“The Church As Field Hospital” – Learning from Pope Francis About the Power of Loneliness and Connection

“I see the church as a field hospital after battle.” The death of Pope Francis gives me reason today to turn to one of the key themes he spoke about during his years leading the Catholic Church. That is, the Church as Field Hospital. Healthwise, the Pope had a history of respiratory conditions which began in his early 20s when he had surgery to remove a piece of his lung affected by an infection. Still, he lived to a ripe 88 years of age, participating in Easter Sunday’s morning mass at The
From Bowling Alone to Eating Alone – What the Shift to Take-Out Food Means for Our Social Well-Being and Mental Health
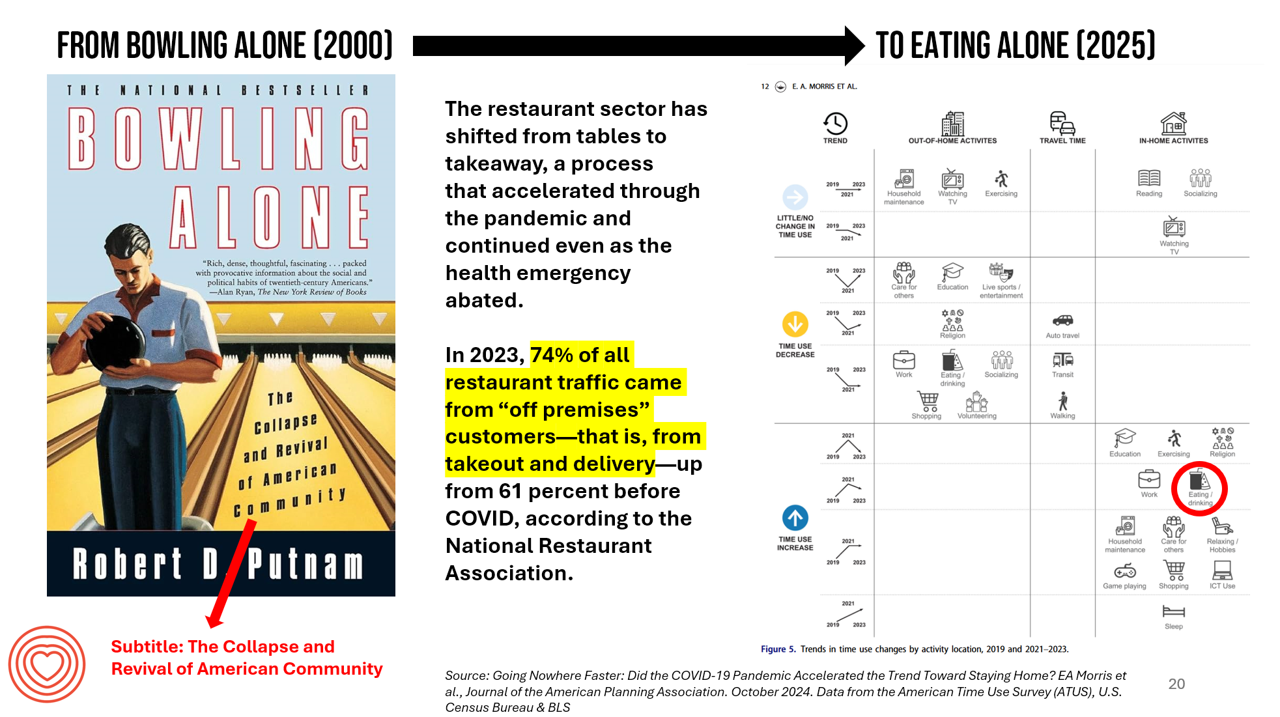
New data from the American Time Use Survey, research conducted by the U.S. Census Bureau and the Bureau of Labor Statistics, shows that Americans now favor eating in-home compared with eating out at restaurants. Corroborating this shift is other data from the National Restaurant Association sharing that 74% of all restaurant traffic in 2023 came from “off premises” customers — that is, from takeout and delivery — up from 61% in the pre-COVID era. What does this mean for our health, well-being, and sense of community and connectivity? I’m preparing a new talk to
Health Consumer Check-In: From Digital Detox to Analog Wellness, Social Re-Wilding, and a Return to the Bookstore

As humans have undergone personal digital transformations, living omni-channel and appreciating the conveniences that being switched-on can bring, there’s a growing demand for “analog wellness.” That’s one of ten trends covered in the Global Wellness Institute’s (GWI) report on 2025 Wellness Trends, and one I want to dig into early this year as consumers are facing growing challenges to our privacy, social bullying, and workforce stressors compelling many employees to spend too many hours in digital isolation and loneliness. To paint the larger landscape of and drivers underpinning analog wellness, I will weave several important reports and studies together, all
Measuring Progress for Life Sciences: Trust, Patient Access, and Prevention at a Fork in the Road of Public Health
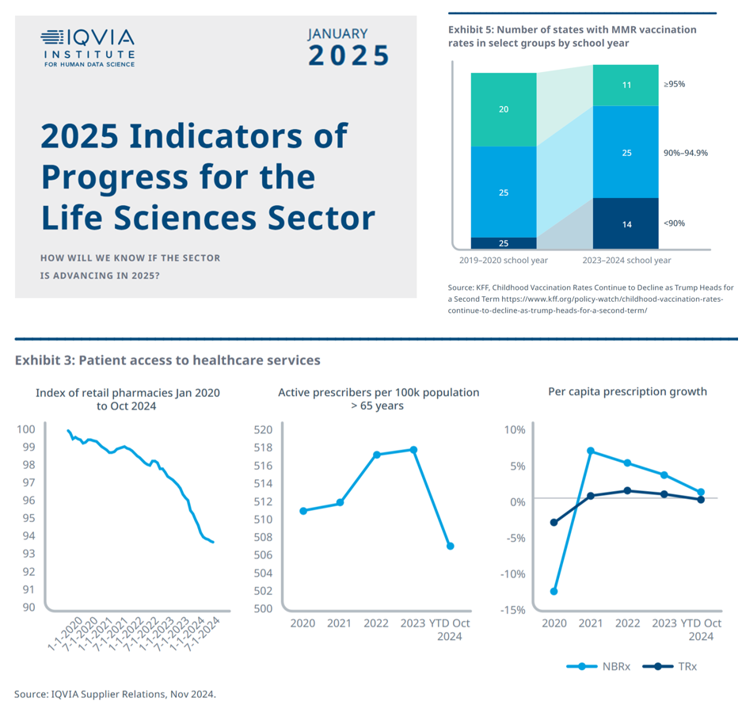
How will we know if the life sciences sector is advancing in 2025? This is the question asked at the start of the report, a Research Brief: 2025 Indicators of Progress for the Life Sciences Sector, from the IQVIA Institute for Human Data Science (IQVIA). To answer that question, IQVIA identified ten indicators for this 2025 profile on the life sciences sector. I selected four key data points for this discussion which provide particularly informative insights for my advisory work right now at the intersection of health, people/consumers, and technology: Trust for/with/in life science
Trust and Grievance in 2025: The Edelman Trust Barometer on MLK Jr. Day Converging with the World Economic Forum Kick-Off and the Inauguration of the 47th U.S. President
At the start of each new year comes the World Economic Forum meet-up in Davos, Switzerland and with that conference start today, 20 January 2025, the publication of the Edelman Trust Barometer. Now in the study’s 25th annual edition, the Edelman Trust Barometer this year finds us, globally, in a Crisis of Grievance which is eroding trust. Edelman surveyed 1,150 residents (plus or minus) in each of 28 countries around the world, yielding over 33,000 citizens’ voices sharing perspectives on trust and institutions. Interviews were fielded from late October to mid-November 2024.
The Evidence for Gratitude and Health, 2024 Giving Thanks
In our home, we’re feeling very grateful for our healthy lives and work-flows right now, being very mindful about seeing blessings around me and within me…. So I’m sharing the love (or “scaling the love” as I recently coined at OSF’s Digital Health Symposium!) to honor American Thanksgiving 2024 here in Health Populi pointing out several sources highlighting the evidence on gratitude and health….underpinned with love, the ultimate driver of health and well-being. Leslie Sarasin, President and CEO of FMI, the Food Industry Association, reminds us that, “Our immigrant ancestors, the pilgrim settlers, worked hard
How’s Life? Around the World – In the U.S., It’s the Sadness That Stands Out
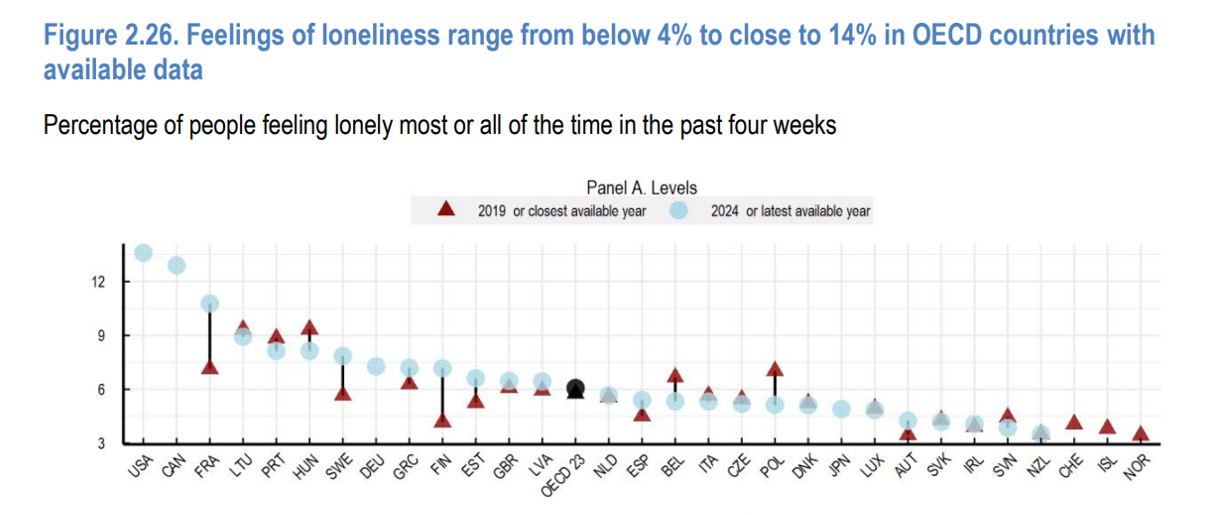
A new report from the OECD asks the question, “How’s Life?” with the tagline letting us know the plotline focuses on “well-being and resilience in times of crisis.” The Organization of Economic Cooperation and Development (OECD) has tracked the well-being of member nations for the past six years, taking a broad view on the definition of holistic health — including physical, mental, financial, and social aspects of people living in OECD countries. The first “How’s Life?” report was published at the height of the global financial crisis; the authors of this report introduce it saying that, “the
