Today marks eight days before #Election2024 in the U.S. While many political pundits assert that “health care is not on the ballot,” I contend it is on voters’ minds in many ways — related to the economy (the top issue in America), social equity, and even immigration (in terms of the health care workforce).
In today’s Health Populi blog, I’m digging into Access Denied: patients speak out on insurance barriers and the need for policy change, a study conducted by Ipsos on behalf of PhRMA, the Pharmaceutical Research and Manufacturers of America — the pharma industry’s advocacy organization (i.e., lobby group) that has polled U.S. adults’ views on health care access and costs. As we look into these survey findings, we remind ourselves that this study was done in the context of PhRMA’s point-of-view and mission objectives. This report was published just before the 2024 U.S. election and reflects Americans’ views on health care policy just before they exercise their voices at the polls on 5th November 2024 (noting some voters have already voted by mail and in early voting booths in states where available). The survey was conducted online between mid-July and August 1st among 2,592 adults ages 18 and over — most of whom had health insurance at the time of the study. 
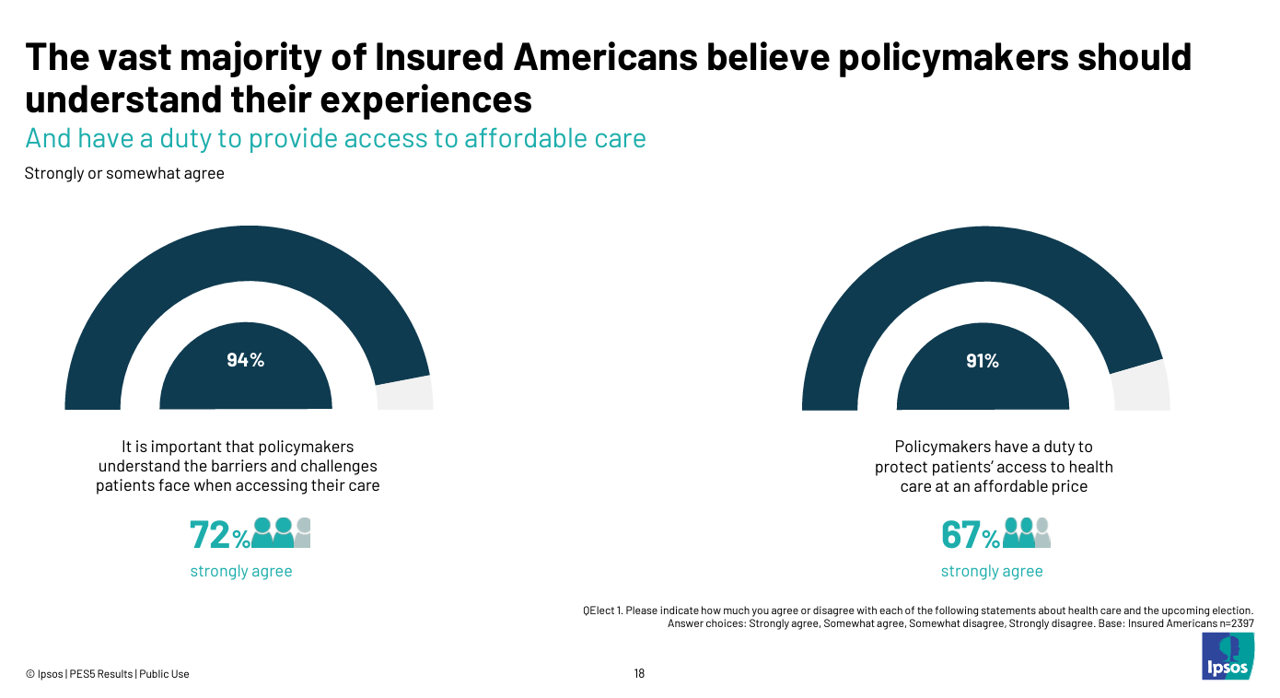
The top-line, politically speaking, is that the vast majority of insured Americans believe that policymakers — that is, the government — have a duty to provide access to health care at an affordable cost.
Patients’ access and affordability story is based on several experiences quantified in the survey data:

- 4 in 10 consumers have encountered at least one health insurance challenge, led by issues with priority authorization and formulary exclusions
- 1 in 2 insured Americans reported trouble anticipating the cost of their prescribed drugs and understanding their insurance coverage for medicines–with 43% of folks concerned their insurance company would deny future care
- Nearly one-half of insured Americans said their out-of-pocket costs were too expensive or unaffordable.

Health care cost concerns are bound up in peoples’ perceptions that in the next 12 months, they would not be able to afford out-of-pocket costs and health insurance premiums.
84% of people believe that health care costs for patients would be lower if insurers and PBMs spent less time managing how medicines should be prescribed by doctors. The top three solutions consumers identified to address out-of-pocket cost concerns were,
- Limiting out-of-pocket costs
- Requiring insurance plans to cover more products and services without a deductible, and,
- Serving up greater transparency of costs.

Health Populi’s Hot Points: On this third issue, the study detailed consumers’ views of how health plans and PBMs, as well as hospitals and health systems, provided greater transparency on costs, rebates and discounts, and access programs and copay assistance.
The last table shown here from the PhRMA/Ipsos report tells us patients’ support for different flavors of transparency and accountability for health insurers and PBMs as well as from hospitals. We see strong support by consumers for both health industry stakeholder groups to serve up transparency for a variety of challenges:
For health insurers and PBMs, most U.S. adults support them…
- Requiring health plans and PBMs to pass on any rebates or discounts received from pharma companies on prescription drugs at he pharmacy
- Cracking down on abuse practices by PBMs and plans such as inappropriate fail first/step therapy and prior auth
- Ensuring copay assistance that is provided by pharma manufacturers goes to patients as intended and not to health plans and PBMs
- Requiring Medicare Part D plans to pass on rebates or discounts they receive from pharma companies to seniors at the pharmacy counter, and,
- Ensuring copay assistance provided by the pharma companies counts toward plan deductibles and OOP maximums; and,
For hospitals, most U.S. adult support them….
- Being more transparent about how much they mark up the costs for prescription medicines
- Using the discounts received on prescription meds to help low-income and uninsured patients access the medicines they need, and,
- Driving greater oversight and transparency of safety net programs (such as 340B) to ensure hospital and other entities are using drug discounts they receive to serve the needy patients the programs are meant to serve.

Both the Democrat and Republican Presidential candidates have developed drug cost policies in their campaigns. I exhibit EY’s comparison of Harris’s versus Trump’s possible policies here for your tracking political pharma-cost Bingo. Some key differences might be,
- Each President’s approach to extending IRA drug price negotiation provisions, expanding the list of medicines under negotiation
- How each would deal with Medicare Part D drug pricing — keeping in mind seniors’/retirees’ keen interest in voting to preserve maximum Medicare and Social Security benefits
- How PBMs would be regulated or otherwise reformed via legislation, and,
- Overall policy positions coming out of The Centers for Medicare and Medicaid Services.

We should also keep in mind what consumers told PhRMA and Ipsos were health citizens’ priorities for policy making: the top four “tied” positions were reducing inefficiency and bureaucracy (which could account for up to 30% of U.S. health care spending), improving access to preventive care, improving access to mental health care, and reining in costs.
As “the economy” continues to rank as the top issue on U.S. voters’ minds, remember that health care costs are bound up in that — including the motivating issue of women’s health care which will drive millions of people to the polls.




 Thank you, Jared Johnson, for including me on the list of the
Thank you, Jared Johnson, for including me on the list of the  I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a