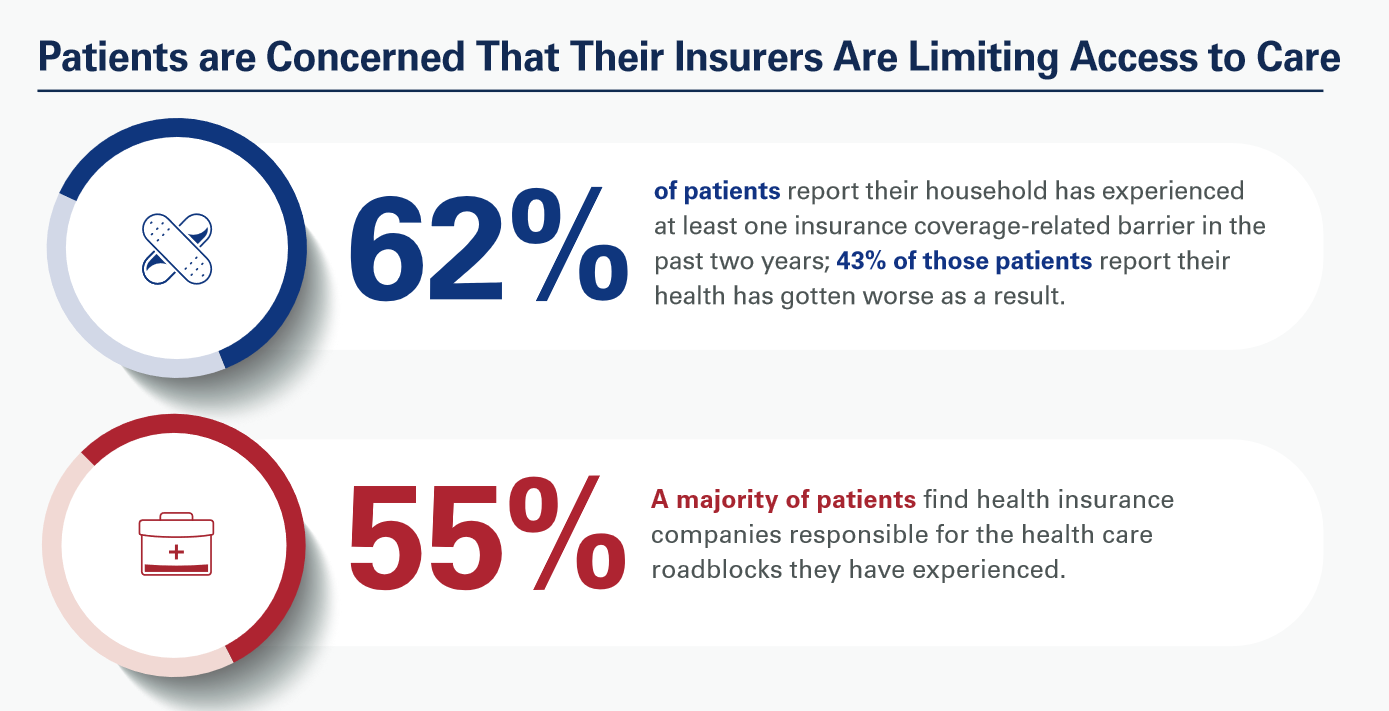
Most patients, nurses and doctors believe that health insurance plans reduce access to health care which contributes to clinician burnout and increases costs, based on three surveys conducted by Morning Consult for the American Hospital Association (AHA).