Women and #Election2024: Listening to Abigail Adams
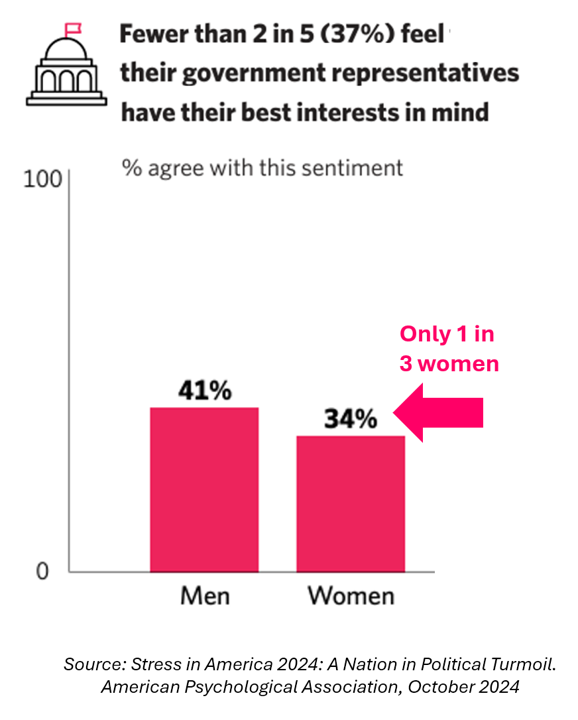
With a handful of days before #Election2024 delivers final voters to polls in the U.S. on November 5th, Americans’ political stress is hitting fever pitches from all points on the U.S. political spectrum. Here is the sticker I am using in my journal today, November 1 2024, from Mental Health America. “Vote as if your mental health depends on it.” MHA has a portal devoted to 2024 Election Mental Health Resources, including a section with “mental health voter merch” to call out the phenomenon of political stress and support the efforts
Where Democrats and Republicans Agree on Health Care Policies – From Medicare and Prescription Drugs to Gun Safety
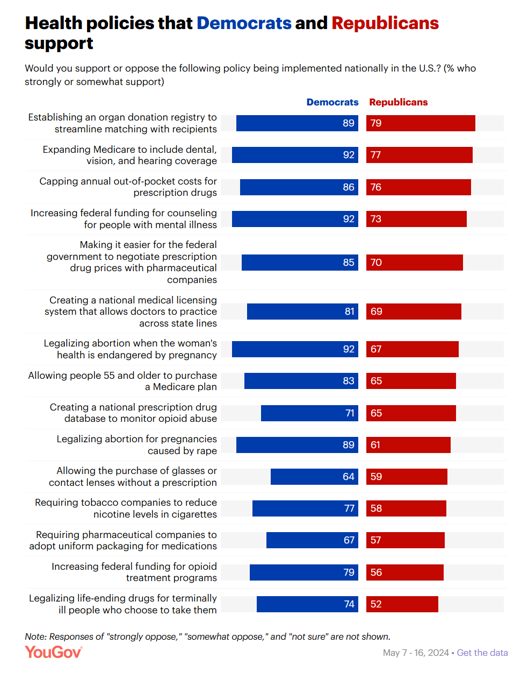
In a super-divided electorate like the U.S. with about 60 days leading up to the 2024 Elections, we might assume there are no “purple” areas of agreement between the Red (Republicans) and the Blue (Democrats) thinking in PANTONE color politics. Surprisingly, there are many health policies on which Democrats and Republicans concur, as found in a series of YouGov polls conducted in May 2024. YouGov fielded the health policies poll in five waves online, each among roughly 1,100 U.S. adults in May 2004. This bar chart summarizes health
Medical Debt, Aflac on Eroding Health Benefits, the CBO’s Uninsured Forecast & Who Pays for Rising Health Care Prices: A Health Consumer Financial Update
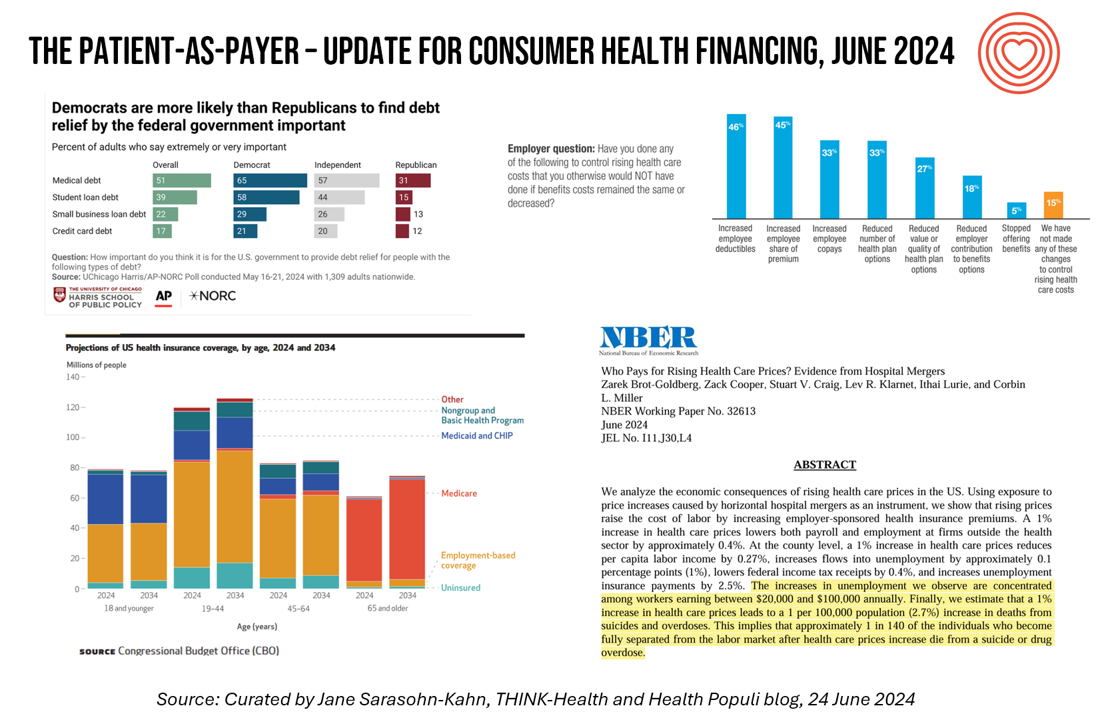
On June 11, Rohit Chopra, the Director of the Consumer Financial Protection Bureau (CFPB) announced the agency’s vision to ban Americans’ medical debt from credit reports. He called out that, “In recent years, however, medical bills became the most common collection item on credit reports. Research from the Consumer Financial Protection Bureau in 2022 showed that medical collections tradelines appeared on 43 million credit reports, and that 58 percent of bills that were in collections and on people’s credit records were medical bills.” Chopra further explained that medical debt on a consumer credit report was quite different than other kinds
A Vote for Telehealth is a Vote for American Patients’ and Doctors’ Well-Being
Whether you’re a patient or a physician in the U.S., you’re burned out, tapped out, stressed out, timed out. While the 118th U.S. Congress can’t agree on much before the 2024 summer recess, there’s one bipartisan stroke of political pens in Washington, DC, that could provide some satisfaction for both patients and doctors: bring telehealth back to patients and providers permanently. Those pens would do two things to modernize American health care for both patients and doctors: first, Congress would pass the CONNECT for Health Act (HR 4189. S 2016) and second, re-introduce and sign the Telehealth Modernization Act.
Everybody is Stressed in America, and It’s Not Good for Our Health: the 2023 Update from the American Psychological Association

The U.S. is “a nation recovering from collective trauma,” the according to the latest survey on Stress in America 2023 from the American Psychological Association (APA). The APA has been quantifying Stress in America since 2007; for context, at the end of that year The Great Recession kicked in, and in response President Obama’s team put together assistance to bolster the national economy, jobs, and health technology (codified in the American Recovery and Reinvestment Act). American health citizens are experiencing a deja vu in 2023 akin to their financial stress experienced in the APA 2008 Stress
A Public Health Wake-Up Call: Reading Between the Lines in IQVIA’s 2023 Use of Medicines Report
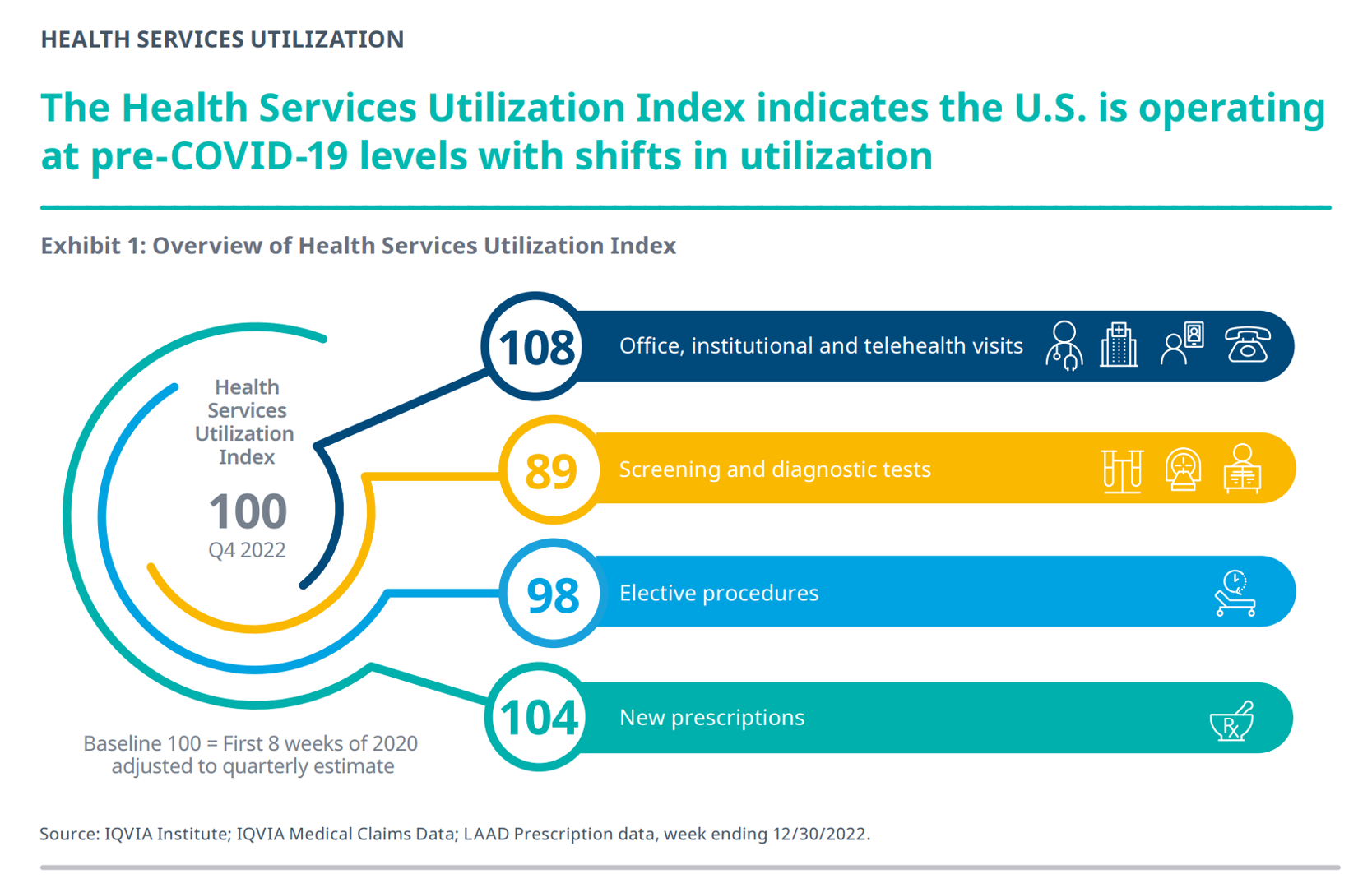
Reviewing the annual 2023 report from the IQVIA Institute for Human Data Science discussing The Use of Medicines in the U.S. is always a detailed, deep, and insightful dive into the state of prescription drugs. It’s a volume speaking volumes on the current picture of prescribed meds, spending and revenues, health care utilization trends, and a forecast looking out to 2027. In my read of this year’s review, I see a flashing light for U.S. health care: “Wake up, public health!” I’ve pulled out a few of the data points that speak to me about population health, prevention and early
The New Loneliness Health Agenda from Dr. Vivek Murphy, US Surgeon General
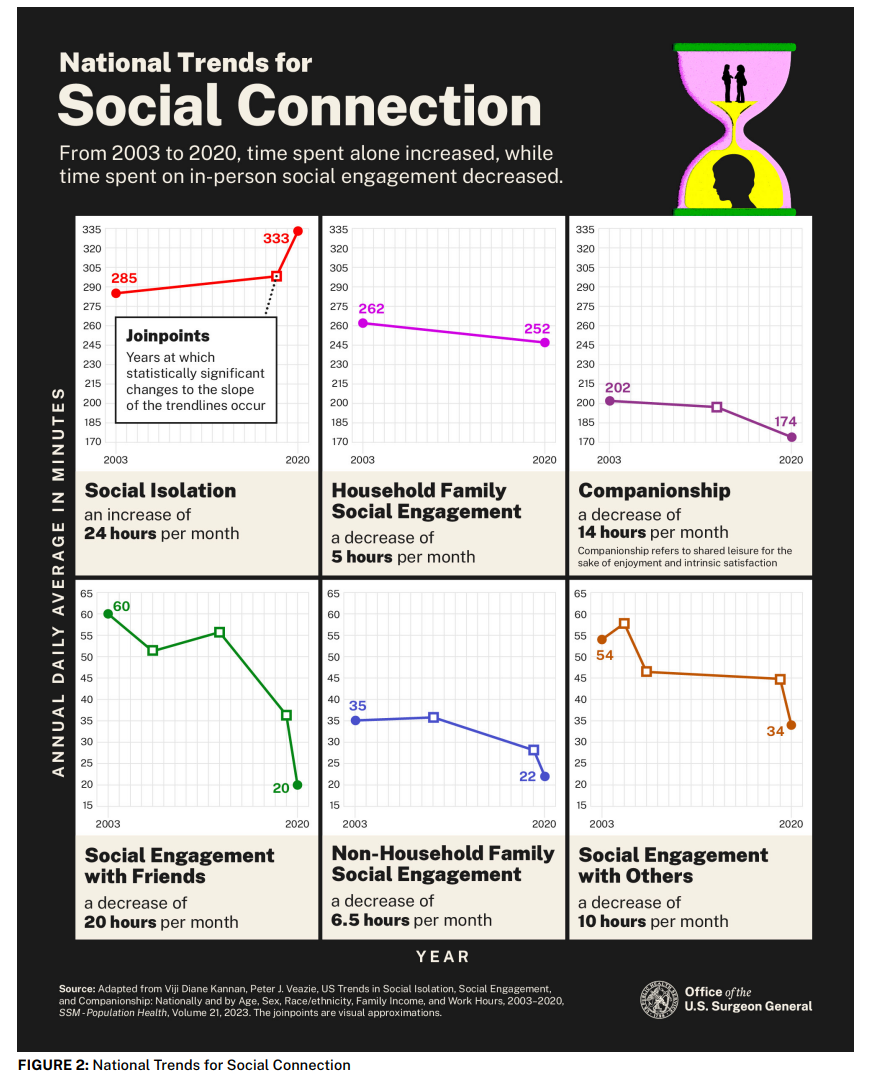
This week, U.S. Surgeon General Dr. Vivek Murthy unveiled a plan to address loneliness in America. This isn’t a theoretical thing: Dr. Murthy has come out of the loneliness closet to tell us that he, too, has confronted and dealt with to loneliness, putting himself out there/here as Exhibit A in the epidemic of Americans who are lonely — and suffering risks across every dimension of personal and social health. The New York Times published Dr. Murthy’s op-ed on the issue in the Sunday issue in a call-to-action titled, “We have become a lonely nation. It’s time to fix that.”
