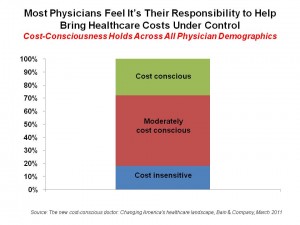
 Doctors practicing in the U.S. are becoming increasingly conscious of the increasing costs of health care. Most consider themselves cost-conscious, and are considering the impact of their practice patterns — in terms of prescribing medicines, tests, and procedures — on the nation’s health bill. In fact, most physicians feel they have a responsibility to bring down health costs.
Doctors practicing in the U.S. are becoming increasingly conscious of the increasing costs of health care. Most consider themselves cost-conscious, and are considering the impact of their practice patterns — in terms of prescribing medicines, tests, and procedures — on the nation’s health bill. In fact, most physicians feel they have a responsibility to bring down health costs.
This perspective on physicians comes from the survey report, The new cost-conscious doctor: Changing America’s healthcare landscape, from Bain & Company, published in March 2011. Bain spoke with over 300 U.S. physicians to assess their perspectives on managing costs, drug and device usage, and standardized care protocols.
The top-line finding is that, regardless of physician demographic — whether male or female, salaried or productivity-based, specialist or generalized, urban or rural, young or mature, doctors uniformly see that they must change clinical practice patterns to accommodate the realities of health economics.
The impacts of this on the practice will be many, including:
- Consolidating practices, increasingly being absorbed into hospital systems
- Decreasing utilization as a direct response to incentives
- Promoting preventive care
- Adapting to standardized treatment protocols.
Health Populi’s Hot Points: Bain rightly points out that these changed physician attitudes and behaviors will ripple through the health supply chain on to life science, medical device, pharmaceutical and technology companies. Organizations in these health supply segments must demonstrate value to physicians and patients in the larger health ecosystem in order to be adopted into clinical practice.
That physicians see cost management as part of their jobs now means that their decisions will be increasingly impacted by their collective cost consciousness lens. Accountable care models, medical homes and more tightly integrated delivery networks will bolster this approach and tightly focus that cost conscious lens. Physicians will be less inclined to try out new-new products without firm proof-of-concept and references from peer physicians who are influencers in their field. Over one-half of physicians told Bain that they’d be using comparative effectiveness analyses within 2 years.
Furthermore, physicians are growing more comfortable with practice protocols and standardized care, Bain found. They’re using clinical guidelines more often in 2011 than 5 years ago; this is especially true of younger physicians, who more often refer to practice guidelines for patients. The mass adoption and full implementation of electronic health records will enable such protocols to be pushed to clinicians at the point-of-care. In fact, physicians expect a five-fold increase in the prevalence of electronic access to clinical treatment guidelines, and an 8-fold increase in pay-for-performance programs.
For manufacturers in the health supply chain, the major challenge is to develop and market products that help lower the costs of health care. That’s the new definition of “innovation” in health care.




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a