report, The Health of Nations: Perspectives from Global Leaders Reveal Untapped Opportunity.
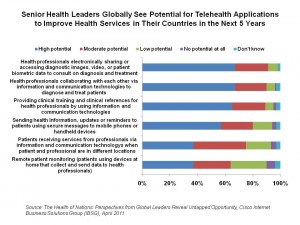
How to address these issues? Well, this is Cisco’s research, so it’s focused on information technology solutions to solve these problems. Specifically, telehealth: the application of connectivity between patients, providers and experts that aren’t in the same place at the same time. The chart illustrates several key telehealth approaches that a majority of senior health leaders find promising including:
- Health professionals electronically sharing/accessing patients’ health information such as images, video and biometric data for consult on diagnosis and treatment
- Clinicians collaborating with each other via technology to diagnose and treat patients
- Providing training and clinical references for clinicians via telehealth connections
- Sending health information and reminders to patients via mobile phones and handheld devices
- Patients receiving services remotely from clinicians and consultants
- Remote patient monitoring.
Cisco identifies several national programs that could be ‘game-changing’ in using communications and information technology to improve health care delivery for access, efficiency and quality: Centers of Excellence, which could be accessible to local and more remote communities via telehealth infrastructure; Community Health Workers supported by telehealth; and, surge capacity required due to national emergencies (e.g., earthquakes, tsunamis, disease pandemics) enabled by telehealth.
Health Populi’s Hot Points: The #1 global priority cited by senior health leaders was ‘equitable access to health services,” well over affordability of that health care. “Services our country can afford” ranked fifth in a long list of priorities, compared with 34% of leaders saying that equitable access to health services was Job #1. This survey didn’t show results by country, so it’s not possible to parse out where the U.S. stood on the issue of access vs. equity: a current chasm in America’s political tug-of-war on health reform.
What is universal, though, is a fact that Cisco calls out with which I agree: that governments and health leaders must lead in building information/communications technology infrastructure to get to that access/efficiency/quality Holy Grail in health. The scale of infrastructure investment and expanse requires government intervention — even in an era where one-half of Americans might detest the concept of “Big Government” and government intervention in general. The FCC Broadband report articulated the value argument for such investment for national health. But government can’t do this alone: private-public partnerships can build new ways of providing health services, with 8 in 10 senior health leaders identifying this as a crucial strategy to imrove health service delivery in their countries. What stands in the way is the lack of broadband infrastructure and agreed standards for interoperability.p
Cisco suggests a migration path, beginning with connecting clinicians to collaborate for diagnosis and treatment enabled by telecommunications and IT. The second phase they see is the adoption of telehealth clinical services for patients, followed by remote health monitoring. I would suggest that the patient/health citizen must be in the center of that first phase of connecting clinicians. Why can’t remote monitoring be integrated sooner into this scenario? Getting patients into self-care and engagement mode would bring that under-utilized resource — the patient himself — into care collaboration. And that can get to greater access, efficiency and quality goals that every nation eyes.





 Grateful to Gregg Malkary for inviting me to join his podcast
Grateful to Gregg Malkary for inviting me to join his podcast  This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're
This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're