The New Deaths of Despair in America – Among U.S. Children
The phenomenon of Deaths of Despair is the short-hand name for rising mortality among certainly people living in the U.S. due to overdose, accidents, and suicide. Angus Deaton and Anne Case published their first of many research papers on Deaths of Despair in 2015. Their research uncovered the risks of dying a Death of Despair to be higher among men, especially those between the ages of 25 and 64. But mortality isn’t only going in the wrong direction for those people most closely associated with the Deaths of Despair demographic: there’s another life-span line graph moving in the wrong direction,
The Top 10 Patient Safety Concerns for 2023 Are About Social, Mental and Behavioral Health
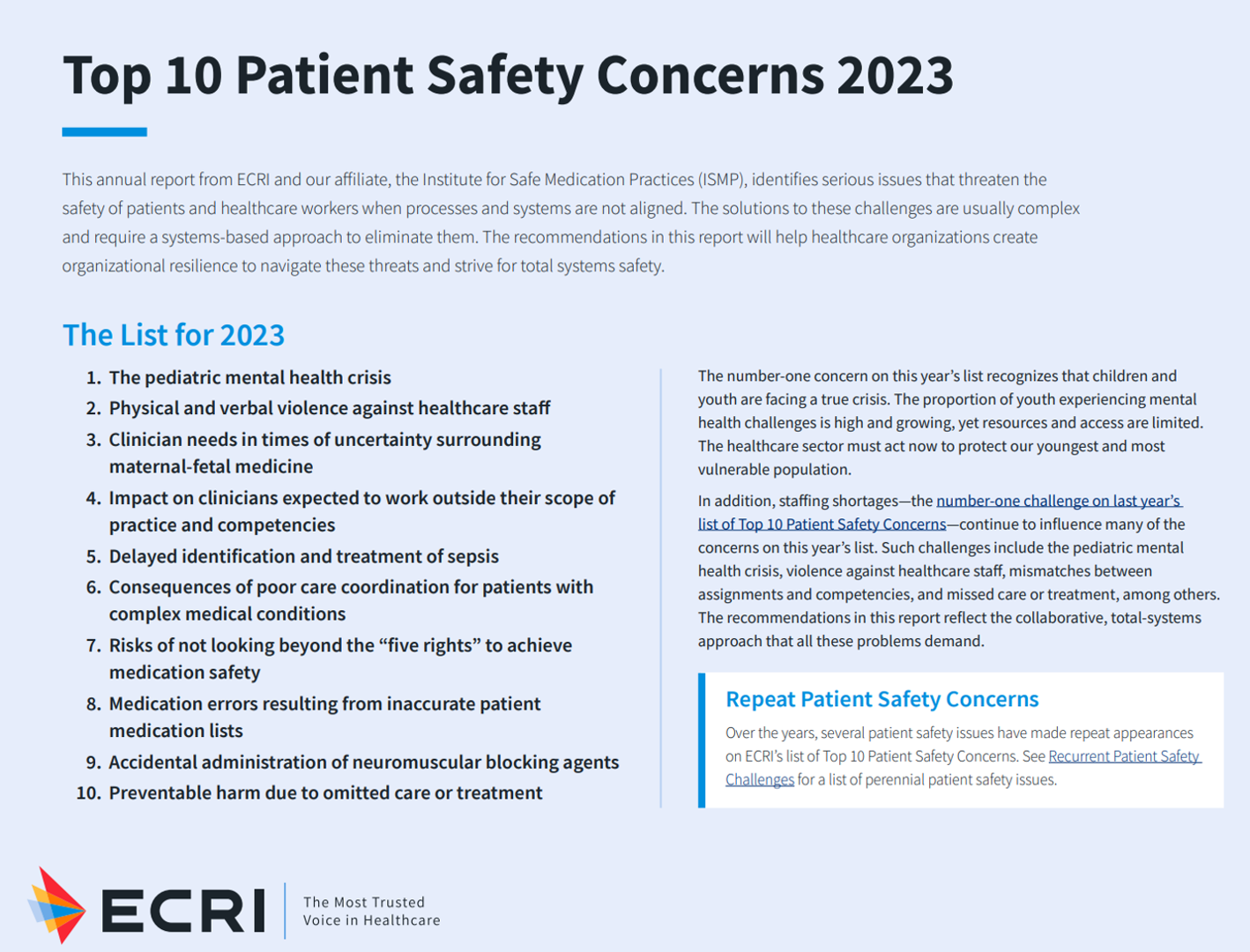
Ten years ago, ECRI named the top 10 health technology hazards for 2013: they were alarm hazards, medication administrative errors using infusion pumps, unnecessary exposure and radiation burns from diagnostic radiology procedures, patient/data mismatches in EHRs and other HIT systems, interoperability failures with medical devices and health IT systems, and five other tech-related hazards. In 2014, ECRI pivoted the title of this annual report to “patient safety concerns,” a nuance away from health technology. Fast forward to 2023 and ECRI’s latest take on the Top 10 Patient Safety Concerns 2023. While technology is embedded in this list, the headlines have more
The Future of Love and How It Could Shape Health, Well-Being, and Daily Living

“The future of love is bound to the institutions that have historically shaped and defined it,” Ipsos’s What the Future: Love report begins. Consider: religion, government, financial institutions….and the health care ecosystem, as well. On this Valentine’s Day 14th February 2023, it is a good time to consider this convergence as health politics, financial well-being, and emerging technologies will be re-shaping institutions and consumers in the coming months and near-term. The Ipsos researchers have been assessing the future of many aspects of our lives over the past couple of years, such as the future of wellness,
The US Healthcare System Outspends and Underperforms While Most People Live Paycheck to Paycheck
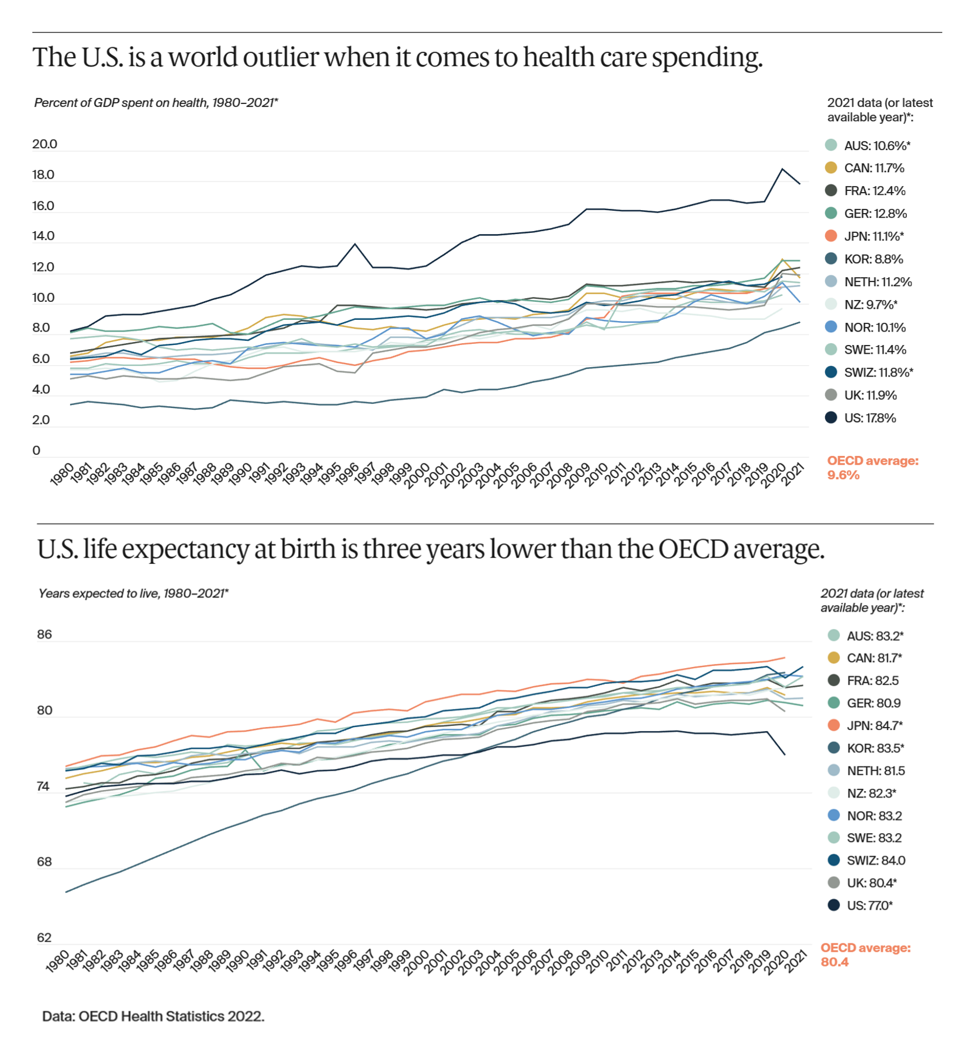
The U.S. is an outlier in the world for high health care spending, as well as in low achievement for life expectancy at birth — 3 years less than that in peer OECD countries — discussed in U.S. Health Care from a Global Perspective, 2022: Accelerating Spending, Worsening Outcomes, the latest look into American health system performance in a global context from The Commonwealth Fund. Another study published in JAMA this week talks about the Organization and Performance of US Health Systems, calling out the fact that, “Small quality differentials combined with large price differentials suggests that health systems have
What Are Patients Looking for in a Doctor? It Depends on Who You Ask…and Their Race
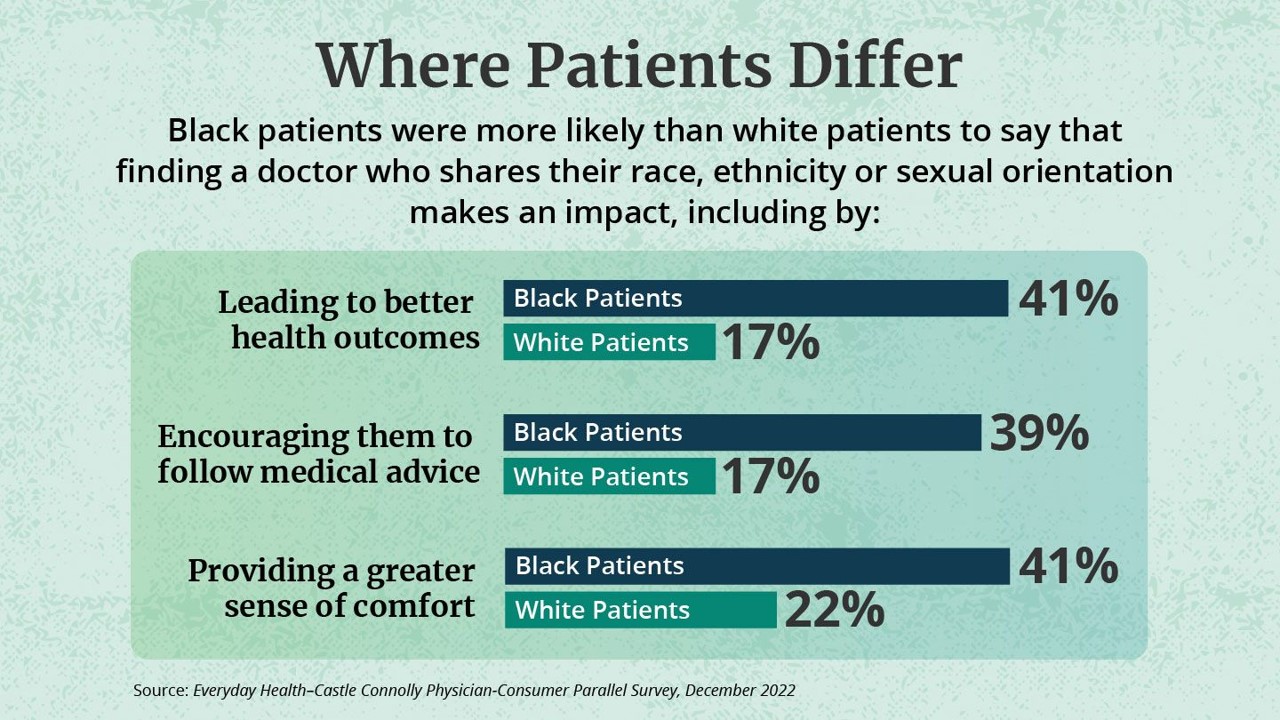
While the same proportion of Black and White patients say they are looking for a doctor with empathy and compassion, there are relatively large differences between patients based on their race, found in the Everyday Health-Castle Connolly Physician-Consumer study. The survey was conducted in December 2022 among a group of 1,001 U.S. consumers and 277 Castle Connolly health care professionals. As the first bar chart illustrates “where patients differ, “Black people were nearly twice as likely as white people (41 percent versus 22 percent) to completely agree that they would be more comfortable and
The Polarization of Trust in 2023 – What It Means for Health, via Edelman at Davos WEF 23
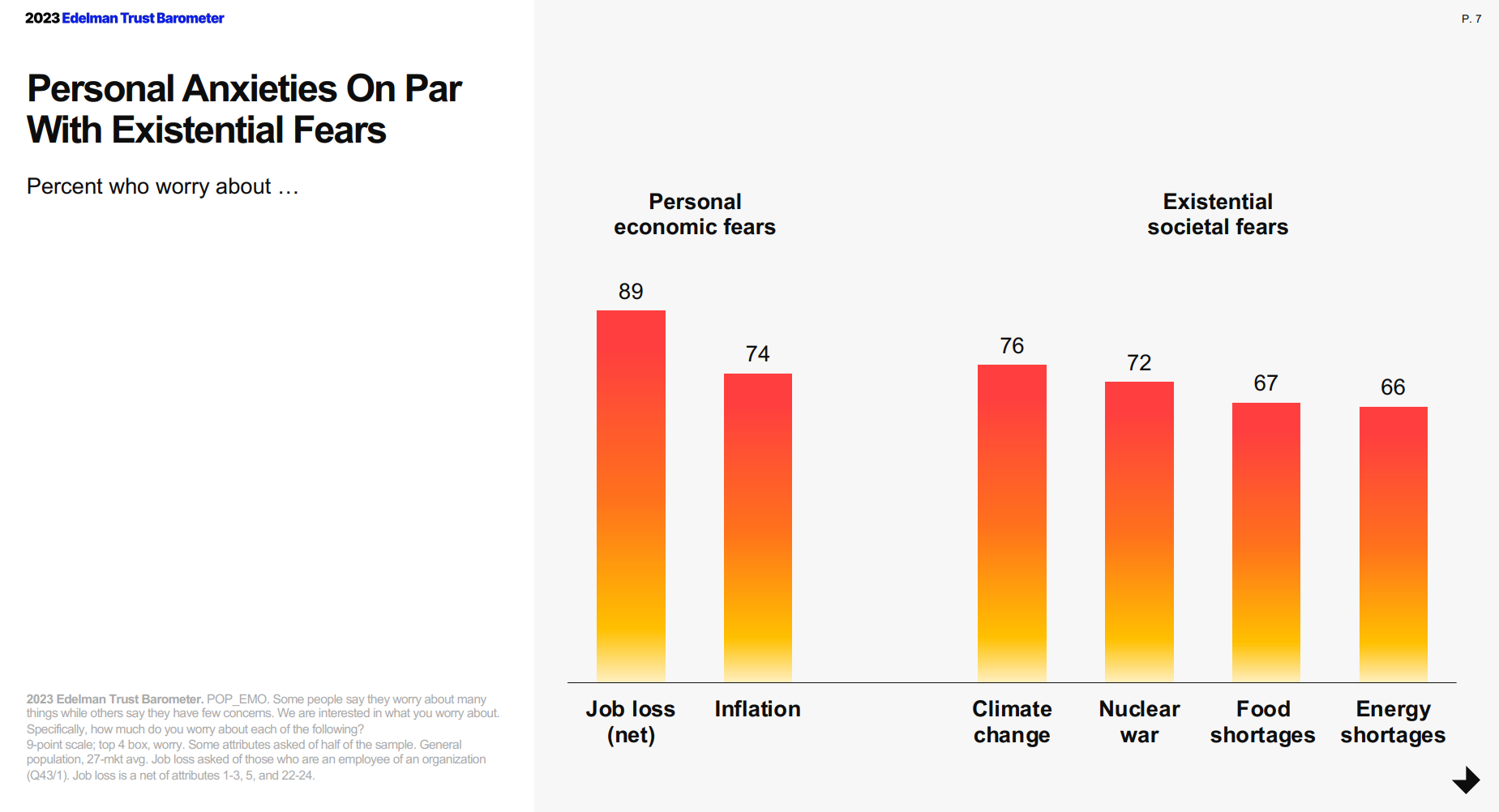
For the third year in a row, citizens in most of the world see business as the most-trusted institution, above government, media, and NGOs, found in the 2023 Edelman Trust Barometer, unveiled this week at the annual World Economic Forum in Davos, Switzerland. The Edelman team conducted this 23rd annual study in November 2022 in 28 countries, among over 32,000 people — some 1,150 residents per country polled. (Note that Russia, studied in the surveys between 2007 and 2022, was not included in the 2023 research). The first chart arrays
Of All Forms of Inequality, Injustice in Health Care is the Most Shocking and Inhumane: Listening to Martin Luther King, Jr.
Today as we appreciate the legacy of Martin Luther King, Jr., I post a photo of him in my hometown of Detroit in 1963, giving a preliminary version of the “I Have a Dream” speech he would deliver two months later in Washington, DC. Wisdom from the speech: “But now more than ever before, America is forced to grapple with this problem, for the shape of the world today does not afford us the luxury of an anemic democracy. The price that this nation must pay for the continued oppression and exploitation of the
What Do John Deere, L’Oreal and MedWand Have in Common? -> Human Security For All

An over-arching theme of the 2023 CES conference was Human Security for All, abbreviated as HS4A. And what, you might ask, do “human” and “security” have to do with the largest annual consumer technology conference, held last week in Las Vegas? Here’s what. “This is the first CES not only in the new post-pandemic or live-with-pandemic era. But this is the first time we actually had a theme. And that theme is focused on what technology can do to make the world better,” Gary Shapiro, CEO and President of the Consumer Technology Association, expressed in his opening speech for #CES2023.
