The new mantra for employers who sponsor health benefits is: “a healthy workplace leads to a healthy workforce.”
Employers that sponsor health plans are now in the behavior change business, according to Aon’s 2011 Health Care Survey. Health plans are tightly focusing on wellness, motivating and sustaining positive personal health changes, with carefully designed incentives (carrots and sticks) informed by behavioral economics. The paradigm is value-based insurance design (VBID) that removes barriers to essential, high-value health services to bolster treatment adherence, improve productivity, and reduce overall medical costs.
The top five priority tactics for employers in health are:
- To offer incentives or disincentives to motivate sustained health care behavior change, cited by 73% of employers
- To promote a culture of health in the workplace, noted by 62% of businesses
- To offer and promote disease management programs, 46%
- To promote other consumer-driven plan strategies, 42%. While PPOs still rank the most popular plan type, high-deductible health plans are gaining traction growing 11 percentage points since 2010. 41% of employers are offering HDHPs in 2011 — the same percentage as offering HMOs.
- To focus on care management and high-cost claimants, 40%.
Aon Hewitt calculates that health care costs will trend up 8% to 10% in the next three to five years. Total health care costs per employee for large companies grew from $4,819 in 2001 to $10,743 in 2009. That cost will increase to $28,530, based on Aon Hewitt’s actuaries’ projection.
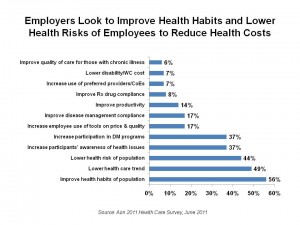
Since consumer-directed health plans and levying higher out-of-pocket costs to employees in and of themselves haven’t bent business’s health cost curve, employers are looking to wellness, disease management and behavior change to move the needle on health care costs. Still, employers will continue to accelerate the premium cost shift to employees and their families.
Health Populi’s Hot Points: Over one-half of employers say the most significant challenge facing their organization in accomplishing their health care goals is motivating participants to promote behavior change. The way they’ll go about motivating change will be a multi-pronged strategy including offering tools to raise participants’ awareness of health status and risk, and targeting communications based on employees’ individual health conditions and demographics.
Within 5 years, most employers say they’ll be using social media to reinforce smart health behaviors and actions for plan participants.
As Aon’s report succinctly puts it, it will require “less ‘education’ and more ‘motivation.'”
We’ve enough health-oriented information available online and in proliferating media channels. The new-new employer health benefit will couple targeted communications and personalized health management tools with incentives: penalties for non-participation (the “stick” approach) as well as rewards for achieving results (via “carrots”).
Employers will smartly not adopt tactical approaches in the value-based insurance design mode: for example, 72% of employers said they weren’t interested in medical tourism, and 68% of business won’t directly contract with health providers. Instead, employers will look to multi-pronged, integrated strategies that drive and sustain employees’ behavior change beyond co-pay tweaks and health risk appraisals.




 Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a