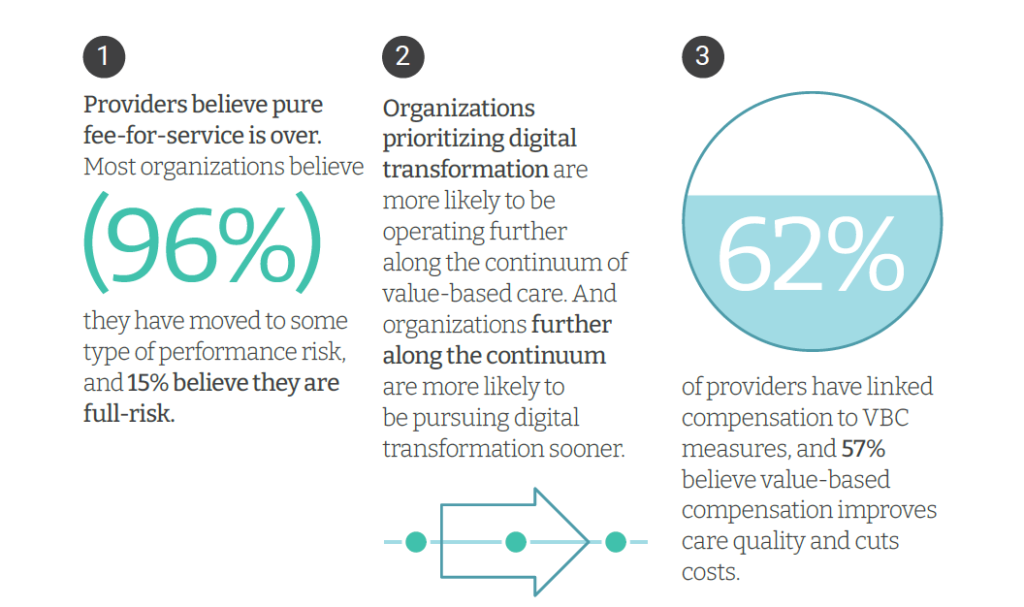
Only 4% of health care payments in the U.S. are pure fee-for-service (FFS) these days. “The end of pure FFS is near,” according to The State and Science of Value-Based Care, a report-out of survey research from Innovaccer and Morning Consult.
Innovaccer, a health cloud/data analytics company, worked with Morning Consult to do deep-dive interviews with 75 senior health care executives; research was conducted in November and December 2021, so these perspectives represent those of health system leaders at the start of 2022.
The full report is worth your read; my focus in this Health Populi post is to note the direct connection in health care leaders’ minds that value-based care is tightly related to digital transformation and, more granularly, data on peoples’ determinants of health (SDoH).

First, consider the pace of change from FFS to value-based care. This has been one of those instances in health care’s slow-to-change stasis where VBC has felt “so close, and yet so far.”
But the pace of change is quickening, according to the health care leaders polled: just three years from now in 2025, one-half of health care systems anticipate employing alternative payment models built on FFS architecture, shifting beyond links to quality and value.
Health care providers further along the continuum of value-based payment adoption have also more deeply implemented digital transformation infrastructures and investments. Quantifying that, within 3 years, 48% of providers anticipate taking on more value-based care and achieving digital transformation, compared to 39% who anticipate having more FFS in 3 years’ time “being digital.”
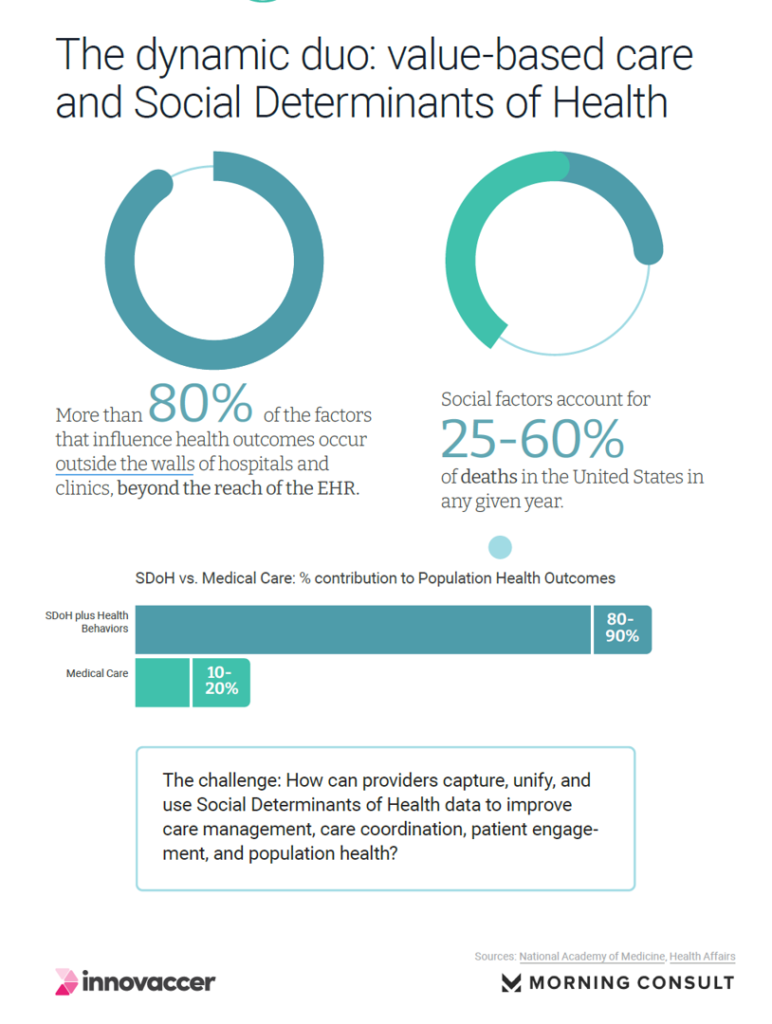
At the heart of “being digital” in the health system’s ability to effectively take on value-based care is the right data flowing through the chassis: and that points to the “dynamic duo” of VBC and the social determinants of health (SDoH) as Innovaccer terms the relationship.