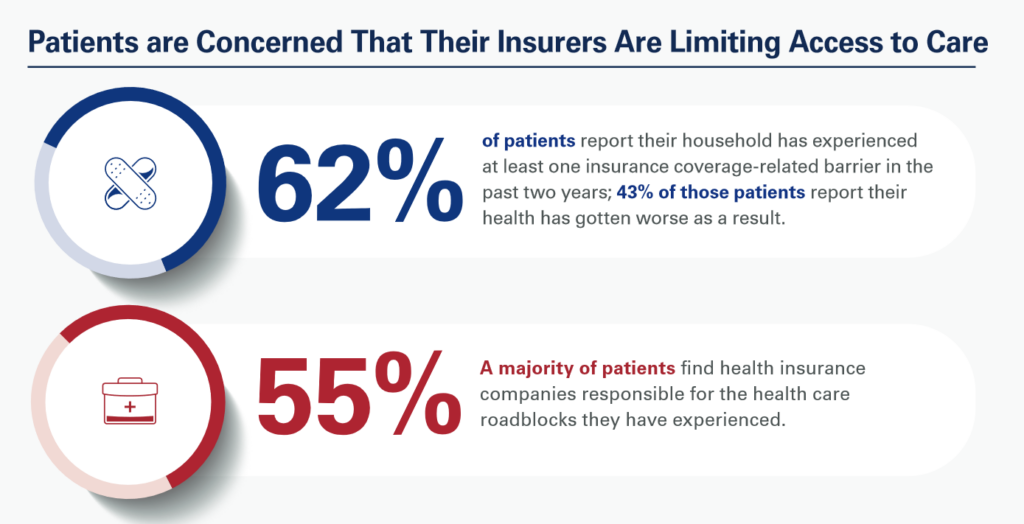
Most patients have experienced at least one health insurance related barrier in the past two years, and 4 in 10 of those people said their health got worse as a result of that care-barrier.
“These surveys bear out what we’ve heard for years — certain insurance companies’ policies and practices are reducing health care access and making it more difficult for our already overwhelmed clinicians to provide care,” according to Rick Pollack, AHA President and CEO.
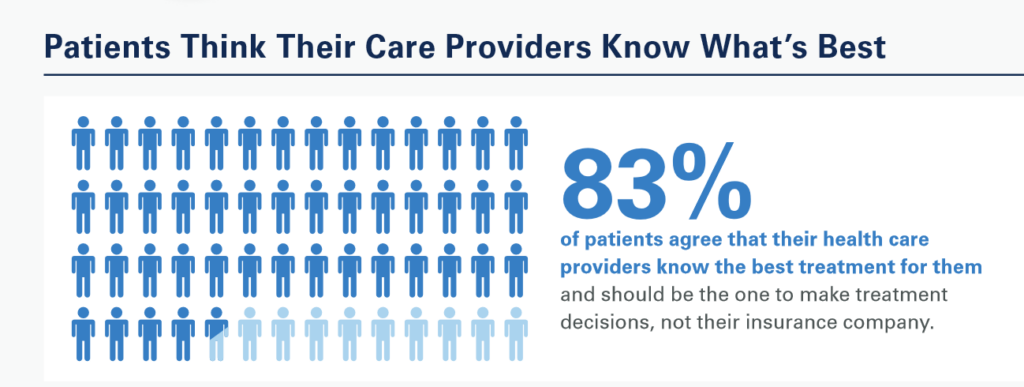
Most patients’ greatest trust-health equity sits with their providers (nurses and doctors) who should be the agent that makes treatment decisions — not the patient’s health insurer, consumers believe.
With consumers’ collective faith in nurses and doctors, the AHA turned to providers to gauge their perspectives on health care access and cost in 2023.
