 The 2009 OECD Health Data set is out, and this year’s top line message doesn’t differ much from last year’s: the US spends a whole lot more money on health care, and gets a whole lot less in terms of life expectancy, infant morbidity, and epidemic obesity rates which inevitably lead to chronic conditions that are tough to manage.
The 2009 OECD Health Data set is out, and this year’s top line message doesn’t differ much from last year’s: the US spends a whole lot more money on health care, and gets a whole lot less in terms of life expectancy, infant morbidity, and epidemic obesity rates which inevitably lead to chronic conditions that are tough to manage.On average, OECD nations spend $2,964 per person and 8.9% of GDP.
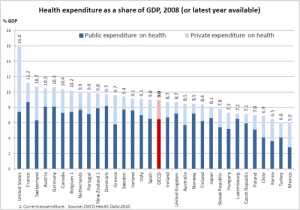
In 2007, OECD calculates that the US spent 16% of gross domestic product (GDP) on health. That equates to about $7,290 per American. The next highest dollar spending (normalized for purchasing power parity) was in Norway, which spent $4,763 per Norwegian, Switzerland spending $4,417 per Swiss, Luxembourg at $4,162 per Luxembourgeois, and $3,895 for each Canadian.
Thus, Canada spends just over one-half per citizen as the U.S. spends on each American.
The chart illustrates GDP expenditure allocated to health in countries that exceed the OECD average.
Remember that money is a process measure that doesn’t tell you how good health status is in each country. Let’s look to some of the quantifiable measures for insights into the ROI of health spending:– Life expectancy in the U.S. gained 8.2 years between 1960 and 2006; in the same period, Japan gained nearly 15 years, and Canada, 9.4 years.
– While infant mortality fell to 6.7 deaths per 1,000 live births in the U.S. in 2006, in the OECD infant mortality on average was 4.9. It is lowest in northern Europe, Luxembourg and Japan, with rates ranging 2 to 3 deaths per 1,000 live births.
– Obesity rates among OECD nations increased in recent years, with the highest rate in the U.S. at 34.3% — which means one in 3 Americans is by definition obese.
Health Populi’s Hot Points: The OECD database shows that the U.S. has the highest share of private health spending among OECD countries except for Mexico; both the U.S. and Mexico have 35% of total health spending from the private sector. In addition to the US and Mexico, only France and Canada have private insurance spending exceeding 10% of total health spending.
I’m not cheering “go Canadian!” to health policy makers, although I might be justified in many respects for advocating a Canadian-style health system based on these statistics. The fact is that the U.S. is unique in having a mixed private/public system, bolstered by employer-sponsored health insurance (unique, with a couple of rough analogues in Europe). Based on this week’s Health Populi blog highlighting Mercer’s survey on employers’ eroding support for comprehensive health reform, it is getting clearer that a health reform compromise in 2009 will have to build on the strengths of the current system: that will include private sector funding and caregiving.
For the U.S. to not be “#1 in the wrong way” when it comes to health funding and outcomes, integral components of a redesigned U.S. health system must include five key elements:
1. A well-funded, resilient, strong primary care base guaranteed and accessible to all Americans;
2. Ubiquitous electronic health record capability yielding data liquidity for measuring and rewarding outcomes;
3. “Connected health care” that empowers health citizens to take advantage of emerging tools that support them in managing chronic conditions, most notably diabetes and other high-cost conditions that erode quality of life and have long cost-tails;
4. A national obesity strategy that engages people: think “The Biggest Loser” combined with innovative local programs sponsored by grocery and drug chains, discount stores, and schools;
5. Continued incentives for innovations that promote early diagnosis and treatment in the care cycle, and breakthrough treatments.
We are wasting precious money and time on health spending that isn’t working for the benefit of all Americans.




 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a