Can Consumer Electronics Help Stem the Decline of U.S. Life-Years? A Preface for #CES2023
Life expectancy in the U.S. dropped nearly three years between 2019 and 2021, from close to 79 years down to 76. We ended 2022 with this new, sobering statistic from the Centers tor Disease Control (CDC). We begin 2023 with the opening of CES 2023, the world’s largest annual meet-up of consumer electronics innovators, companies, and retailers. How can digital health and other consumer-facing technologies help our health? First, consider the stark data point(s), and then we can better respond to the question’s answer in the Hot Points, below. In case you
How Will the “New” Health Economy Fare in a Macro-Economic Downturn?

What happens to a health care ecosystem when the volume of patients and revenues they generate decline? Add to that scenario a growing consensus for a likely recession in 2023. How would that further impact the micro-economy of health care? A report from Trilliant on the 2022 Trends Shaping the Health Economy helps to inform our response to that question. Start with Sanjula Jain’s bottom-line: that every health care stakeholder will be impacted by reduced yield. That’s the fewer patients, less revenue prediction, based on Trilliant’s 13 trends re-shaping the U.S. health
Life Expectancy Falls in the U.S., the Largest 2-Year Decline in 100 Years
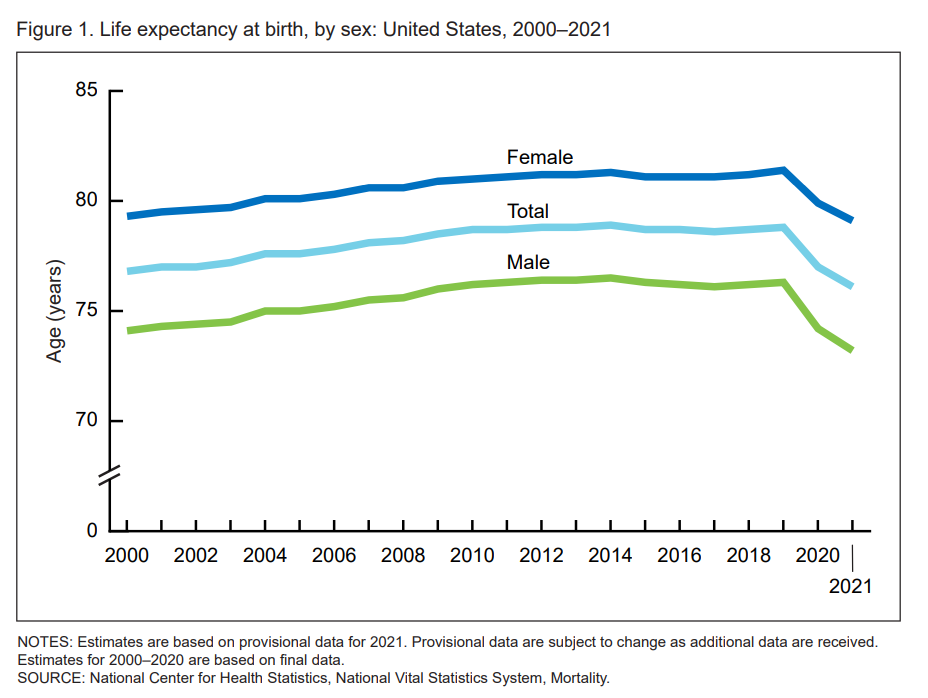
Life expectancy at birth in 2021 in the United States fell to 76.1 years, the lowest level since 1996. Men fared much worse than women, with 73,2 years of life expectancy versus 79.1 years for women, the latest research from the CDC’s National Center for Health Statistics revealed. In their Provisional Life Expectancy Estimates for 2021, the CDC kicks off a demographically detailed analysis with this simple line chart which graphs the dramatic decline in life expectancy at birth. The overall decline across gender and all race/ethnic groups was 2.7 years: 3.1 years
Your State as a Determinant of Health: Sharecare’s 2021 Community Well-Being Index

People whose sense of well-being shifted positively in the past two years are finding greater personal purpose and financial health, we see in Sharecare’s Community Well-Being Index – 2021 State Rankings Report. Sharecare has been annually tracking well-being across the 50 U.S. states since 2008. When the study launched, Well-Being Index evaluated five domains: physical, social, community, purpose, and financial. In 2020, Sharecare began a collaboration with the Boston University School of Public Health to expand the Index, including drivers of health such as, Healthcare access (like physician supply per 1,000
The 2022 US Health System Report Card: Pretty Terrific If You Live in Hawaii or Massachusetts
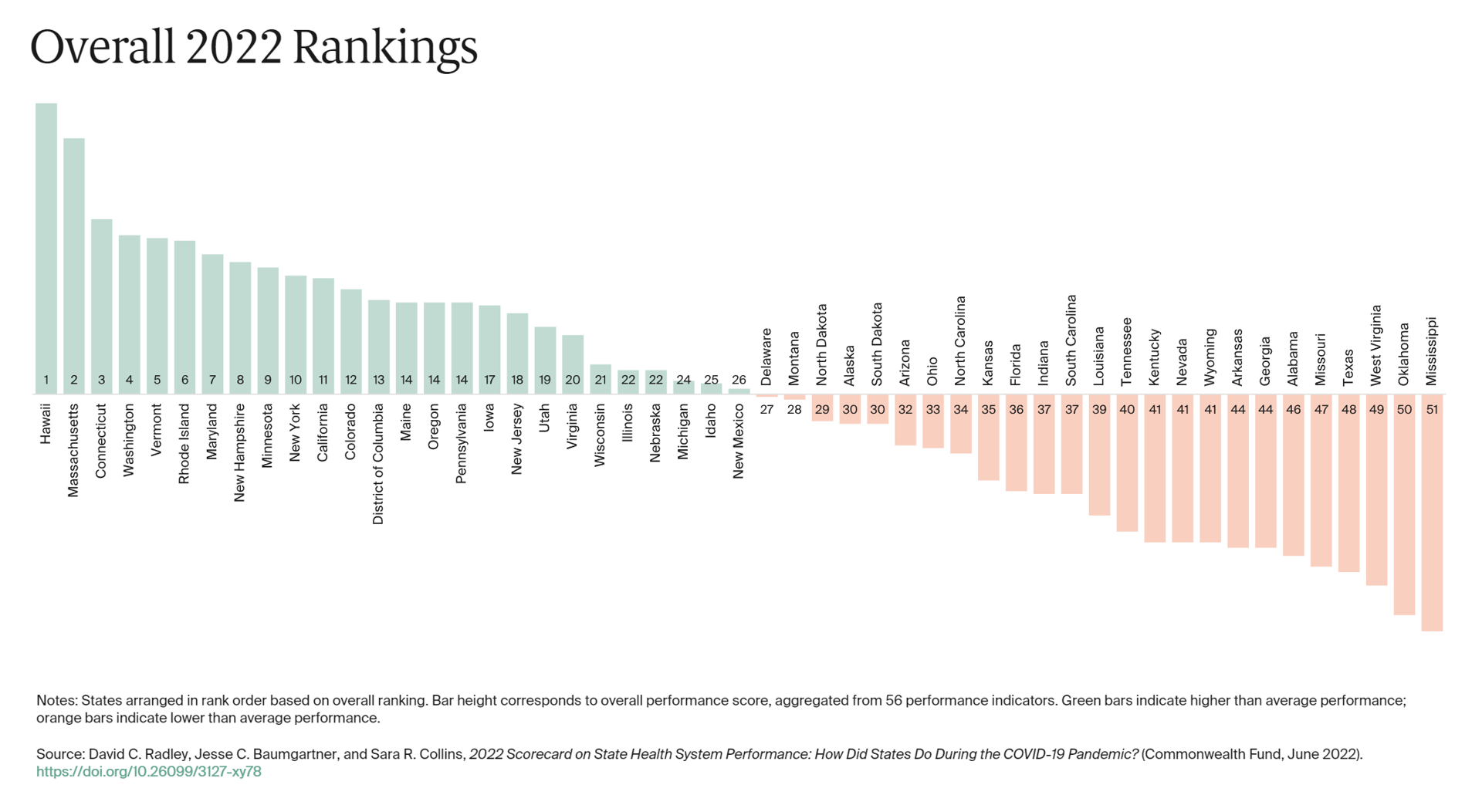
The best U.S. states to live in for health and health care are Hawaii, Massachusetts, Connecticut, Washington, Vermont, Rhode Island, and Maryland… Those are the top health system rankings in the new 2022 Scorecard on State Health System Performance annual report from the Commonwealth Fund. If you live in Mississippi, Oklahoma, West Virginia, Texas, Missouri, Alabama, Georgia, or Arkansas, your health care and outcomes are less likely to be top-notch, the Fund’s research concluded. The Commonwealth Fund has conducted this study since 2006, assessing a range
Health is Our Most Important Relationship: Inconvenient Truths from MRM/McCann Truth Central

We’ve hit a great “healthcare trust” recession around the world, translating into lower multiple points of medical ‘facts’ and pseudoscience, lower adherence to therapeutic regimens, and clinician burnout that has compromised medicine as the team sport it ideally should be. And that’s just one of five inconvenient truths unearthed in The Truth About Our Relationships with Health, the first in a series of papers that MRM is developing to, in their words, “look at the truths pr7eventing us from achieving a better relationship with our own health and with those along our health journey.” This report from MRM analyzes research
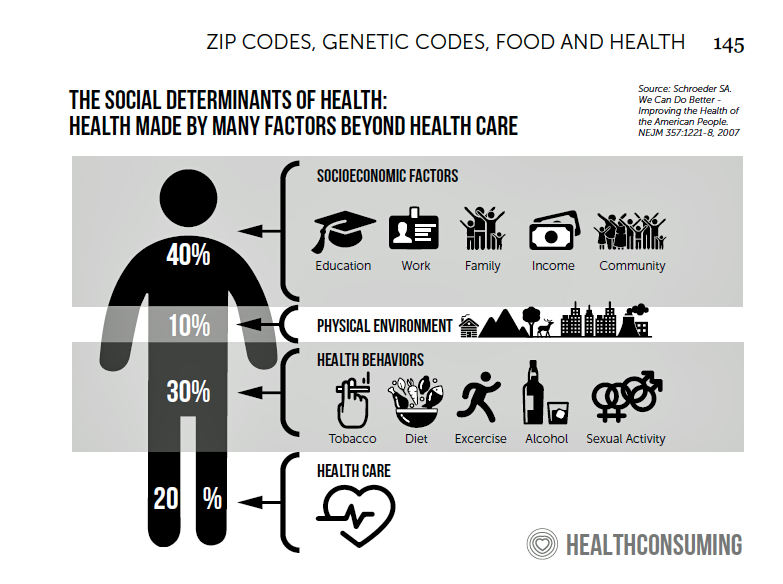
How Business Can Bolster Determinants of Health: The Marmot Review for Industry

“Until now, focus on….the social determinants of health has been for government and civil society. The private sector has not been involved in the discussion or, worse, has been seen as part of the problem. It is time this changed,” asserts the report, The Business of Health Equity: The Marmot Review for Industry, sponsored by Legal & General in collaboration with University College London (UCL) Institute of Health Equity, led by Sir Michael Marmot. Sir Michael has been researching and writing about social determinants of health and health equity for decades, culminating publications
McKinsey’s Six Shifts To Add Life to Years — and One More to Consider
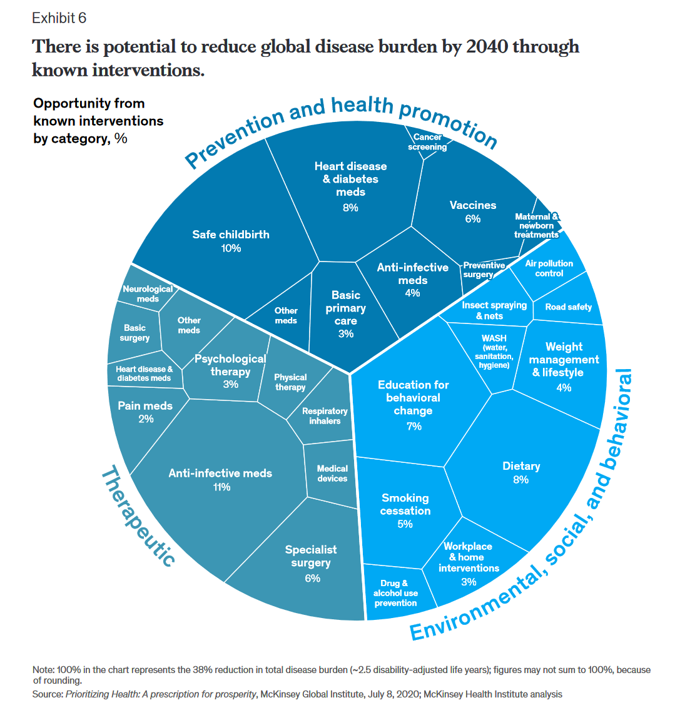
People spend one-half of their lives in “less-than-good health,” we learn early in the paper, Adding years to life and life to years from the McKinsey Health Institute. In this data-rich essay, the McKinsey team at MHI sets out an agenda that could help us add 45 billion extra years of higher-quality life equal to an average of six years per person (depending on your country and population demographics). The first graphic from the report illustrates four dimensions of health and the factors underneath each of them that can bolster or diminish our well-being: personal behaviors (such as sleep and diet),