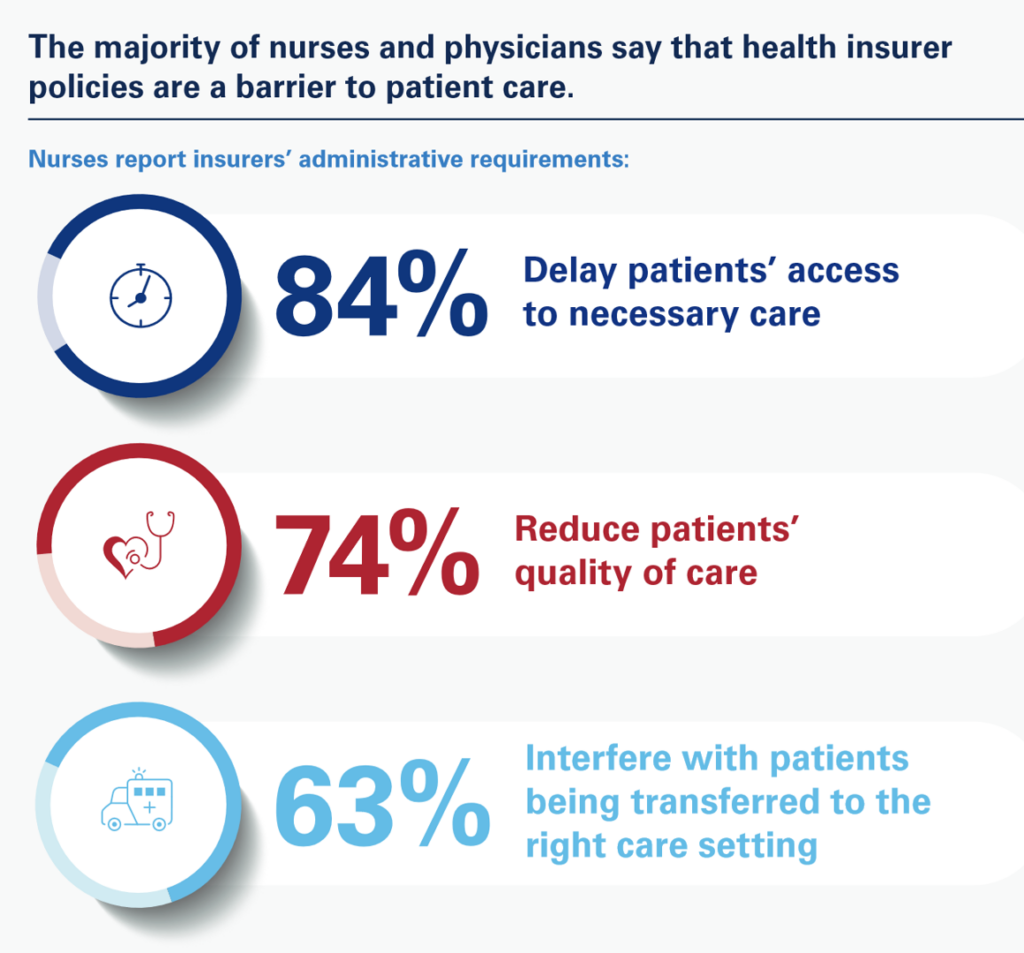
Most nurses believe that health insurers’ policies are barriers to patients receiving care in terms of delaying patients’ access to needed care, reducing patients’ quality of care, and interfering with patients being transferred to the right care settings.
4 in 5 physicians said that health insurers’ administrative requirement [negatively] impact doctors’ ability to practice medicine.
And those policy burdens are increasing, both nurses and doctors agree — “driving nurses away from the profession altogether,” AHA asserted, and compelling physicians to revisit their ability to operate a practice.
Note the methodologies deployed for the three polls:
- For the consumer survey, Morning Consult surveyed 1,502 U.S. adults online in December 2022
- For the study among nurses, Morning Consult polled 500 nurses online in March 2023
- For physicians, Morning Consult surveyed 500 physicians online between late March and early April 2023.