Because health is essentially made outside of the doctor’s office and hospital walls — where we, as the mantra says, “live, work, play, pray” and I’ll add “learn and shop,” the information about our every day lives, social, economic, and environmental context are key to understand our risks and preventive opportunities for individual health or sickness.
Substance use/abuse, language barriers, and health literacy rank at the top of the list of SDoH factors that would be captured by one-half or more health systems this year — specifically, alcohol usage, tobacco usage, other controlled substance usage, English as a second language, and health literacy.
Racism-discrimination-violence, income, food security, safe house, education/literacy, and transportation were planned to be captured by about one-third of the health care executives.
While there is exuberant support for embedding SDoH factors into digitally transforming health care systems, relatively few providers will be leveraging software and other digital technology to identify at-risk patients. This is a transition phase wherein the vanguard systems are investing in digital transformation, but many not leveraging the SDoH data in population health programs yet by, say, integrating the determinants of health data in clinical workflows or using software to identify at-risk patients.
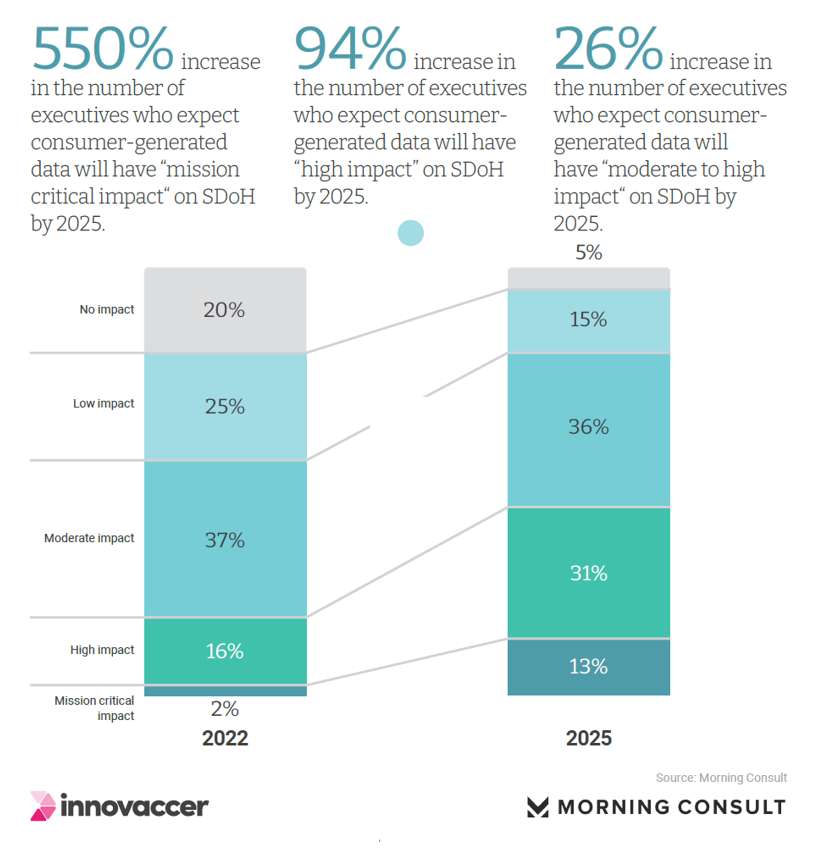
Health Populi’s Hot Points: Complementing and adding even more fire-power to assessing patients’ health risks, consumer-generated data from wearable tech and remote health devices and apps are expected to “explode” by 2025, according to the study. A fast-growing group of health system leaders expect these consumer-generated data flows will have “mission critical impacts” on determinants of health in three years.
In the post-pandemic error, more patients-as-consumers have been purchasing smartwatches and using apps for bolstering personal wellness and health-at-home.
The latest research from the Consumer Technology Association, convener of CES (the consumer electronics show), found that with the slowdown of the U.S. economy, the growing purchases of smartwatches has been one of the few bright lights in the retail consumer technology environment (beyond big-screen smart TVs and other more traditional consumer electronics buys).
The growing wellness and self-care via digital health tech is a consumer trend that the health care system can build on. But watch out for a digital health divide in terms of which at-risk patients would also be at-risk for not adopting, or be able to afford, the platform devices like smartphones and smartwatches to enable the data to be generated. We may be entering a new phase of digital therapeutic “prescriptions” of consumer-facing devices to enable at-risk patients to generate and gather necessary data to help people prevent and manage their health. Heath plans and providers taking on risk-based payments are tuning into this opportunity.




 Thank you, Jared Johnson, for including me on the list of the
Thank you, Jared Johnson, for including me on the list of the  I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a