People in the U.S. Without the Internet Were More Likely To Die in the Pandemic
Access to the Internet has been a key determinant of health — or more aptly, death — during the COVID-19 pandemic. Americans lacked Internet access were more likely to die due to complications from the coronavirus, according to a study published in JAMA Network Open this month. The study’s key finding was that for every additional 1% of people living in a county who have access to the Internet, between 2.4 and 6.0 COVID-19 deaths per 100,000 were preventable. The paper asserts that, “More awareness is needed about the essential asset of technological access to reliable information, remote work, schooling
On Valentine’s Day 2022, Let’s Remember That Love is a Social Determinant of Health

While love can’t solve all of the world’s problems, it is absolutely a basic human need and a positive force for health and well-being. For today’s Health Populi blog, I have curated a big hug-full of posts I’ve written over the years building the evidence base of love as a determinant of health. As a sidebar, the graphic you see here — my “WiFi Heart” — was purposefully commissioned to my web designer to incorporate elements of love and connectivity. Wishing you all the blessing of love in your life, in all of its glorious and health-ful forms…XO JSK My
The Wellness Economy in 2022 Finds Health Consumers Moving from Feel-Good Luxury to Personal Survival Tactics
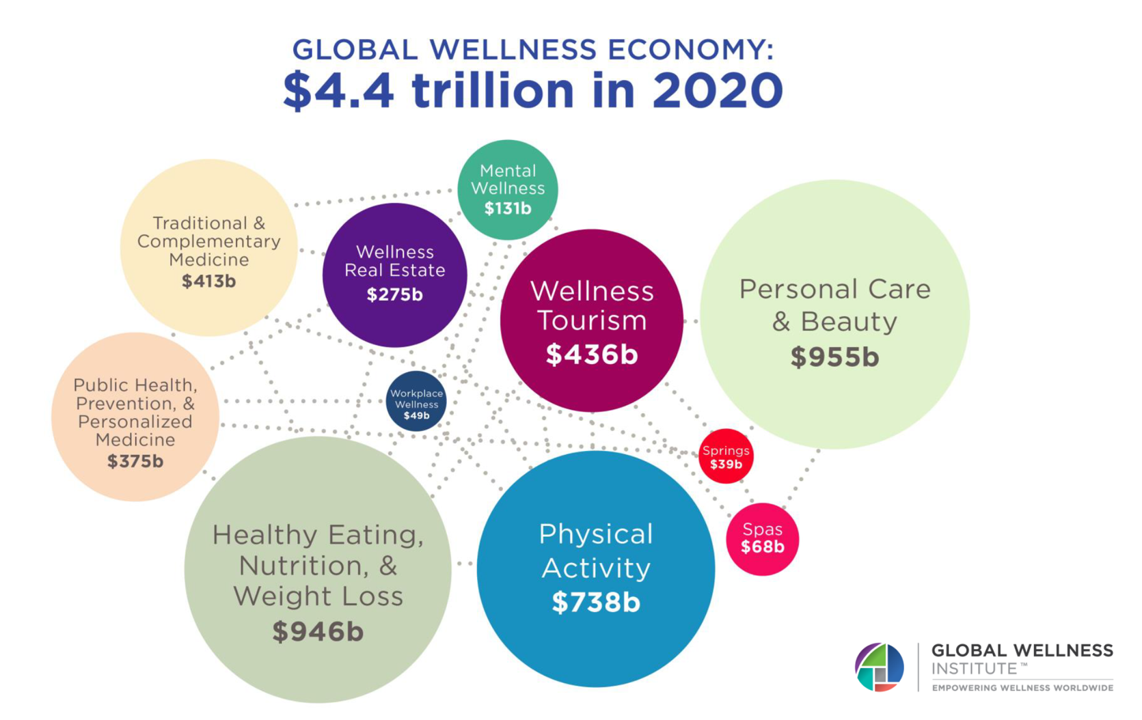
The Future of Wellness in 2022 is, “shifting from a ‘feel-good’ luxury to survivalism as people seek resilience,” based on the Global Wellness Institute’s forecast on this year’s look into self-care and consumer’s spending on health beyond medical care — looking beyond COVID-19. GWI published two research papers this week on The Future of Wellness and The Global Wellness Economy‘s country rankings as of February 2021. I welcomed the opportunity to spend time for a deep dive into the trends and findings with the GWI community yesterday exploring all of the data, listening through my health economics-consumer-technology lens. First, consider
Effective Health Spending Is An Investment, Not a Cost: the Bottom-Line from OECD Health at a Glance 2021
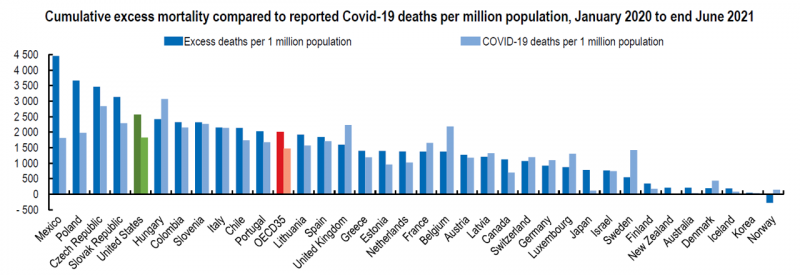
“The pandemic has shown that effective health spending is an investment, not a cost to be contained: stronger, more resilient health systems protect both populations and economies,” the OECD states in the first paragraph of the organization’s perennially-updated report, Health at a Glance 2021. This version of the global report incorporates public health data from the “OECD35,” 35 nations from “A” to “U” (Australia to United States) quantifying excess deaths experienced during the COVID-19 pandemic, the obesity epidemic, mental and behavioral health burdens, and health care spending, among many other metrics. The first chart illustrates that calculation of excess deaths,
Be Mindful About What Makes Health at HLTH
“More than a year and a half into the COVID-19 outbreak, the recent spread of the highly transmissible delta variant in the United States has extended severe financial and health problems in the lives of many households across the country — disproportionately impacting people of color and people with low income,” reports Household Experiences in America During the Delta Variant Outbreak, a new analysis from the Robert Wood Johnson Foundation, NPR, and the Harvard Chan School of Public Health. As the HLTH conference convenes over 6,000 digital health innovators live, in person, in Boston in the wake of the delta
Consider Mental Health Equity on World Mental Health Day
COVID-19 exacted a toll on health citizens’ mental health, worsening a public health challenge that was already acute before the pandemic. It’s World Mental Health Day, an event marked by global and local stakeholders across the mental health ecosystem. On the global front, the World Health Organization (WHO) describes the universal phenomenon and burden of mental health on the Earth’s people… Nearly 1 billion people have a mental disorder Depression is a leading cause of disability worldwide, impacting about 5% of the world’s population People with severe mental disorders like schizophrenia tend to die as much as 20 years earlier
Health Disparities in America: JAMA Talks Structural Racism in U.S. Health Care

“Racial and ethnic inequities in the US health care system have been unremitting since the beginning of the country. In the 19th and 20th centuries, segregated black hospitals were emblematic of separate but unequal health care,” begins the editorial introducing an entire issue of JAMA dedicated to racial and ethnic disparities and inequities in medicine and health care, published August 17, 2021. This is not your typical edition of the Journal of the American Medical Association. The coronavirus pandemic has changed so many aspects of American health care for so many people, including doctors. Since the second quarter of 2020,
Regulation, Reimbursement, and Interoperability Block Health Systems’ Digital Transformation – The State of Healthcare in 2021 From HIMSS
There is no doubt that the COVID-19 pandemic motivated health care providers, payers, and patients to adopt digital tools and contact-less services, allowing people to deliver and receive medical care. Still, 18 months into the pandemic, now endemic and in its fourth wave of cases spiking around the world and in many parts of the U.S., some aspects of “digital transformation” seem not to have fully transformed American healthcare, we learn in HIMSS’s annual 2021 State of Healthcare Report. HIMSS collaborated with the organizations Trust Accenture, The Chartix Group, and ZS on this year’s research. Nine in ten clinicians have recommended
