 Economic challenges have forced 8 in 10 hospital CIOs to cut IT spending by about 10%. At the same time, these CIOs realize that penalties are looking in 2011 if they fail to implement “meaningful use” of EHRs.
Economic challenges have forced 8 in 10 hospital CIOs to cut IT spending by about 10%. At the same time, these CIOs realize that penalties are looking in 2011 if they fail to implement “meaningful use” of EHRs.
This is the Rock and a Hard Place PricewaterhouseCoopers (PwC) describes in the report of the same name.
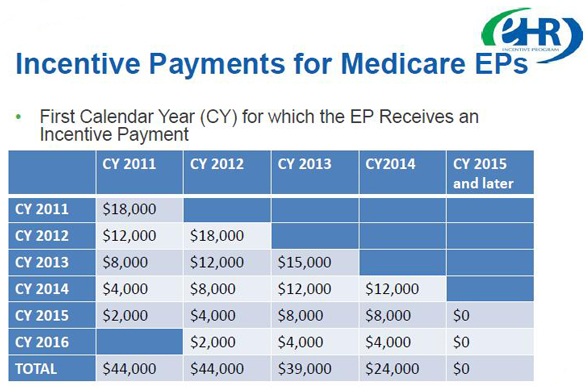
PwC believes that the “stick” of Medicare payment penalties will be more compelling than the “carrot” of HIT incentives provided by the HITECH funding: based on the firm’s calculations on modeling the funding for providers, the report asserts that, “the stimulus funding for health IT is a small carrot compared to the amount of resources it will take to deploy this technology over the next five years. Also, providers will feel a big stick of financial penalties if they fail to use government-certified electronic health records (EHRs) in a certified manner beginning in 2015.
Hard EHR software costs per physician, including implementation and training, would range $33,000 to $60,000, according to PwC’s analysis (shown in the table above). Adding in interface, reporting, and software maintenance for 2 years, total costs per physician would range from $61,250 to $104,000.
For hospitals, there’s a huge stick to consider. PwC’s model is based on a scenario of a 500-bed hospital providing 2.5% of its $1.2 annual billion in charges in charity care; an average of 26,000 annual discharges; and, 62,500 total Medicare inpatient days. In total, the hospital would receive $2.4 mm in 2011, and overall, $6.1 million.
On the other hand, check out the second chart, above. This illustrates PwC’s estimates on average Medicare reimbursement losses for 500-bed hospitals that do not implement a government-certified EHR. By 2017, the 500-bed hospital that does not meet meaningful use standards would lose as much as $3.2 million.
Thus, PwC sees the “stick” as being more compelling than the “carrot” of incentives, when comparing the two.
Health Populi’s Hot Points: A key issue with the HITECH Act is something we learned with ePrescribing (eRx): the benefits of the eRx, as with EHR implementation, don’t directly or immediately accrue to the providers implementing the technology. The benefits accrue to payers, both private (employers, etc.) and public (Medicare and Medicaid).
Furthermore, ongoing implementation costs for both hospitals and physicians will out-weigh the incentive amounts. These economic realities of implementation shouldn’t be glossed over when providers are making EHR investment decisions. A full-cost approach, such as life-cycle costing, should be adopted by those entering this murky, but essentially mandated, investment ‘decision.’





 Gil Bashe, Chair Global Health and Purpose with FINN Partners,
Gil Bashe, Chair Global Health and Purpose with FINN Partners,  Grateful to Gregg Malkary for inviting me to join his podcast
Grateful to Gregg Malkary for inviting me to join his podcast