 Patients are morphing into health care consumers with growing use of technology for medical shopping and health engagement, according to a survey conducted by Altarum, the health services research organization.
Patients are morphing into health care consumers with growing use of technology for medical shopping and health engagement, according to a survey conducted by Altarum, the health services research organization.
Virtually all (99%) of U.S. health citizens want to play a role in medical decisions about their care. However, consumers vary in just how much of that responsibility they want to assume:
– 35% want to make the final decision with some input from doctors and other experts
– 29% want to be completely in charge of their decisions
– 28% want to make a joint decision with equal input from their doctor
– 7% want their doctor to make the decisions, providing some input themselves
Just 1% want the doctor to be completely in charge of treatment decisions.
These roles vary by age, with the oldest age cohort preferring joint decision making with doctors or making the final decision with physician input. The youngest age cohort, 25-34, is more keen to be “completely” in charge of medical decisions (33%) or in final decision making mode with physician input. This “flavor” of decision making — the final decision with some input from doctors and other experts — is the most commonly favored decision making style, ranging from 37% among 25-34 year olds to 32% for 65+.
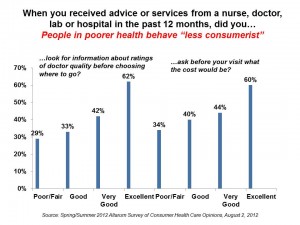
The cost of care is an issue consumers are keen to know more of in health care. Altarum asked consumers about two health behaviors when receiving advice or services from a health provider — looking for information about doctor quality ratings before choosing where to go, and asking before a visit how much the cost would be. Overall, fewer than half of consumers asked about prices (42%) or investigated quality before receiving the health service (39%).
Importantly, engaging in these two health behaviors was less likely among folks who were in poor/fair health than those in excellent health, with 29% looking for quality information on providers and 34% asking about cost — compared with 62% of people in excellent health asking about quality and 60% asking about cost.
The survey found, consistent with other polls, that most consumers trust and like their doctor. Furthermore, 76% of consumers also believe that their doctor would “never” recommend a test or procedure unless it was necessary.
The poll was conducted online in April and May, 2012, among 2,129 U.S. adults.
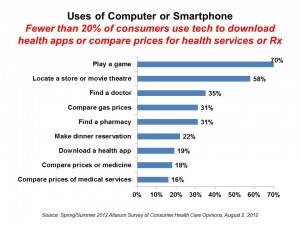 Health Populi’s Hot Points: Communications technology plays a prominent role in enabling consumerism in health care. Altarum looked into peoples’ use of computers and smartphones for everyday life tasks, such as playing games, locating stores and theatres, comparing gas prices, and conducting health care activities.
Health Populi’s Hot Points: Communications technology plays a prominent role in enabling consumerism in health care. Altarum looked into peoples’ use of computers and smartphones for everyday life tasks, such as playing games, locating stores and theatres, comparing gas prices, and conducting health care activities.
The second chart arrays the findings: 35% of computer and smartphone users have used these tech’s for finding a doctor, 19% have downloaded a health app, 18% have compared prices of medicines, and 16% have compared prices for medical services. It is early days for comparative shopping in health, but this aspect of health-shopping is poised to substantially grow toward 2014 as health insurance exchanges and consumer-driven health plans put health citizens into the role of health shoppers.
What’s concerning in Altarum’s findings is that the poorer health the consumer perceives, the less consumer-empowered that individual feels. While 75% of those in excellent health say they’re confident they can reduce costs of care by shopping for better prices, only 30% of those in poor/fair health are confident in doing so. Thus, 70% of those in poor/fair health are uncertain/not at all confident that they’ll be competent health shoppers, able to reduce their health costs.
Yet it’s those in poorer health who tend to be higher cost patients.
While several entrepreneurial companies are positioning themselves to play starring roles in shedding light on prices and quality in health care — such as Castlight Health, Change:Healthcare, Clear Health Costs, among them — it is unclear whether their business plans are positioning them to serve the sicker, less health literate population. This is a key issue for policymakers and health foundations to target. It’s an area where health disparities could widen.




 Thank you, Jared Johnson, for including me on the list of the
Thank you, Jared Johnson, for including me on the list of the  I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a