CVS Finds Differences in Mental and Behavioral Health Among Men Vs. Women in the Pandemic
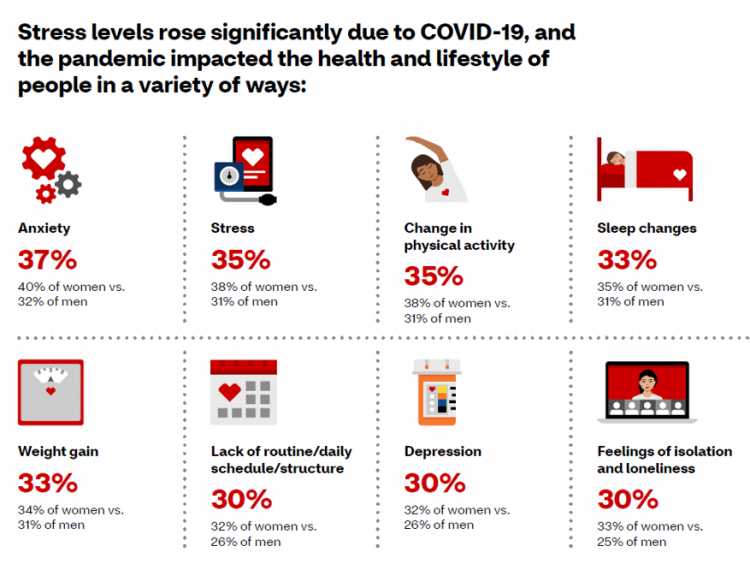
As the COVID-19 pandemic shifts to a more endemic phase — becoming part of peoples’ everyday life for months to come — impacts on peoples’ mental health will persist, according to new research from CVS Health in the company’s annual Health Care Insights Study. CVS conducted the annual Health Care Insights Study among 1,000 U.S. adults in March 2021. To complement the consumer study, an additional survey was undertaken among 400 health care providers including primary care physicians and specialists, nurse practitioners, physician assistants, RNs and pharmacists. CVS has been tracking the growing trend of health care consumerism in the
Digital Inclusion As Upstream Health Investment
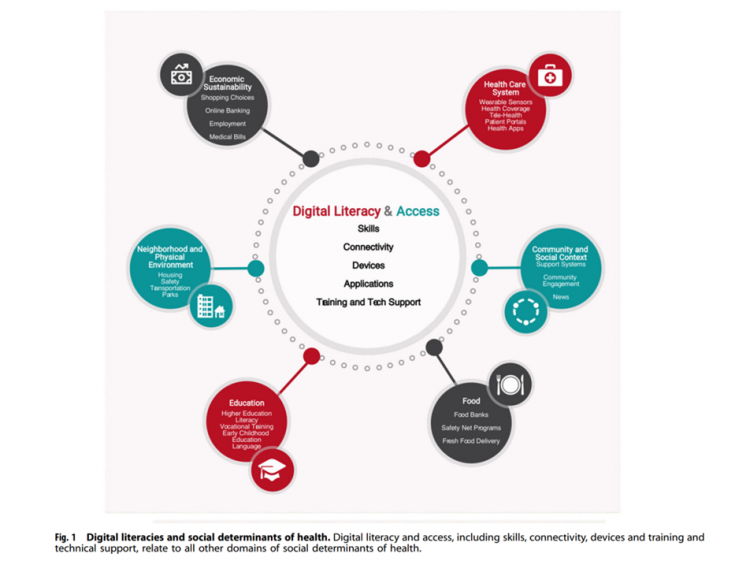
Without access to connectivity during the pandemic, too many people could not work for their living, attend school and learn, connect with loved ones, or get health care. The COVID-19 era has shined a bright light on what some of us have been saying since the advent of the Internet’s emergence in health care: that digital literacies and connectivity are “super social determinants of health” because they underpin other social determinants of health, discussed in Digital inclusion as a social determinant of health, published in Nature’s npj Digital Medicine. On the downside, lack of access to digital tools and literacies
The Healthiest Communities in the U.S. After the Pandemic – U.S. News & Aetna Foundation’s Post-COVID Lists

Some of America’s least-healthy communities are also those that index greater for vaccine hesitancy and other risks for well-being, found in U.S. News & World Report’s 2021 Healthiest Communities Rankings. U.S. News collaborated with the Aetna Foundation, CVS Health’s philanthropic arm, in this fourth annual list of the top geographies for well-being in the U.S. Six of the top ten healthiest towns in America are located in the state of Colorado. But #1 belongs to Los Alamos County, New Mexico, which also ranked first in ___. Beyond Colorado and New Mexico, we find that Virginia fared well for health in
5.5 Million Years of Life Will Be Lost Due to COVID-19 in the U.S. in 2020
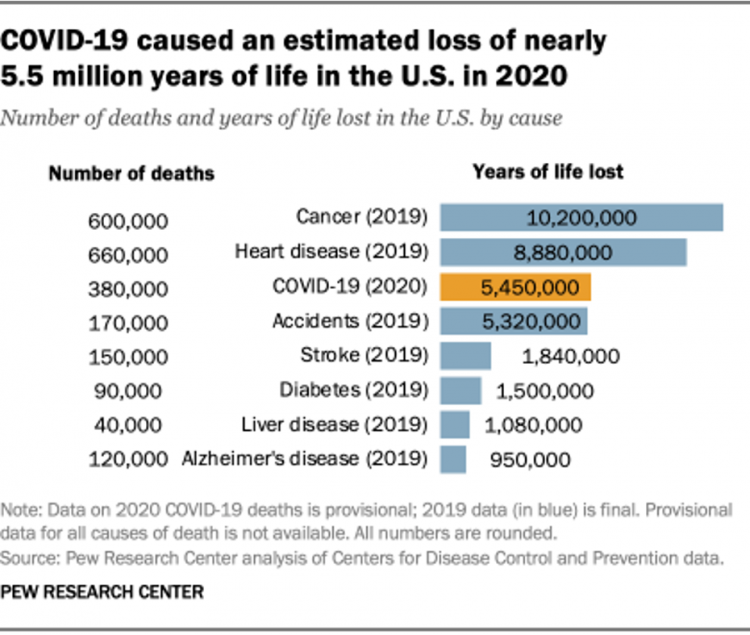
In 2020 in the U.S., 380,000 people are expected to die due to COVID-19. These people lost due to the coronavirus would, collectively, have lived another 5.5 million life-years would they not have succumbed to the virus. COVID-19 has cut lives short relative to their life expectancy, calculated in an analysis by the Pew Research Center based on CDC data from 2019 and 2020, coupled with additional statistics on life expectancy by age and gender. The bottom-line from the Pew Research Center’s analysis, simply stated, is that, “The pandemic…has killed many Americans who otherwise might have expected to live for
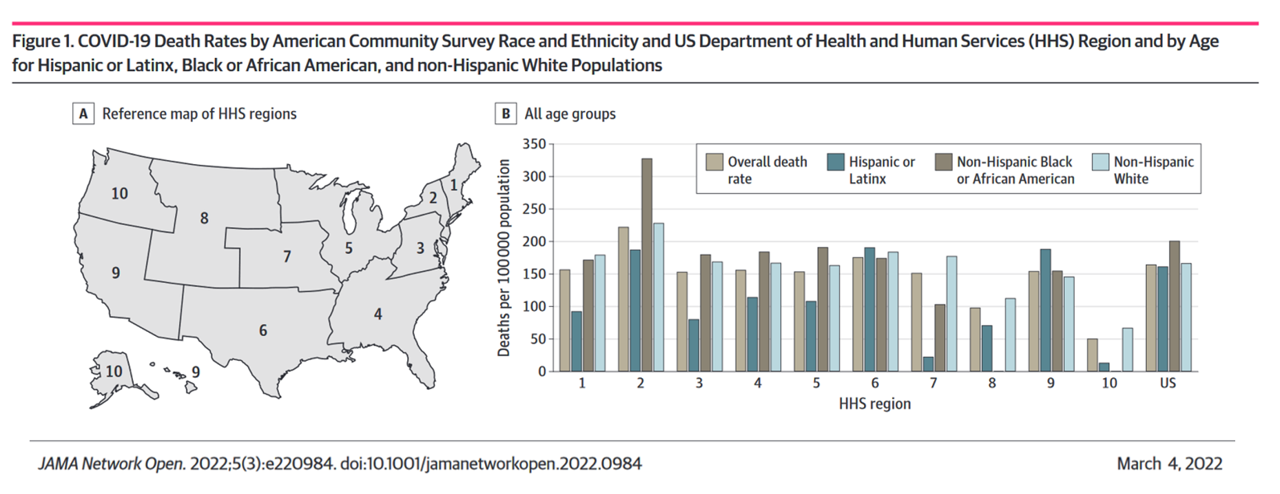
Health Disparities and the Risks of Social Determinants for COVID-19 – 14 Months of Evidence
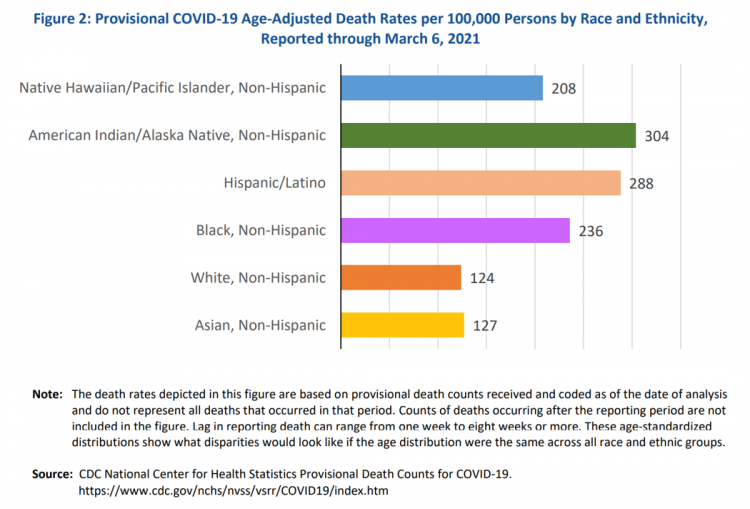
In April 2020, the U.S. Centers for Disease Control issued a report featuring evidence that in the month of March 2020, the coronavirus pandemic was not an equal-opportunity killer. Within just a couple of months of COVID-19 emerging in America, it became clear that health disparities were evident in outcomes due to complications from the coronavirus. An update from that early look at differences in COVID-19 diagnoses and mortality rates was published in Health Disparities by Race and Ethnicity During the COVID-19 Pandemic: Current Evidence and Policy Approaches, In this report, the Assistant Secretary for Planning and Evaluation, part of
Stress in America, One Year into the Pandemic – an APA Update on Parents, Healthcare Workers, and Black Americans
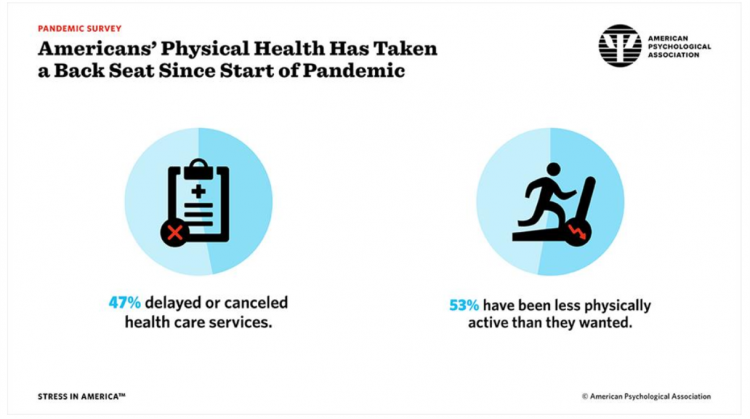
A Year into our collective coronavirus experience, Americans remain stressed, with physical health taking a back seat to our daily grinds based on the 2021 Stress in America survey from the American Psychological Association (APA). The APA has been updating us on U.S.-stress for several years, and more frequently since the start of the COVID-19 pandemic at the start of 2020. In their latest report, APA updates their previous profiles of Americans’ stress looking into different demographic groups and coping mechanisms. The topline, across all adults living in America, is that one-half have delayed or cancelled health care services. One-half has
A BA Degree as Prescription for a Longer Life – Update on Deaths of Despair from Deaton and Case
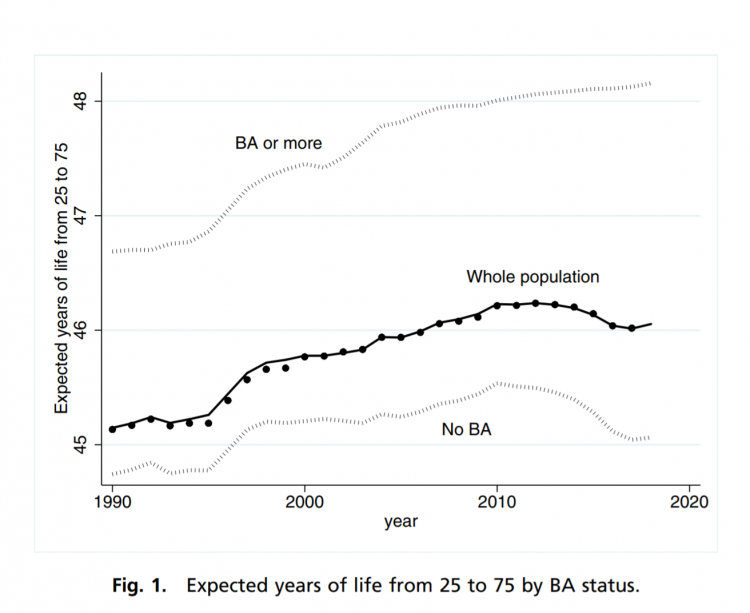
“Without a four-year college diploma, it is increasingly difficult to build a meaningful and successful life in the United States,” according to an essay in PNAS, Life expectancy in adulthood is falling for those without a BA degree, but as educational gaps have widened, racial gaps have narrowed by Anne Case and Angus Deaton. Case and Deaton have done extensive research on the phenomenon of Deaths of Despair, the growing epidemic of mortality among people due to accidents, drug overdoses, and suicide. Case and Deaton wrote the book on Deaths of Despair (detailed here in Health Populi), Case and Deaton
Americans Lost Future Life-Years in 2020: How Much Life Was Lost Depends on the Color of One’s Skin
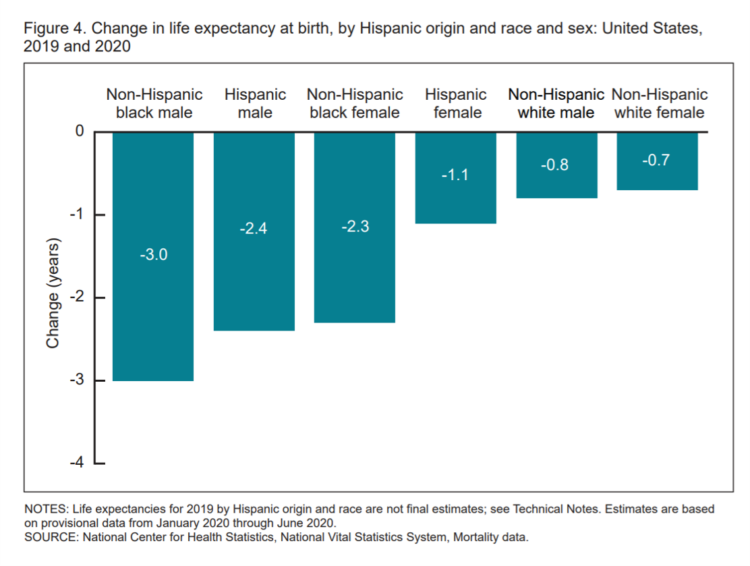
Some people remark about 2020 being a “lost year” in the wake of the coronavirus pandemic. That happens to be a true statement, sadly not in jest: in the U.S., life expectancy at birth fell by one full year over the first half of 2020 compared with 2019, to 77.8 years. In 2019, life expectancy at birth was 78.8 years, according to data shared by the National Center for Health Statistics (NCHS), part of the Centers for Disease Control and Prevention (CDC). Life expectancy at birth declined for both females and males, shown in the first chart. The differences between
Three in Four People Avoiding Health Care in the Pandemic Have Had Chronic Conditions
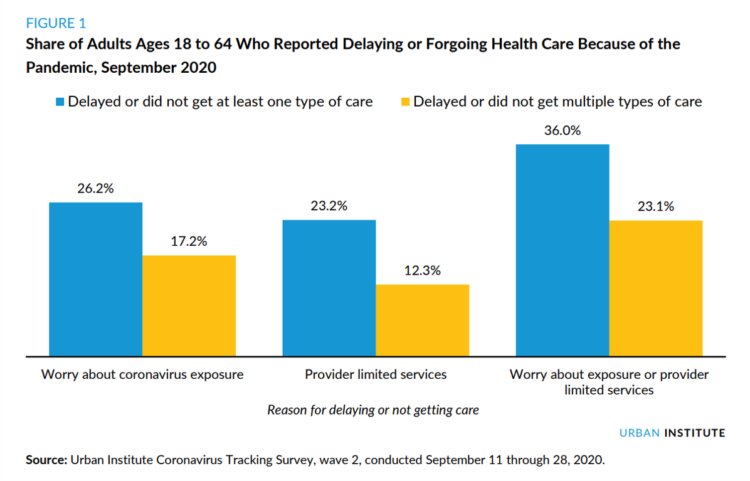
By the autumn of 2020, U.S. physicians grew concerned that patients who were avoiding visits to doctor’s offices were missing care for chronic conditions, discussed in in Delayed and Forgone Health Care for Nonelderly Adults during the COVID-19 Pandemic from the Urban Institute. More than three-fourths of people who delayed or forewent care had at least one chronic health condition. The pandemic may have led to excess deaths from diabetes, dementia, hypertension, heart disease, and stroke, as well as record drug overdoses in the 12 months ending in May 2020. In their JAMA editorial on these data, Dr. Bauchner and
The Pandemic Has Been a Shock to Our System – Learning from Known
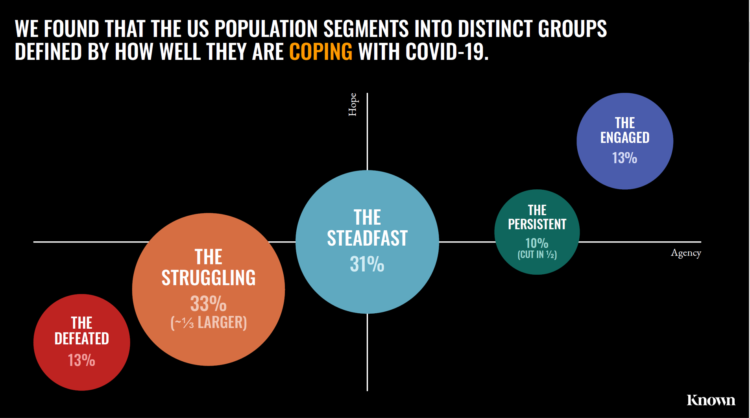
The coronavirus pandemic has been a shock to people across all aspects of everyday living, for older and younger people, for work and school, for entertainment and travel — all impacting our hearts, minds, and wallets. “As the bedrock of daily life was shaken, uncertainty predictably emerged as the prevailing emotion of our time but this universal problem was eliciting a highly differentiated reaction in different people,” Kern Schireson, CEO of Known, observed. His company has conducted a large quantitative and qualitative research program culminating in a first report, The Human Condition 2020: A Shock To The System. Known’s team of
Stress in America, Like COVID-19, Impacts All Americans
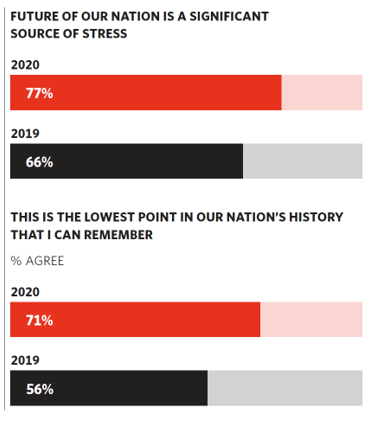
With thirteen days to go until the U.S. #2020Elections day, 3rd November, three in four Americans say the future of America is a significant source of stress, according to the latest Stress in America 2020 study from the American Psychological Association. Furthermore, seven in 10 U.S. adults believe that “now” is the lowest point in the nation’s history that they can remember. “We are facing a national mental health crisis that could yield serious health and social consequences for years to come,” APA introduces their latest read into stressed-out America. Two in three people in the U.S. say that the
Our Home Is Our Health Hub: CTA and CHI Align to Address Digital and Health Equity

In the pandemic, I’ve been weaving together data to better understand how people as consumers are being re-shaped in daily life across their Maslow Hierarchies of Needs. One of those basic needs has been digital connectivity. People of color have faced many disparities in the wake of the pandemic: the virus itself, exacting greater rates of mortality and morbidity being the most obvious, dramatic inequity. Another has been digital inequity. Black people have had a more difficult time paying for phone and Internet connections during the COVID-19 crisis, we learned in a Morning Consult poll fielded in June 2020. In
Behavioral Health Side-Effects in the COVID Era
“This surge of people experiencing acute behavioral health problems…has the potential to further impact the healthcare system for years to come,” a report from McKinsey expects looking at the hidden costs of COVID-19’s impact on U.S. health care. The coronavirus pandemic has taken a toll on Americans’ mental health, with anxiety and depression growing as a side-effect to worries about the virus itself, the long Great Lockdown in much of the country, and the economic recession that has particularly impacted women and people of color. I covered depression impacts due to COVID-19 here in Health Populi yesterday, and wanted to
The Mental Health Impacts of COVID-19 – Trauma- and Stress-Related Disorders in the Pandemic
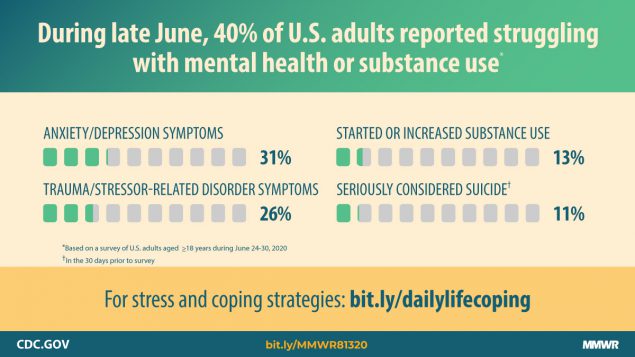
The CDC calculated that some 200,000 American lives would be lost to the coronavirus pandemic by Labor Day weekend 2020. Beyond the tragic mortality in the U.S. come morbidity impacts hitting mental health in America, hard. And some people are being hit-harder than others, a report from the Centers for Disease Control details. Overall, 4 in 10 people in the U.S. reported at least one adverse mental or behavioral health symptom in the last week of June 2020. These symptoms included anxiety disorder, depressive disorder, COVID-19 related trauma- or stress-related disorder (TSRD), substance use (either starting or increasing), and serious
Juneteenth 2020: Inequality and Injustice in Health Care in America
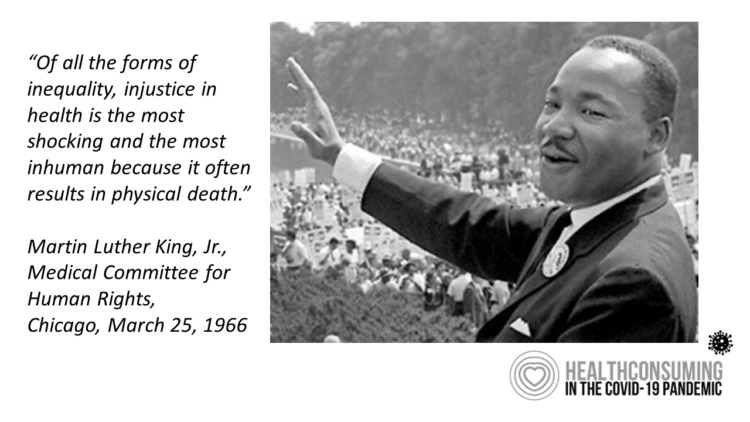
“Of all the forms of inequality, injustice in health is the most shocking and the most inhuman because it often results in physical death,” Martin Luther King, Jr., asserted at the second meeting of the Medical Committee for Human Rights in Chicago on March 25, 1966. This quote has been shortened over the five+ decades since Dr. King told this truth, to the short-hand, “Of all the forms of inequality, injustice in health care is the most shocking and inhumane.” Professor Charlene Galarneau recently enlightened me on Dr. King’s original statement in her seminal essay, “Getting King’s Words Right.” Among
How COVID-19 Is Driving More Deaths of Despair
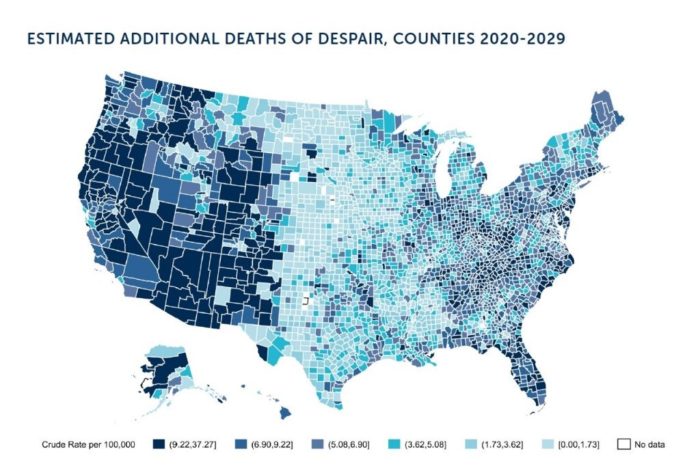
In the current state of the COVID-19 pandemic, we all feel like we are living in desperate times. If you are a person at-risk of dying a Death of Despair, you’re even more at-risk of doing so in the wake of the Coronavirus in America. Demonstrating this sad fact of U.S. life, the Well Being Trust and Robert Graham Center published Projected Deaths of Despair from COVID-19. The analysis quantifies the impact of isolation and loneliness combined with the dramatic economic downturn and mass unemployment with the worsening of mental illness and income inequity on the epidemic of Deaths of
The Coronavirus Impact on American Life, Part 2 – Our Mental Health
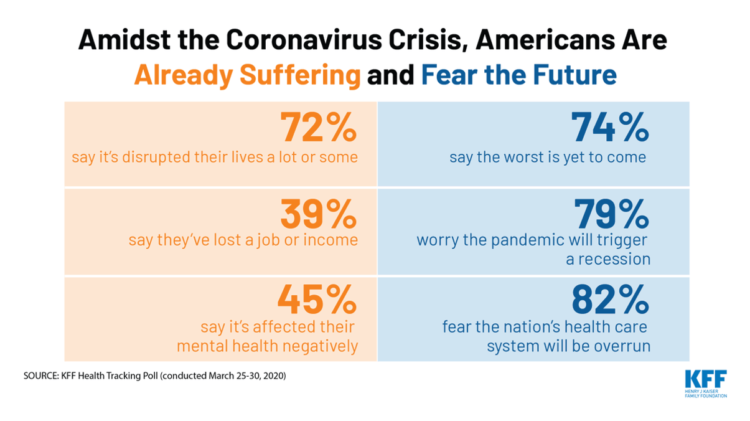
As the coronavirus pandemic’s curve of infected Americans ratchets up in the U.S., people are seeking comfort from listening to Dolly Parton’s bedtime stories, crushing on Dr. Anthony Fauci’s science-wrapped-with-empathy, and streaming the Tiger King on Netflix. These and other self-care tactics are taking hold in the U.S. as most people are “social distancing” or sheltering in place, based on numbers from the early April 2020 Kaiser Family Foundation health tracking poll on the impact of the coronavirus on American life. While the collective practice of #StayHome to #FlattenTheCurve is the best-practice advice from the science leaders at CDC, the NIAID
The Book on Deaths of Despair – Deaton & Case On Education, Pain, Work and the Future of Capitalism
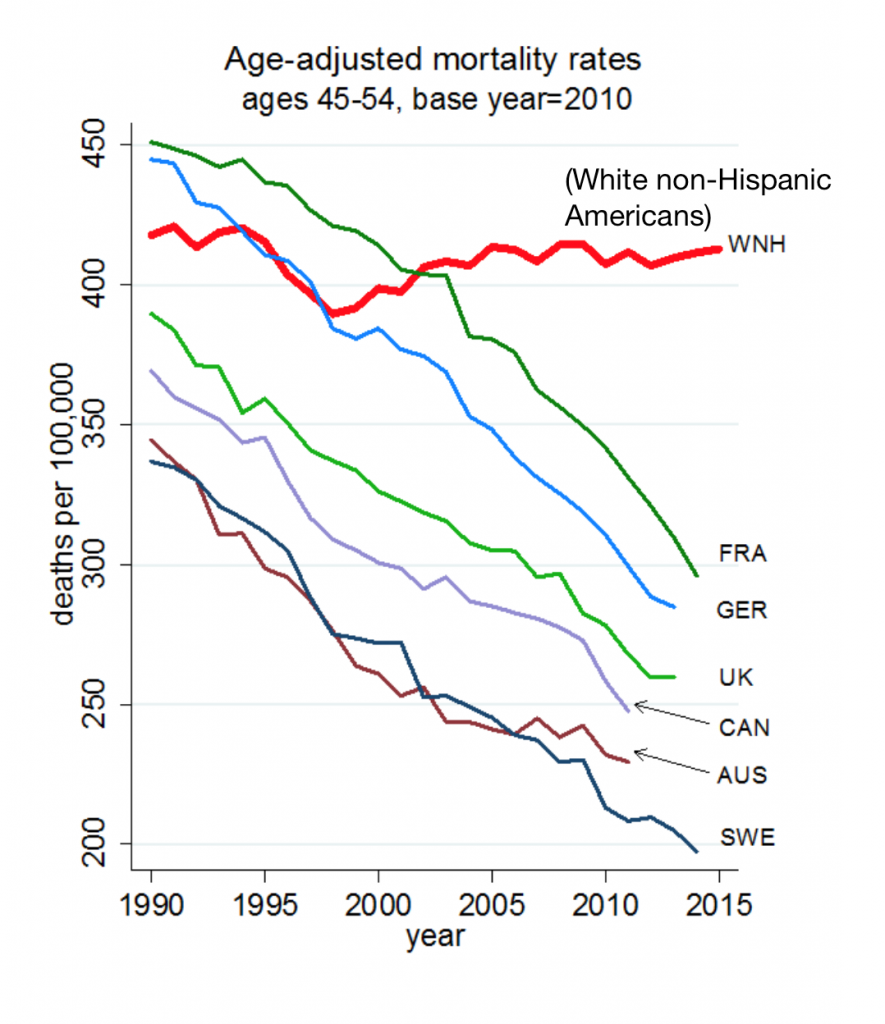
Anne Case and Angus Deaton were working in a cabin in Montana the summer of 2014. Upon analyzing mortality data from the U.S. Centers for Disease Control, they noticed that death rates were rising among middle-aged white people. “We must have hit a wrong key,” they note in the introduction of their book, Deaths of Despair and the Future of Capitalism. This reversal of life span in America ran counter to a decades-long trend of lower mortality in the U.S., a 20th century accomplishment, Case and Deaton recount. In the 300 pages that follow, the researchers deeply dive into and
The High Cost-of-Thriving and the Evolving Social Contract for Health Care
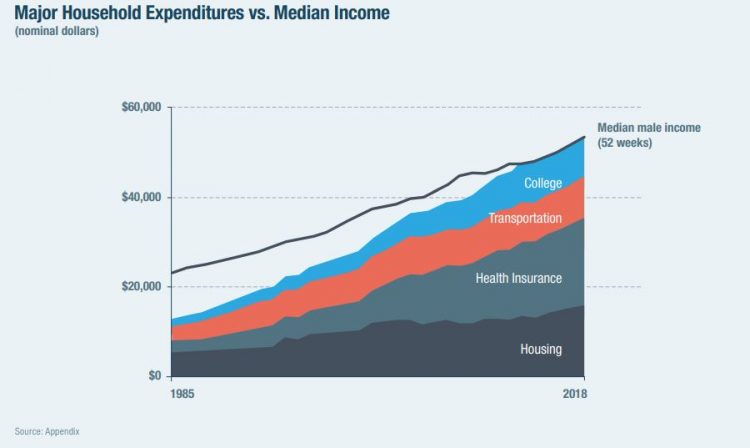
Millions of Americans have to work 53 weeks to cover a year’s worth of household expenses. Most Americans haven’t saved much for their retirement. Furthermore, the bullish macroeconomic outlook for the U.S. in early 2020 hasn’t translated into individual American’s optimism for their own family budgets. (Sidebar and caveat: yesterday was the fourth day in a row of the U.S. financial markets losing as much as 10% of market cap, so the global economic outlook is being revised downward by the likes of Goldman Sachs, Vanguard, and Morningstar, among other financial market prognosticators. MarketWatch called this week the worst market
Most Americans Regardless of Income Say It’s Unfair for Wealthier People to Get Better Health Care
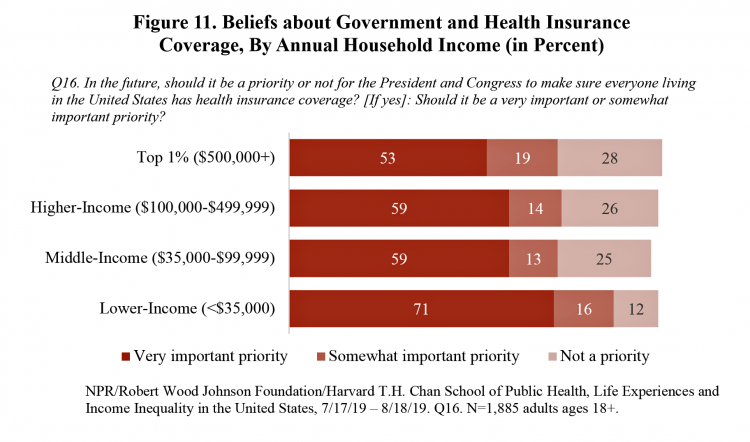
In America, earning lower or middle incomes is a risk factor for having trouble accessing health care and/or paying for it. But most Americans, rich or not, believe that it’s unfair for wealthier people to get better health care, according to a January 2020 poll from NPR, the Robert Wood Johnson Foundation and Harvard Chan School of Public Health, Life Experiences and Income Equality in the United States. The survey was conducted in July and August 2019 among 1,885 U.S. adults 18 or older. Throughout the study, note the four annual household income categories gauged in the research: Top 1%
The Suicide Rate in America Increased by 40% between 2000 and 2017. Blue Collar Workers Were Much More At Risk.
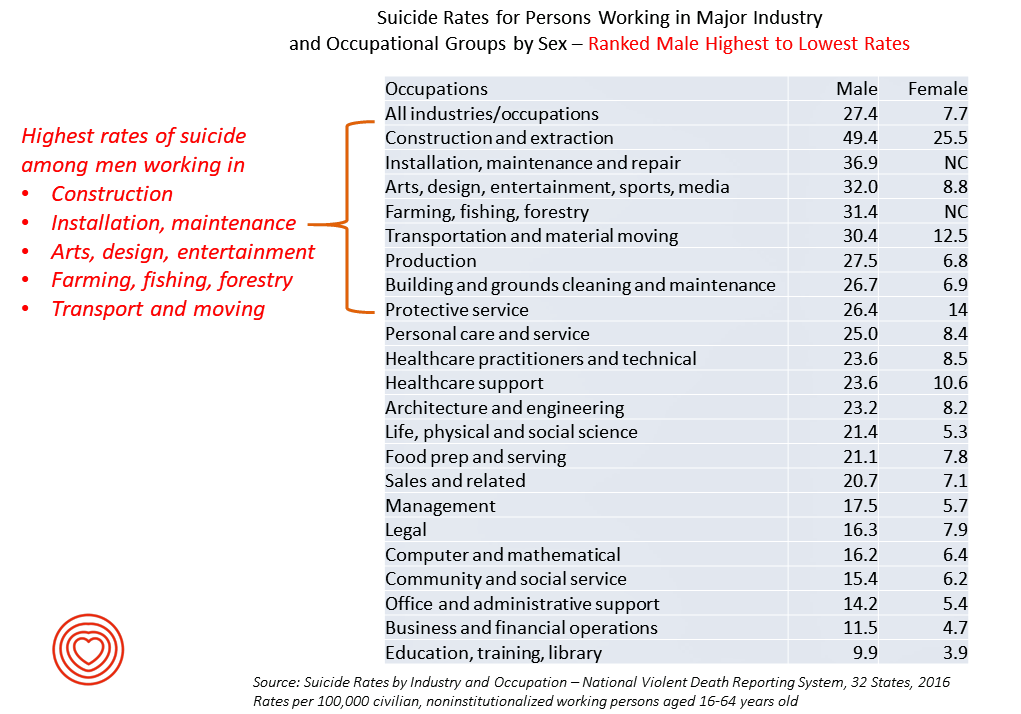
The rate of suicide in the U.S. rose from 12.9 per 100,000 population to 18.0 between 2000 and 2017, a 40% increase. Those workers most at-risk for suiciding were men working in construction and mining, maintenance, arts/design/entertainment/sports/media, farming and fishing, and transportation. For women, working in construction and mining, protective service, transportation, healthcare (support and practice), the arts and entertainment, and personal care put them at higher risk of suicide. The latest report from the CDC on Suicide Rates by Industry and Occupation provides a current analysis of the National Violent Death Reporting System which collects data from 32 states,
Consumers Seek Benefits From Food, a Personal Social Determinant of Health
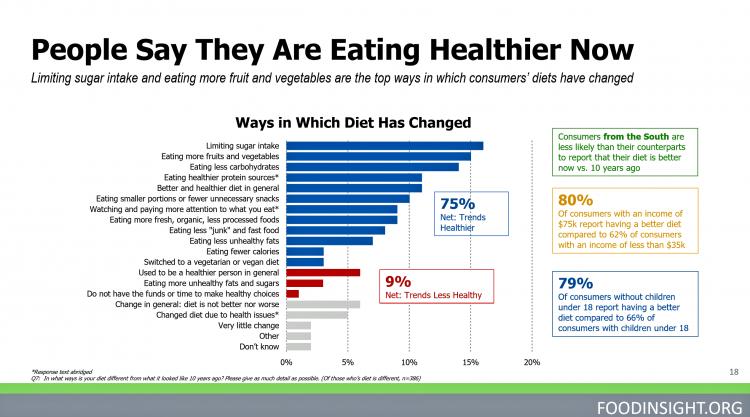
As consumers in the U.S. wrestle with accessing and paying for medical benefits, there’s another sort of health benefit people increasingly understand, embrace, and consume: food-as-medicine. More people are taking on the role of health consumers as they spend more out-of-pocket on medical care and insurance, and seeking food to bolster their health is part of this behavior change. One in four Americans seek health benefits from food, those who don’t still seek the opportunity to use food for weight loss goals, heart health and energy boosting, according to the 2019 Food & Health Survey from the International Food Information





 I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for