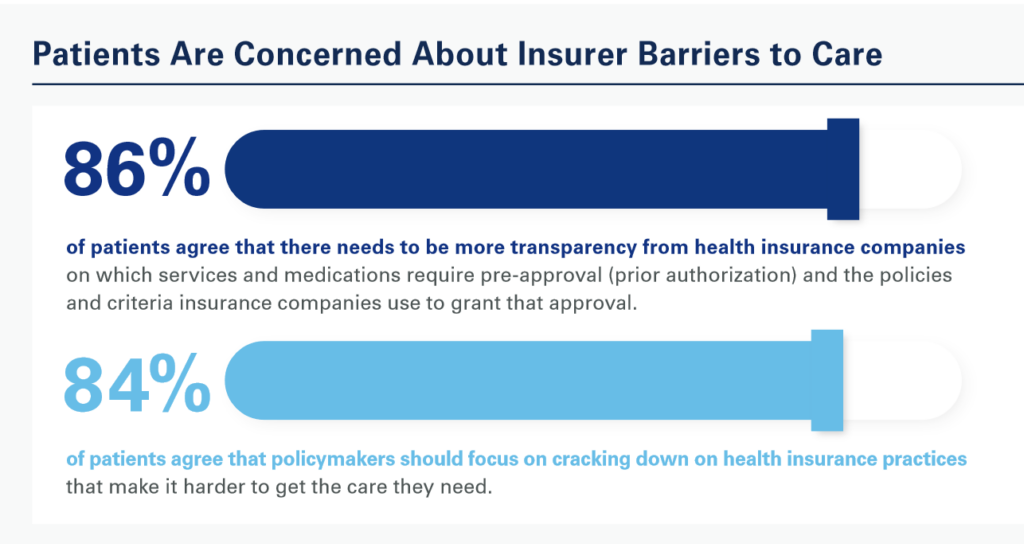
Health Populi’s Hot Points: “Health insurance should be a bridge to medical care, not a barrier to it for patients. If policymakers are serious about expanding access and addressing the health care workforce crisis, then we must hold insurance companies accountable for these harmful practices,” AHA CEO Pollack asserted in the studies’ combined press release.
We’re in a politically charged moment in America where the big health care advocacy organizations who lobby Capitol Hill and State Houses are in blame-game M.O.’s when it comes to health care costs — hospitals pointing to health insurers and pharma, pharma pointing to providers and insurers, and insurers pointing to….well, you get the picture.
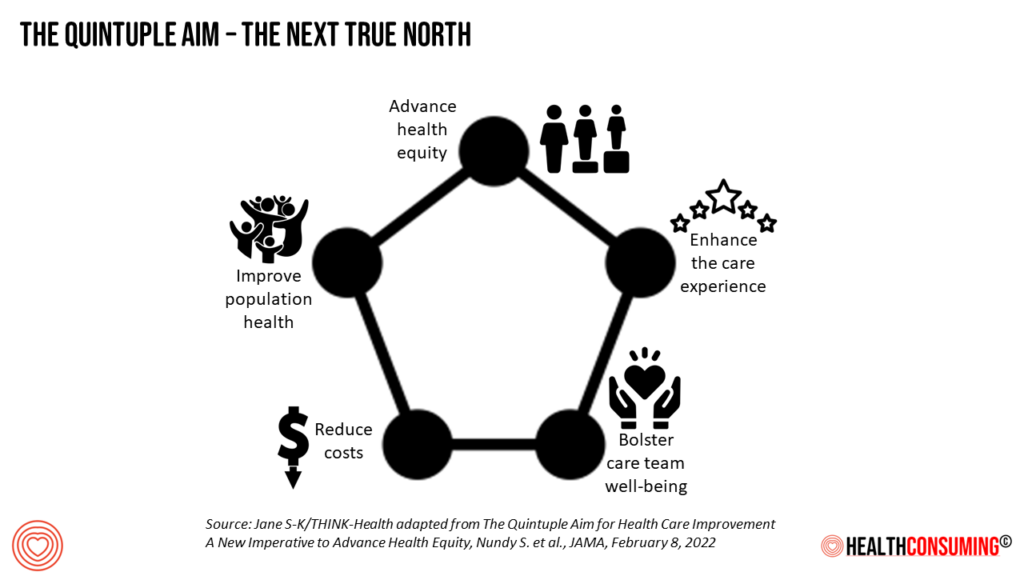
We must shift our True North mantra for improving health care in the U.S. to expand to the five pillars of the Quintuple Aim beyond improving the care experience, driving population health outcomes, and reducing per-patient costs. To those three initial Triple Aim objectives, we add in attending to health equity and drivers of health, and to bolstering the well-being of providers — nurses, doctors, pharmacists — the front-line human capital that delivers care to health citizens. Without the health of providers, the health system falls apart in further peril and fragmentation. exacerbating well-being for all/




 Thank you FeedSpot for
Thank you FeedSpot for