 The record attendance at HIMSS12, in terms of both attendees (numbering some 38,000) and exhibitors, illustrated just how hot health information technology has become in the 20 years since I first began attending this meeting — when it was only a few thousand hospital computer geeks and materials managers picking up pocket protectors and calculators from vendors.
The record attendance at HIMSS12, in terms of both attendees (numbering some 38,000) and exhibitors, illustrated just how hot health information technology has become in the 20 years since I first began attending this meeting — when it was only a few thousand hospital computer geeks and materials managers picking up pocket protectors and calculators from vendors.
At this year’s conference, the major concerns were when Stage 2 meaningful use details would be revealed. HIMSS communications leadership in the press room thought it would be Tuesday, then Wednesday. Finally, it was Thursday the 23rd of February when Farzad Mostashari, National Coordinator for Health IT at the Department of Health and Human Services, said to a press conference of HIT reporters that the regs were, “At the Federal Register; they are having formatting issues….(the regs) are going to get promoted; I think people should just chill.”
Chill? The questions surrounding what would be included, downplayed, or enhanced for Stage 2 was a main topic of conversation all week at HIMSS. Of course, business was transacted without these details as the heavy lifting (or implementing, as it were) continues on adopting electronic health records and using them in ways that will ensure providers win their fair share of incentives flowing from the HITECH Act included in the stimulus bill (ARRA).
EHRs alone won’t bend the national health care cost curve or improve population health. To get to those grand goals will require connectivity and Big Data, and these were two major themes at HIMSS 2012. We used to talk about “interoperability” in the David Brailer days of the Office of the National Coordinator. In 2012, it’s about connectivity, based on the PR and market positioning of dozens of large HIT vendors who are trying to walk the talk of openness and iPod-like platforms for plugging in heterogeneous applications.
Connectivity then enables data bits and bytes to move through the health ecosystem, beyond a single institution through the cloud — and it was cloudy all over the HIMSS convention floor, both among large Big Iron vendors as well as the smaller up-starts who are providing some of the more novel and nimble applications that can help physician practices move from “here” to “there” in getting to meaningful use and connectivity.
Big Data and data analytics are also important news at HIMSS 2012 as we move from fee-for-services payment (outside of Kaiser, Group Health, Geisinger and VA) toward paying for performance, outcome and value. To do so requires real-time utilization management — the ability to identify people before they get too far downstream as high-cost high-risk patients.
But patient care isn’t a one-way street: patient engagement can help get people more involved, responsible and active in their own care — and that’s when outcomes improve and costs (year on year) fall in aggregate. In meaningful use Stage 1, patient engagement is prominently featured. Thus, patient portals were all over the HIMSS convention floor. They came in a broad range of look-and-feel, but most that I kicked tires on weren’t as well designed as I would have liked. We are in the nascent era of patient portals, with miles to go to get to something remotely engaging. Only the most activated patients would cotton onto the portals I viewed. I respect the hard work that’s gone into the dozen+ I dove into…and offered constructive comments to every vendor with whom I met. I am no patient portal maven — after all, we’re in the First Phase of such tools — but I’ve been schooled at the foot of Edward Tufte, Juhan Sonin, Michael Graves, and Ikea ; ) As Sonin told attendees of his talk on health IT and design, “software is a visual medium.” And so many portals’ pages looked like literal photocopies of medical forms — without videos, engaging graphics, or gamification. Still, this phase of patient engagement is about availability and access to data — this is a journey, not a destination, I tell myself. But innovative design clearly is prescribed for the patient portal, v2. In the “that’s what I’m talking about” vein, check out Tonic Health for its fresh approach to patient-centered design and engagement.
What’s promising on the patient engagement front are the many applications available to people at-home via remote monitoring and on-the-go via mobile applications. This year at HIMSS, the Qualcomm Life and 2net hub included many patient-facing tools from HelloHealth, Asthmapolis, AirStrip, and iSonea, among 40 such offerings. This section of the conference was a nice bridge from the Consumer Electronics Show to the B2B meeting that is HIMSS. I was very happy to see it as health engagement is critical to optimal patient outcomes. With accountable care payment regimes, these tools will be useful complements to inpatient and ambulatory care — keeping patients healthy on-the-go, and safe and well at home to stem readmissions to hospital.
Remote devices and patient engagement are addressed in Eric Topol’s important book, The Creative Destruction of Medicine, which I read enroute to/from Vegas. Every attendee at HIMSS should have been given a copy at check-in.
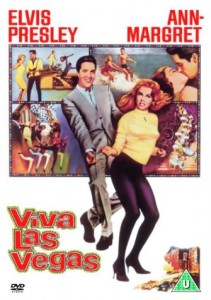 Health Populi’s Hot Points: I find the lyrics from Elvis’s iconic song, Viva Las Vegas, to reflect my post-HIMSS 2012 reflections:
Health Populi’s Hot Points: I find the lyrics from Elvis’s iconic song, Viva Las Vegas, to reflect my post-HIMSS 2012 reflections:
Demonstrating meaningful use to earn Stage 1/2 incentives:
Bright light city gonna set my soul
Gonna set my soul on fire
Got a whole lot of money that’s ready to burn,
So get those stakes up higher
The hard work ahead
How I wish that there were more
Than the twenty-four hours in the day
‘Cause even if there were forty more
I wouldn’t sleep a minute away
The risk and opportunity cost
Oh, there’s black jack and poker and the roulette wheel
A fortune won and lost on ev’ry deal
All you need’s a strong heart and a nerve of steel
How I wish that there were more
Than the twenty-four hours in the day
‘Cause even if there were forty more
I wouldn’t sleep a minute away
Oh, there’s black jack and poker and the roulette wheel
A fortune won and lost on ev’ry deal
All you need’s a strong heart and a nerve of steel
Viva Las Vegas, Viva Las Vegas.
Health care in the U.S. is at a crossroads. HIMSS being sited in Vegas provided a sobering lens about where health IT in the US could go: if momentum drives adoption, meaningful use, and data analytics that can inform care decisions in real-time getting patients the right care at the right time, then we say, in Todd Park style, “Viva health IT!”
If, on the other hand, the scenario turns out to be a growing chasm between the health care provider “have’s” and “have not’s” (especially community physicians), then the nation will have placed a bet, and lost. And that will not be so much about a few billion dollars; that will be the opportunity cost of moving America’s public health outcomes into a leading place on the league table of other OECD nations.
Next year, HIMSS will be hosted in New Orleans — two years in a row in cities that tout good times, not so much Healthy Cities milieus. While no one likes to laissez les bons temps roulez more than me, I wonder if that’s what we’ll feel like doing reflecting over the 2012-13 year of HIT implementation. Here’s hoping we’ll toast to progress…




 Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider