Health Care and the Democratic Debates – Round 2 – Battle Royale for M4All vs Medicare for All Who Want It – What It Means for Industry

Looking at this photo of the 2020 Democratic Party Presidential candidate debater line-up might give you a déjà vu feeling, a repeat of the night-before debate. But this was Round 2 of the debate, with ten more White House aspirants sharing views — sometimes sparring — on issues of immigration, economic justice, climate change, and once again health care playing a starring role from the start of the two-hour event. The line-up from left to write included: Marianne Williamson. author and spiritual advisor John Hickenlooper, former Governor of Colorado Andrew Yang. tech company executive Pete Buttigieg, Mayor of South Bend,
IKEA Garners the Top Health & Wellness Award at Cannes Lions 2019 – the Expanding Health/Care Ecosystem

“Health is now everyone’s business,” Shaheed Peera, Executive Creative Director of Publicis LifeBrands, said this week at the 2019 Cannes Lions awards. Shaheed also led the Health & Wellness jury at Cannes Lions 2019, the mission of which is to, in the words of the award’s portal, “celebrate creativity for personal wellbeing.” The Grand Prix Lions award for Health & Wellness went to IKEA for the company’s ThisAbles campaign. ThisAbles is a project pioneered by IKEA’s team in Israel, looking to improve everyday living for people with special needs through well-designed IKEA products. IKEA collaborated with non-profit organizations to develop
Americans Could Foster a Health Consumer Movement, Families USA Envisions
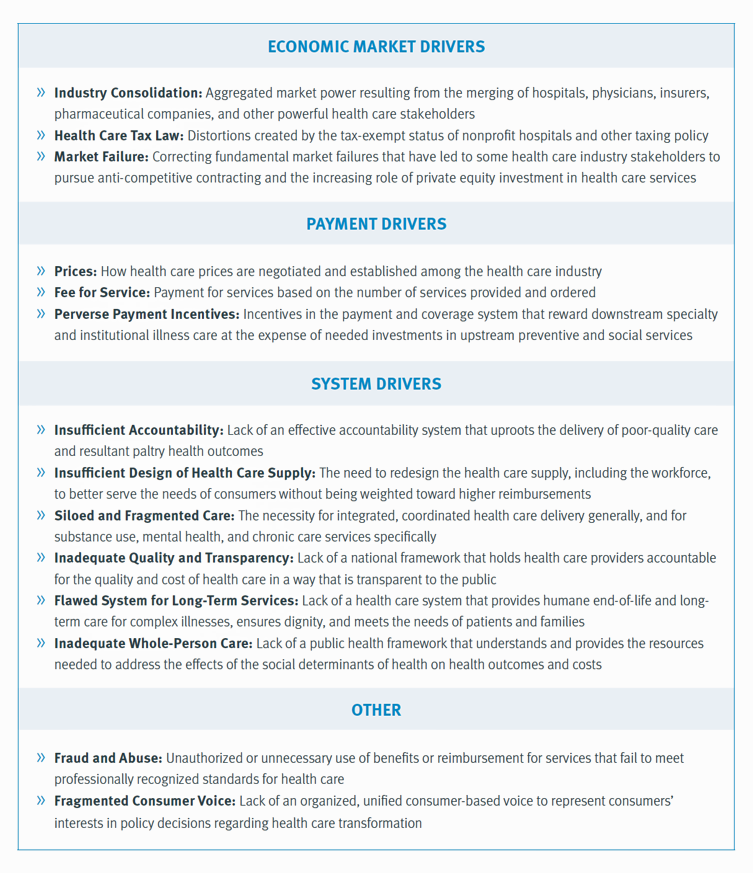
Employers, health care providers, unions, leaders and — first and foremost, consumers — must come together to build a more accessible, affordable health care system in America, proposes a call-to-action fostered by a Families USA coalition called Consumers First: The Alliance to Make the Health Care System Work for Everyone. The diverse partners in this Alliance include the American Academy of Family Physicians, AFSCME (the largest public service employees’ union in the U.S.), the American Benefits Council (which represents employers), the American Federation of Teachers (AFT), First Focus (a bipartisan children’s advocacy organization), and the Pacific Business Group on Health
People Want to Flourish, Not Just Live – Speaking Health Politics to Real People
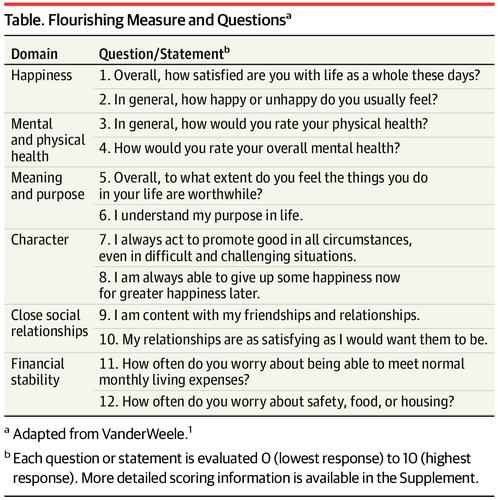
“How should we define ‘health?'” a 2011 BMJ article asked. The context for the question was that the 1948 World Health Organization definition of health — that health is, “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”– was not so useful in the 21st century. The authors, a global, multidisciplinary team from Europe, Canada and the U.S., asserted that by 2011, human health was marked less by infectious disease and more by non-communicable conditions that could be highly influenced, reversed and prevented through self-care by the individual and public health policy
How Consumers’ Belt-Tightening Could Impact Health/Care – Insights from Deloitte’s Retail Team

Over the ten years between 2007 and 2017, U.S. consumer spending for education, food and health care substantially grew, crowding out spending for other categories like transportation and housing. Furthermore, income disparity between wealthy Americans and people earning lower-incomes dramatically widened: between 2007-2017, income for high-income earners grew 1,305 percent more than lower-incomes. These two statistics set the kitchen table for spending in and beyond 2019, particularly for younger people living in America, considered in Deloitte’s report, The consumer is changing, but perhaps not how you think. The authors are part of Deloitte Consulting’s Retail team. The retail spending data
Health Care Costs Still Americans’ Top Financial Worry Among All Money Concerns

Health care costs rank ahead of Americans’ money-worries about low wages and availability of cash, paying for college, house payments, taxes, and debt, according to the latest Gallup poll on peoples’ most important family financial problems in 2019. Medical costs have, in fact, ranked at the top of this list for three years in a row, with a five percentage point rise between 2018 and 2019. No other financial concern had that growth in increase-of-money-worries in the past year. Health care costs rank the top financial problem for people across all income levels. One in five families (19%) earning under
How Consumers Look At Social Determinants of Health for Cancer, Diabetes and Mental Health

Enlightened health/care industry and public policy stakeholders have begun to embrace and address social determinants of health. These are the inputs that bolster health beyond health care services: they include economic stability like job security and income level (and equity), education, and access to healthy food, food security, safe neighborhoods, social support, clean environments (water and air), and in my own update on SDoH factors, access to broadband connectivity. As physician leaders in the AMA, technology advocates from AMIA, and numerous health plans focus efforts on strengthening social determinants, what do people – consumers, patients, caregivers — think about these
The 3 A’s That Millennials Want From Healthcare: Affordability, Accessibility, Availability

With lower expectations of and satisfaction with health care, Millennials in America seek three things: available, accessible, and affordable services, research from the Transamerica Center for Health Studies has found. Far and away the top reason for not obtaining health insurance in 2018 was that it was simply too expensive, cited by 60% of Millennials. Following that, 26% of Millennials noted that paying the tax penalty plus personal medical expenses were, together, less expensive than available health options. While Millennials were least likely to visit a doctor’s office in the past year, they had the most likelihood of making a
A Dose of Optimism Is a Prescription for Financial Health, Says Frost Bank

People define their personal health and well-being broadly, well beyond physical health. Mental wellness, physical appearance, social connections, and financial wellness all add into our self-health definitions. Mind Over Money is a consumer study conducted by Frost Bank, working with FleischmanHillard, connecting the dots between optimism and financial health. The top-line of the study is that people who are optimists have roughly two-thirds fewer days of financial stress per year than pessimists. Put another way, pessimists stress about finances 62% of the year, shown in the first chart from the study. This translates into 62% of optimists having better financial
Listen Up, Healthcare: Hear The Patient’s Voice!
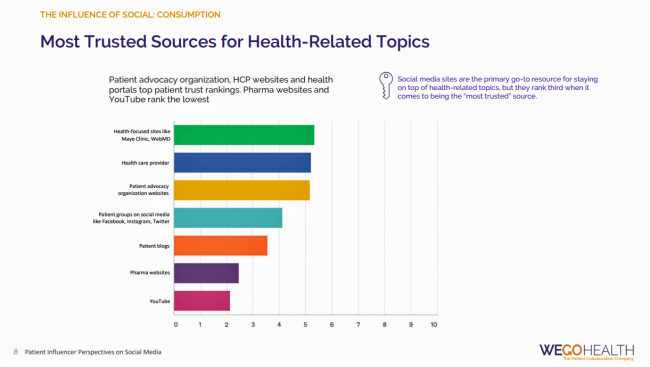
Consider the voice of a patient before the advent of the Internet in the digital 1.0 world, and then the proliferation of social networks in v 2.0. One patient could talk with another over their proverbial neighborhood fence, a concerned parent at the PTA meeting with others dealing with a children’s health issue, or a recovering alcoholic testifying in person at an AA session. Today, the voice of the patient is magnified one-to-many, omnichannel and multi-platform — via video, blogs, podcasts, social networks, listservs….and, yes, still in live forums like AA meetings, church basements, Y-spaces, and the Frazzled Cafe meet-ups
The United States of Diabetes: a $1,240 Tax on Every American
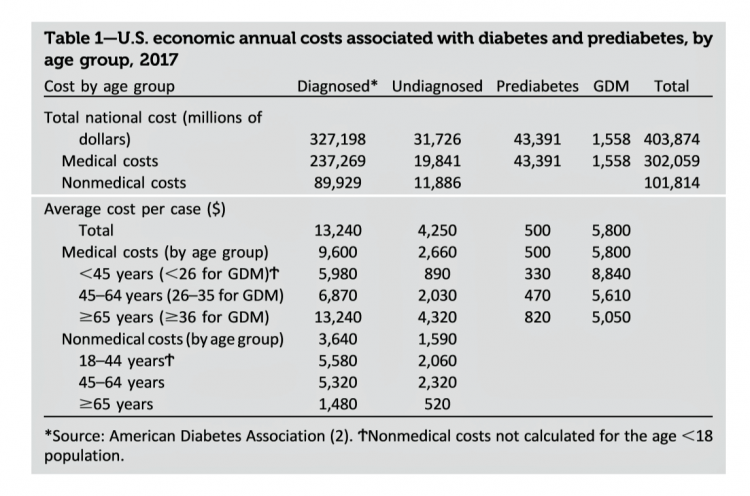
Pharmaceutical company executives are testifying in the U.S. Congress this week on the topic of prescription drug costs. One of those medicines, insulin, cost a patient $5,705 for a year’s supply in 2016, double what it cost in 2012, according to the Health Care Cost Institute. Know that one of these insulin products, Lilly’s Humalog, came onto the market in 1996. In typical markets, as products mature and get mass adoption, prices fall. Not so insulin, one of the many cost components in caring for diabetes. But then prescription drug pricing doesn’t conform with how typical markets work in theory.
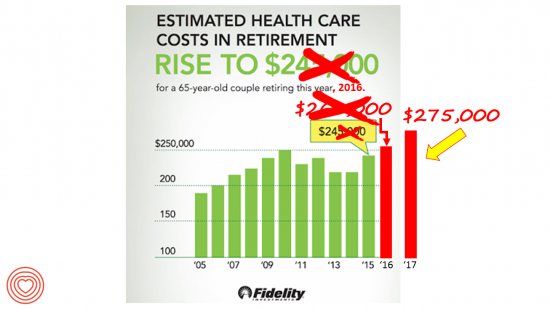
What $285,000 Can Buy You in America: Medical Costs for Retirees in 2019
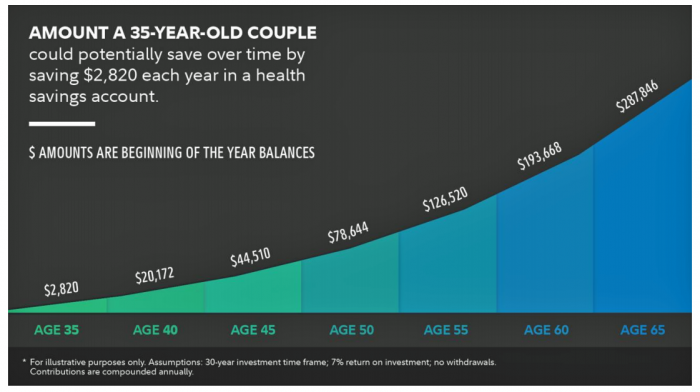
The average 65-year old couple retiring in 2019 will need to have a cash nest-egg of $285,000 to cover health care and medical expenses through retirement years, Fidelity Investments calculated. Fidelity estimates the average retiree will allocate 15% of their annual spending in retirement on medical costs. As if that top-line number isn’t enough to sober one up, there are two more caveats: (1) the $285K figure doesn’t include long-term care, dental services and over-the-counter medicines; and, (2) it’s an after-tax number. So depending on your tax bracket, you have to earn a whole lot more to net the $285,000
Medical Costs Are Consuming Americans’ Financial Health
Spending on medical care costs crowded out other household spending for millions of Americans in 2018, based on The U.S. Healthcare Cost Crisis, a survey from West Health and Gallup. Gallup polled 3,537 U.S. adults 18 and over in January and February 2019. One in three Americans overall are concerned they won’t be able to pay for health care services or prescription drugs: that includes 35% of people who are insured, and 63% of those who do not have insurance. Americans borrowed $88 billion in 2018 to pay for health care spending, West Health and Gallup estimated. 27 million Americans
In the Modern Workplace, Workers Favor More Money, New Kinds of Benefits, and Purpose
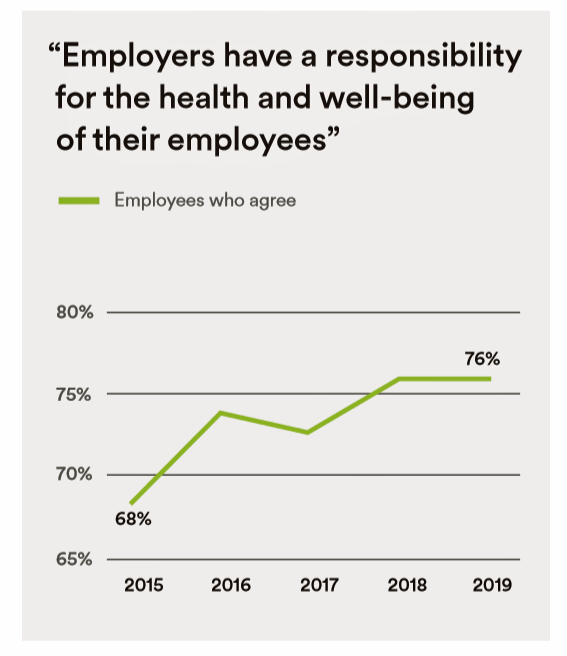
Today, April 2nd, is National Employee Benefits Day. Who knew? To mark the occasion, I’m mining an important new report from MetLife, Thriving in the New Work-Life World, the company’s 17th annual U.S. employee benefit trends study with new data for 2019. For the research, MetLife interviewed 2,500 benefits decision makers and influencers of companies with at least two employees. 20% of the firms employed over 10,000 workers; 20%, 50 and fewer staff. Companies polled represented a broad range of industries: 11% in health care and social assistance, 10% in education, 9% manufacturing, 8% each retail and information technology, 7%
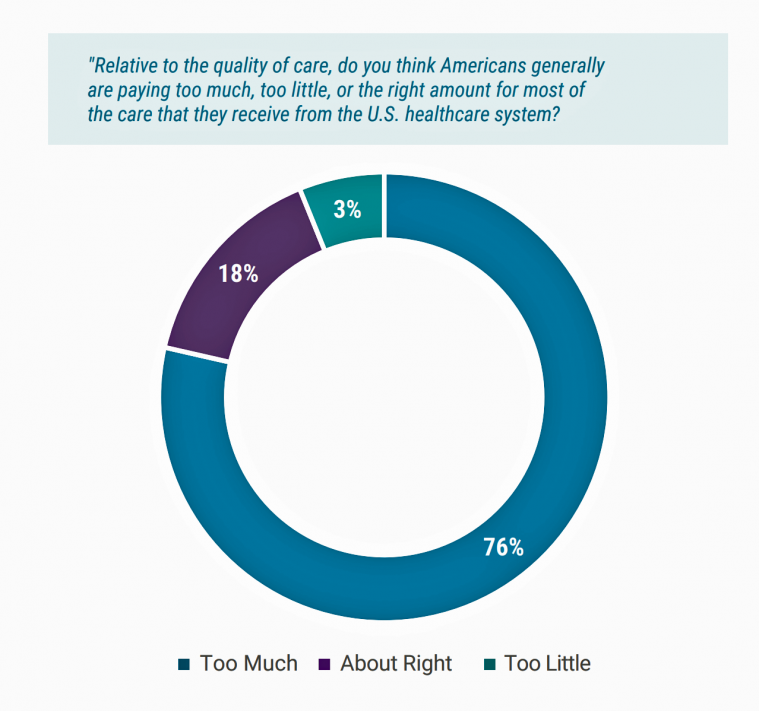
In the U.S., Patients Consider Costs and Insurance Essential to Their Overall Health Experience
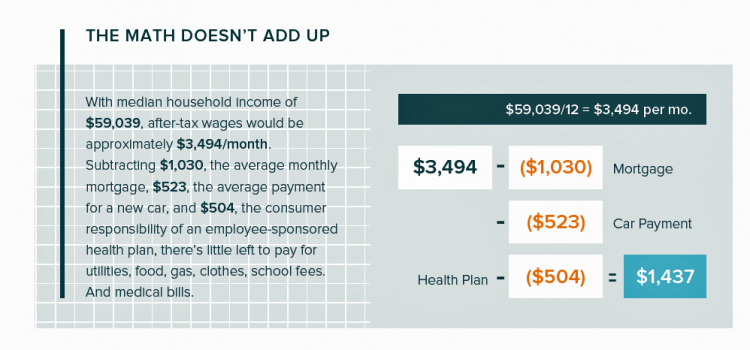
Patients in the U.S. assume the role of payor when they are enrolled in high-deductible health plans. People are also the payor when dealing with paying greater co-payments for prescription drugs, especially as new therapeutic innovations come out of pipelines into commercial markets bearing six-digit prices for oncology and other categories. For mainstream Americans, “the math doesn’t add up” for paying medical bills out of median household budgets, based on the calculations in the 2019 VisitPay Report. Given a $60K median U.S. income and average monthly mortgage and auto payments, there’s not much consumer margin to cover food, utilities, petrol,
Medical Issues Are Still The #1 Contributor to Bankruptcy in the U.S., An AJPH Study Asserts
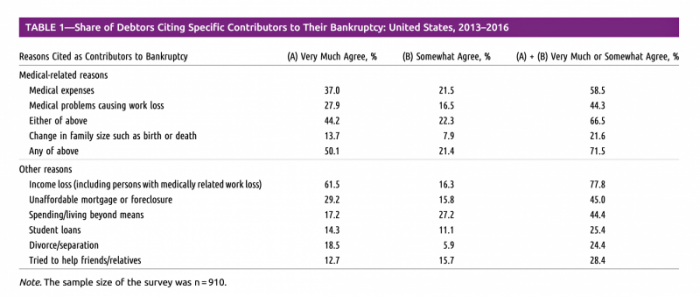
Medical costs in America are still the top contributor to personal bankruptcy in the U.S., a risk factor in two-thirds of bankruptcies filed between 2013 and 2016. That’s a sad fiscal fact, especially as more Americans gained access to health insurance under the Affordable Care Act, according to a study published this month in the American Journal of Public Health (AJPA). Between 2013 and 2016, about 530,000 bankruptcies were filed among U.S. families each year associated with medical reasons, illustrated in Table 1 from the study. The report, Medical Bankruptcy: Still Common Despite the Affordable Care Act, updates research from 2007 which
Most Americans Across Party ID Favor U.S. Government Negotiation to Lower Rx Drug Costs

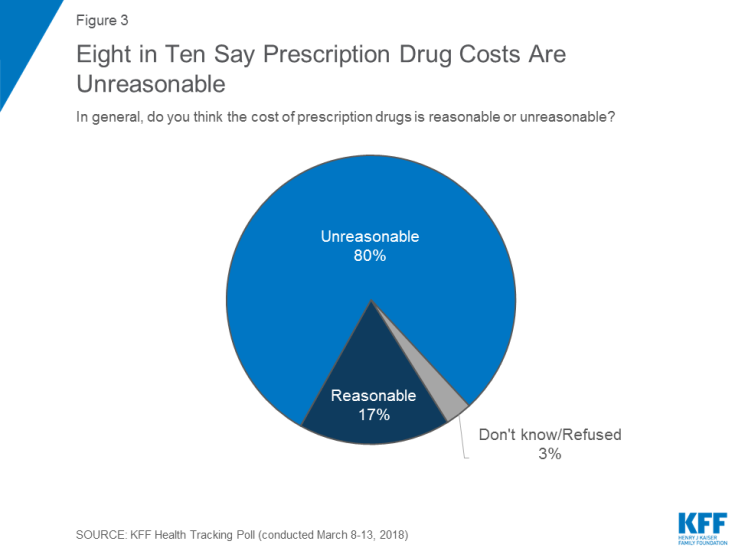
There’s little Americans, by political party, agree upon in 2019. One of the only issues bringing people together in the U.S. is prescription drug prices — that they’re too high, that the Federal government should negotiate to lower costs for Medicare enrollees, and that out-of-pocket costs for drugs should be limited. The Kaiser Family Foundation has been tracking this topic for a few years, and this month, their March 2019 Health Tracking Poll shows vast majorities of Democrats, Independents and Republicans all share these sentiments. It’s not that patients who take prescription drugs don’t appreciate them – most (58%) say medicines
Open Table for Health: Patients Are Online For Health Search and Physician Reviews
Seeking health information online along with researching other patients’ perspectives on doctors are now as common as booking dinner reservations and reading restaurant reviews, based on Rock Health’s latest health consumer survey, Beyond Wellness for the Healthy: Digital Health Consumer Adoption 2018. Rock Health has gauged consumes’ digital health adoption fo a few years, showing year-on-year growth for “Googling” health information, seeking peer patients’ physician and hospital reviews, tracking activity, donning wearable tech, and engaging in live telehealth consultations with providers, as the first chart shows. The growth of tracking and wearable tech is moving toward more medical applications beyond fitness
The Cost of Prescription Drugs, Doctors and Patient Access – A View from HIMSS19
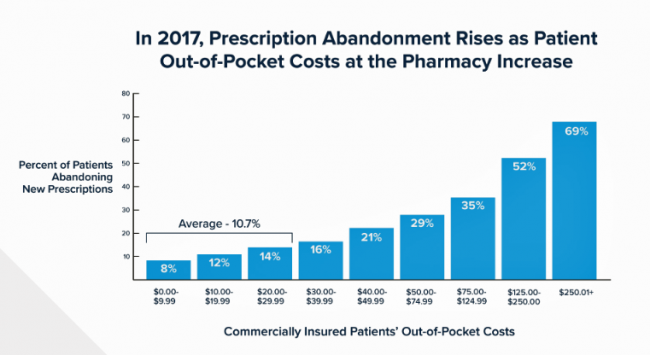
Most patient visits to doctors result in a prescription written for a medicine that people retrieve from a pharmacy, whether retail in the local community or via mail order for a maintenance drug. This one transaction generates a lot of data points, which individually have a lot of importance for the individual patient. Mashed with other patients’, prescription drug utilization data can combine with more data to be used for population health, cost-effectiveness, and other constructive research pursuits. At HIMSS19, there’s an entire day devoted to a Pharma Forum on Tuesday 12 February, focusing on pharma-provider-payor collaborations. Allocating a full
Calling Out Health Equity on Martin Luther King Day 2019
On this weekend as we appreciate the legacy of Martin Luther King, Jr., I post a photo of him in my hometown of Detroit in 1963, giving a preliminary version of the “I Have a Dream” speech he would deliver two months later in Washington, DC. Wisdom from the speech: “But now more than ever before, America is forced to grapple with this problem, for the shape of the world today does not afford us the luxury of an anemic democracy. The price that this nation must pay for the continued oppression and exploitation of the Negro or any other
In U.S. Health Care, It’s Still the Prices, Stupid – But Transparency and Consumer Behavior Aren’t Working As Planned
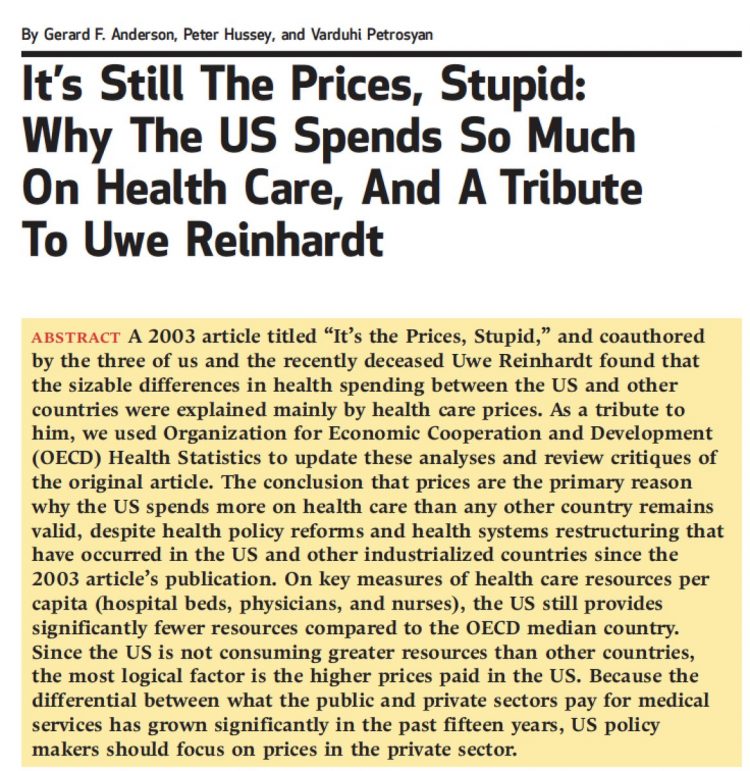
I’m glad to be getting back to health economic issues after spending the last couple of weeks firmly focused on consumers, digital health technologies and CES 2019. There’s a lot for me to address concerning health care costs based on news and research published over the past couple of weeks. We’ll start with the centerpiece that will provide the overall context for this post: that’s the ongoing research of Gerard Anderson and colleagues under the title, It’s Still The Prices, Stupid: Why The US Spends So Much On Health Care, And A Tribute To Uwe Reinhardt. It is bittersweet to
The Consumer as Payor – Retail Health at CES 2019

All health/care is retail now in America. I say this as most people in the U.S. who have health insurance must take on a deductible of some amount, which compels that insured individual to spend the first dollar on medical services up until they meet their financial commitment. At that point, health insurance kicks in, and then the insured may have to spend additional funds on co-payments for general medicines and services, and coinsurance for specialty drugs like injectables and high-cost new therapies. The patient is a consumer is a payor, I asserted today during my talk on the expanding
Costs, Consumerism, Cyber and Care, Everywhere – The 2019 Health Populi TrendCast

Today is Boxing Day and St. Stephens Day for people who celebrate Christmas, so I share this post as a holiday gift with well-wishes for you and those you love. The tea leaves have been brewing here at THINK-Health as we prepared our 2019 forecast at the convergence of consumers, health, and technology. Here’s our trend-weaving of 4 C’s for 2019: costs, consumerism, cyber and care, everywhere… Health care costs will continue to be a mainstream pocketbook issue for patients and caregivers, with consequences for payors, suppliers and ultimately, policymakers. Legislators inside the DC Beltway will be challenged by the
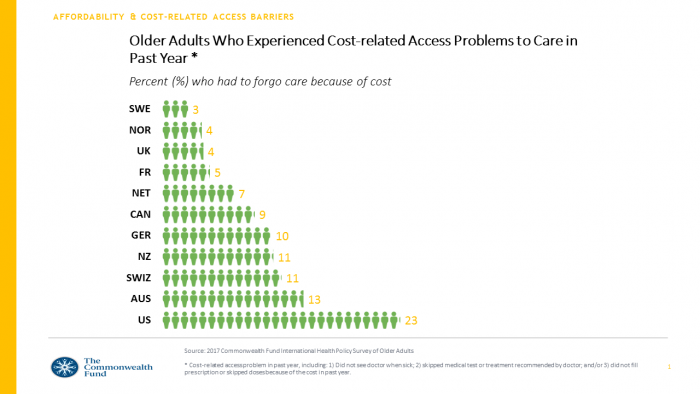
Rationing Care in America: Cost Implications Getting to Universal Health Coverage

It would not be surprising to know that when the Great Recession hit the U.S. in 2008, one in three Americans delayed medical treatment due to costs. Ten years later, as media headlines and the President boast an improved American economy, the same proportion of people are self-rationing healthcare due to cost. That percentage of people who delay medical cost based on the expense has remained stable since 2006: between 29 and 31 percent of Americans have self-rationed care due to cost for over a decade. And, 19% of U.S. adults, roughly one-in-five people who are sick and dealing with
Americans End 2018 Worried About Healthcare Costs

Nearly one-half of Americans are quite concerned they won’t have enough money to pay for medical care, according to the latest Gallup poll. Health insurance in-security is mainstream as of November 2018, when Gallup polled U.S. adults about views on healthcare costs. It’s a major concern among six in ten people that their health plan would require they pay higher premiums or a bigger portion of their healthcare expenses. It’s also a big concern for four in ten people that someone in their family would be denied health insurance covering for a pre-existing condition, or that they might have to
While National Health Care Spending Growth Slowed in 2017, One Stakeholder’s Financial Burden Grew: The Consumer’s

National health care spending growth slowed in 2017 to the post-recession rate of 3.9%, down from 4.8% in 2016. Per person, spending on health care grew 3.2% to $10,739 in 2017, and the share of GDP spent on medical care held steady at 17.9%. Healthcare spending in America is a $3.5 trillion micro-economy…roughly the size of the entire GDP of Germany, and about $1 trillion greater than the entire economy of France. These annual numbers come out of the annual report from the Centers for Medicare and Medicaid Services, published yesterday in Health Affairs. Underneath these macro-health economic numbers is
Most Americans Want the Federal Government to Ensure Healthcare for All

Most people in the U.S. believe that the Federal government should ensure that their fellow Americans, a new Gallup Poll found. This sentiment has been relatively stable since 2000 except for two big outlying years: a spike of 69% in 2006, and a low-point in 2003 of 42%. In 2006, Medicare Part D launched, which may have boosted consumers’ faith in Federal healthcare programs. In contrast, in 2013 the Affordable Care Act was in implementation and consumer-adoption mode, accompanied by aggressive anti-“Obamacare” campaigns in mass media. That’s the top lighter green line in the first chart. But while there’s majority support
Money First, Then Kids: The State of the American Family in 2018

Most American families with children at home are concerned about paying bills on a monthly basis. One in two people have had at least one personal “economic crisis” in the past year, we learn in the American Family Survey 2018, released last week from Deseret News and The Brookings Institution. The project surveyed 3,000 U.S. adults across the general population, fielded online by YouGov. This poll, conducted since 2005, looks at the state of U.S. families through several issue lenses: the state of marriage and family, parents and teenagers, sexual harassment (with 2018 birthing the #MeToo movement), social capital and
The Ultimate Health Outcome, Mortality, Is Rising in America

How long can people living in the U.S. expect to live? 78.6 years of age, if you were born in 2017. That’s a decline of 0.1 year from 2016. This decline especially impacted baby boys: their life expectancy fell to 76.1 years, while baby girls’ life expectancy stayed even at 81.1 years. That’s the latest data on Mortality in the United States, 2017, soberly brought to you by the Centers for Disease Control and Prevention, part of the U.S. Department of Health and Human Services. Underneath these stark numbers are the specific causes of death: in 2017, more Americans died
Consumers Want Help With Health: Can Healthcare Providers Supply That Demand?

Among people who have health insurance, managing the costs of their medical care doesn’t rank as a top frustration. Instead, attending to health and wellbeing, staying true to an exercise regime, maintaining good nutrition, and managing stress top U.S. consumers’ frustrations — above managing the costs of care not covered by insurance. And maintaining good mental health and staying on-track with health goals come close to managing uncovered costs, Oliver Wyman’s 2018 consumer survey learned. These and other important health consumer insights are revealed in the firm’s latest report, Waiting for Consumers – The Oliver Wyman 2018 Consumer Survey of US
Financial Stress Is An Epidemic In America, Everyday Health Finds

One in three working-age people in the U.S. have seen a doctor about something stress-related. Stress is a way of American life, based on the findings in The United States of Stress, a survey from Everyday Health. Everyday Health polled 6,700 U.S. adults between 18 and 64 years of age about their perspectives on stress, anxiety, panic, and mental and behavioral health. Among all sources of stress, personal finances rank as the top stressor in the U.S. Over one-half of consumers say financial issues regularly stress them out. Finances, followed by jobs and work issues, worries about the future, and relationships cause
Food and Cooking for Health: a UK Perspective from Hammersmith & Fulham
Food deserts aren’t just a U.S. phenomenon. They’re found all around the world. This week as I explore social determinants of health and technology solutions in several parts of Europe, I’ve learned more about food access challenges in the UK. These are discussed in a report published this month by the Social Market Foundation asking, What are the barriers to eating healthily in the UK? The research was supported by Kellogg’s, the food manufacturer. The first table comes from the report, and the topline shows that about 4 in 10 Britons shopped at a cheaper food store in response to high
Loneliness, Public Policy and AI – Lessons From the UK For the US

There’s a shortage of medical providers in the United Kingdom, a nation where healthcare is guaranteed to all Britons via the most beloved institution in the nation: The National Health Service. The NHS celebrated its 70th anniversary in July this year. The NHS “supply shortage” is a result of financial cuts to both social care and public health. These have negatively impacted older people and care for people at home in Great Britain. This article in the BMJ published earlier this year called for increasing these investments to ensure further erosion of population and public health outcomes, and to prevent
Open Source Health Care Will Liberate Patients

Information is power in the hands of people. When it’s open in the sunshine, it empowers people — whether doctors, patients, researchers, Presidents, teachers, students, Everyday People. Welcome to the era of Open Source Healthcare, not only the “about time” for patients to own their health, but for the launch of a new publication that will support and continue to evolve the concept. It’s really a movement that’s already in process. Let’s go back to some definitions and healthcare basics to understand just why Open Source Healthcare is already a thing. When information access is uneven, it’s considered
As Workers’ Healthcare Costs Increase, Employers Look to Telehealth and Wearable Tech to Manage Cost & Health Risks
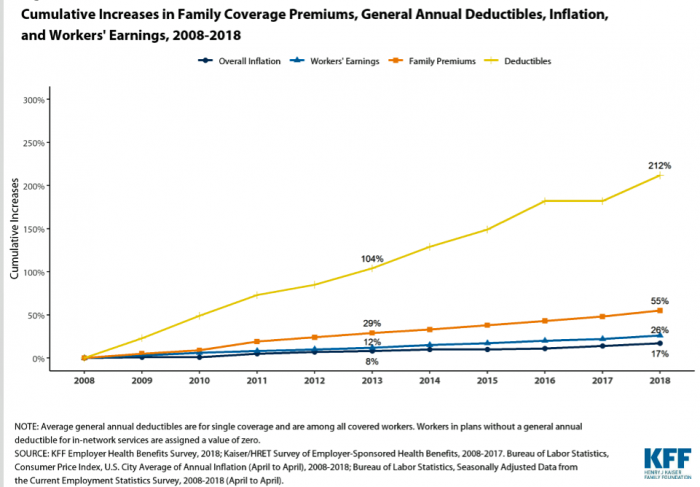
Family premiums for health insurance received at the workplace grew 5% in 2018: to $19,616, according to the 2018 KFF Employer Health Benefits Survey released today by the Kaiser Family Foundation (KFF). These two trends combine for a 212% increase in workers’ deductibles in the past decade. This is about eight times the growth of workers’ wages in the U.S. in the same period. Thus, the main takeaway from the study, KFF President and CEO Drew Altman noted, is that rising health care costs absolutely remain a burden for employers — but a bigger problem for workers in America. Given that
When Life and Health Insurance Blur: John Hancock, Behavioral Economics, and Wearable Tech

Most consumers look to every industry sector to help them engage with their health. And those companies include the insurance industry and financial services firms, we found in the 2010 Edelman Health Engagement Barometer. John Hancock, which covers about 10 million consumers across a range of products, is changing their business model for life insurance. Here’s the press release, titled, “John Hancock Leaves Traditional Life Insurance Model Behind to Incentivize Longer, Healthier Lives.” “We fundamentally believe life insurers should care about how long and well their customers live. With this decision, we are proud to become the only U.S. life insurance
Consumers Don’t Know What They Don’t Know About Healthcare Costs

The saving rate in the U.S. ranks among the lowest in the world, in a country that rates among the richest nations. So imagine how well Americans save for healthcare? “Consumers are not disciplined about saving in general,” with saving for healthcare lagging behind other types of savings, Alegeus observes in the 2018 Alegeus Consumer Health & Financial Fluency Report. Alegeus surveyed 1,400 U.S. healthcare consumers in September 2017 to gauge peoples’ views on healthcare finances, insurance, and levels of fluency. As patients continue to take on more financial responsibility for healthcare spending in the U.S., they are struggling with finances and
Self-Care is Healthcare for Everyday People

Patients are the new healthcare payors, and as such, taking on the role of health consumers. In fact, health and wellness consumers have existed since a person purchased the first toothpaste, aspirin, heating pad, and moisturizing cream at retail. Or consulted with their neighborhood herbalista, homeopathic practitioner, therapeutic masseuse, or skin aesthetician. Today, the health and wellness consumer can DIY all of these things at home through a huge array of products available in pharmacies, supermarkets, Big Box stores, cosmetic superstores, convenience and dollar stores, and other retail channels – increasingly, online (THINK, of course, of Amazon — more on
The Top Pain Point in the Healthcare Consumer Experience is Money

Beyond the physical and emotional pain that people experience when they become a patient, in the U.S. that person becomes a consumer bearing expenses and financial pain, as well. 98% of Americans rank paying their medical bills is an important pain point in their patient journey, according to Embracing consumerism: Driving customer engagement in the healthcare financial journey, from Experian Health. Experian is best known as the consumer credit reporting agency; Experian Health works with healthcare providers on revenue cycle management, patient identity, and care management, so the company has experience with patient finance and medical expense sticker shock. In the
Surprise, Surprise: Most Americans Have Faced a “Surprise” Medical Bill

Most Americans have been surprised by a medical bill, a NORC AmeriSpeak survey found. Who’s responsible? Nearly all Americans (86% net responsible) first blame health insurance companies, followed by hospitals (82%). Fewer U.S. patients blamed doctors and pharmacies, although a majority of consumers still put responsibility for surprise healthcare bills on them (71% and 64% net). Most of the surprise bills were for charges associated with a physician’s service or lab test. Most surprise charges were not due to the service being excluded from a health plans provider network. The poll was conducted among 1,002 U.S. adults 18 and over
Wealth is Health and Health, Wealth, Fidelity Knows – with Weight a Major Risk Factor
The two top stressors in American life are jobs and finances. “My weight” and my family’s health follow just behind these across the generations. Total Well-Being, a research report from Fidelity Investments, looks at the inter-connections between health and wealth – the combined impact of physical, mental, and fiscal factors on our lives. The first chart summarizes the study’s findings, including the facts that: One-third of people have less than three months of income in the bank for emergency Absenteeism is 29% greater for people who don’t have sufficient emergency funds saved People who are highly stressed tend not to
Benefit Cost Increases Overwhelm Flat Wages for Most in US: Pew
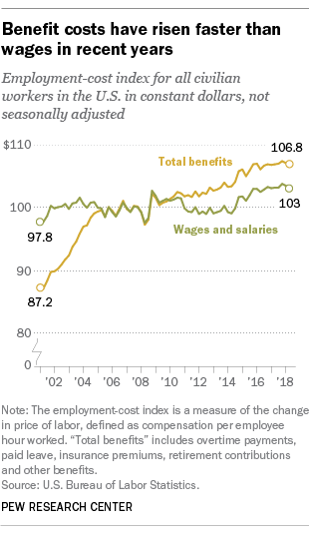
Today’s financial news reports and the bullish stock market generate headlines saying that the U.S. economy is riding high. President Trump forecasted in late July, “we are now on track to hit an average GDP annual growth of over 3% and it could be substantially over 3%,” Trump said. “Each point, by the way, means approximately $3 trillion and 10 million jobs. Think of that.” Indeed, unemployment is at its lowest rate in decades at 4%. Today, NASDAQ reported that, “the U.S. economy stays strong as the Fed holds steady.” For mainstream working people, though, even with a job in a high employment
Employers Take on Health Activism, Embracing Behavioral Health, Virtual Care, AI, and Transparency
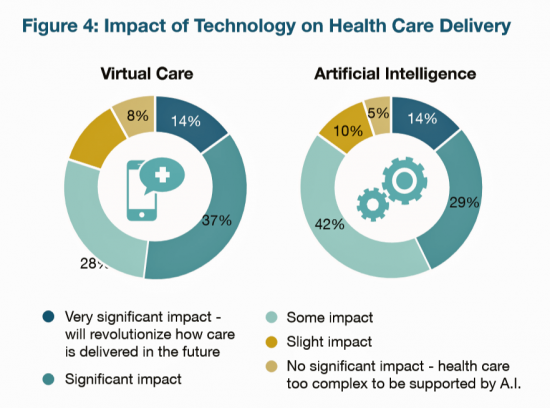
More U.S. employers are growing activist roles as stakeholders in the healthcare system, according to the 2019 Large Employers Health Care Strategy and Plan Design Survey from the National Business Group on Health (NBGH). Consider the Amazon-Berkshire Hathaway-JPMorgan Chase link up between Jeff Bezos, Warren Buffet, and Jamie Dimon, as the symbol of such employer-health activism. The NBGH report is based on survey results collected from 170 large employers representing 13 million workers and 19 million covered lives (families/dependents). This annual survey is one of the most influential such reports released each year, providing a current snapshot of large employers’ views
How Taking Care of Your Health Boosts Savings Accounts
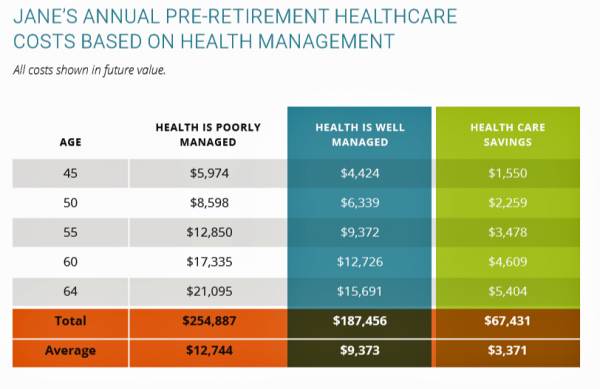
It will cost about $275,000 for a couple retiring in the U.S. this year to cover their healthcare costs for the rest of their life in retirement, Fidelity estimated. But Americans are notoriously pretty undisciplined about saving money, compared with peers living in other developed countries. How to address this challenge? Show people what improving their personal health can do to boost their 401(k) plans. This tactic is discussed in Health & Retirement Savings: Leveraging Healthcare Costs to Drive 401(k) Contributions & Improve Health, from HealthyCapital, a joint venture of Mercy health systems and HealthView Services. The chart illustrates three
Consumers Consider Cost When They Think About Medical Innovation
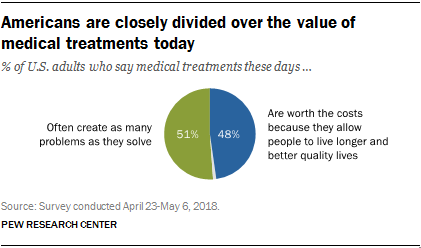
While the vast majority of Americans say that science has made life easier for most people, and especially for health care, people are split in questioning the financial cost and value of medical treatments, the Pew Research Center has found. The first chart illustrates the percent of Americans identifying various aspects of medical treatments as “big problems.” If you add in people who see these as “small problems,” 9 in 10 Americans say that all of these line items are “problems.” In the sample, two-thirds of respondents had seen a health care provider for an illness or medical condition in
Healthcare Policies We Can Agree On: Pre-Existing Conditions, Drug Prices, and PillPack – the June 2018 KFF Health Tracking Poll
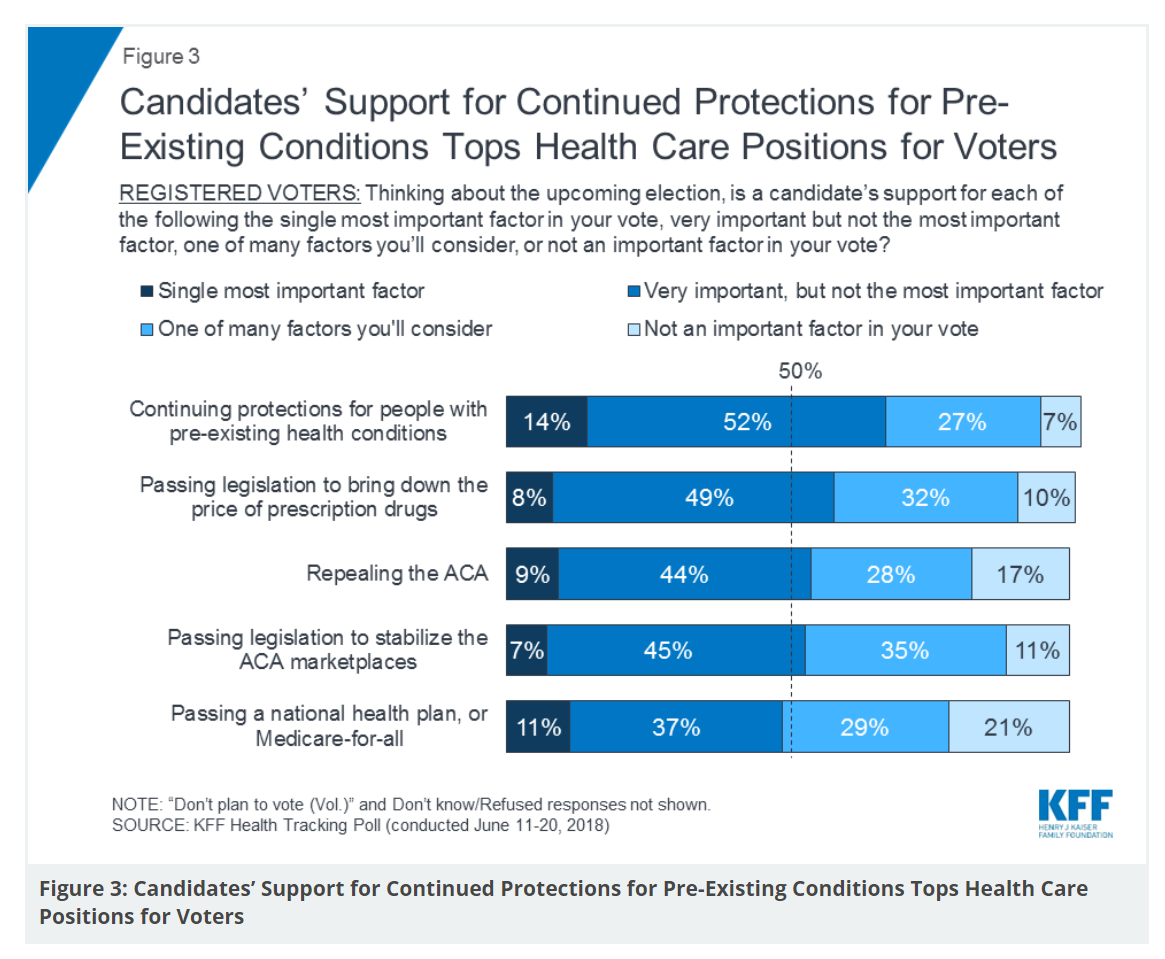
There are countless chasms in the U.S. this moment in social, political, and economic perspectives. but one issue is on the mind of most American voters where there is evidence of some agreements: health care, as evidenced in the June 2018 Health Tracking Poll from Kaiser Family Foundation. Top-line, health care is one of the most important issues that voters want addressed in the 2018 mid-term elections, tied with the economy. Immigration, gun policy, and foreign policy follow. While health care is most important to voters registered as Democrats, Republicans rank it very important. Among various specific health care factors, protecting
Design, Empathy and Ethics Come to Healthcare: HXD

Design-thinking has come to health/care, finally, and Amy Cueva has been beating this drum for a very long time. I’m delighted to be in her collegial circle, speaking at the conference about the evolving healthcare consumer who’s financially strapped, stressed-out, and Amazon Primed for customer service. I’m blogging live while attending HXD 2018 in Cambridge, MA, the health/care design conference convened by Mad*Pow, 26th and 27th June 2018. Today was Day 1 and I want to recap my learnings and share with you. Amy, Founder and Chief Experience Office of Mad*Pow, kicked off the conference with context-setting and inspiration. Design
Good Coffee + Engaging Design + Banking = Financial Health

As I walked by windows with Marvel-inspired superhero characters, I stopped to read their talk-bubbles: “strengthen your savings, power your financial quest, be the hero of your money, be one with your budget.” The top-line message here is that you can be your own fiscal superhero. The sign read, Capital One Cafe with Peet’s Coffee. But was it a bank branch or a cafe? I asked myself, passing by this sign yesterday morning at the corner of Walnut and 18th Streets in center city Philadelphia. It’s both, as it turned out, and when I entered I found a welcoming, beautifully
It Could Take Five Generations for a Low-Income US Family to Reach Average Income in America

Social mobility in America has a lot of friction: children of wealthier people tend to grow into affluence, and children of low-income parents tend to struggle to move up the income and education ladder, according to A Broken Social Elevator: How to Promote Social Mobility, a new report from the OECD. The Organization for Economic Cooperation and Development studied member nations’ economies, demographics, income and opportunities to gauge each country’s social mobility. Social mobility, the OECD explains, is multi-faceted. It can refer to inter-generational mobility between parents, children, and grandchildren. Alternatively, social mobility can look at intra-generational mobility, over the course
As Medical Cost Trend Remains Flat, Patients Face Growing Health Consumer Financial Stress

When it comes to healthcare costs, lines that decline over time are generally seen as good news. That’s how media outlets will cover the top-line of PwC’s report Medical cost trend: Behind the numbers 2019. However, there are other forces underneath the stable-looking 6.0% medical trend growth projected for 2019 that will impact healthcare providers, insurers, and suppliers to the industry. There’s this macro-health economic story, and then there’s the micro-economics of healthcare for the household. Simply put: the impact of growing financial risk for healthcare costs will be felt by patients/consumers themselves. I’ve curated the four charts from the
Doing Less Can Be Doing More for Healthcare – the Biggest Takeaway From ASCO 2018

Less can lead to more for so many things: eating smaller portions, lowering sugar consumption, and driving less in favor of walking or cycling come to mind. When it comes to healthcare utilization, doing less can also result in equal or even better outcomes. Groundbreaking research presented at this week’s ASCO meeting found that some women diagnosed with certain forms of cancer do not benefit from undergoing chemotherapy. The American Society of Clinical Oncology (ASCO) is one of the largest medical meetings annually, and at this huge meeting these research results for the TAILORx trial were huge news with big
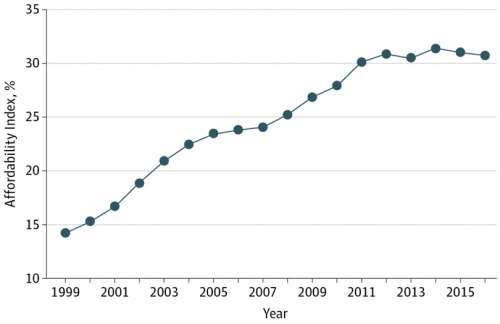
Mary Meeker on Healthcare in 2018: Connectivity, Consumerization, and Costs
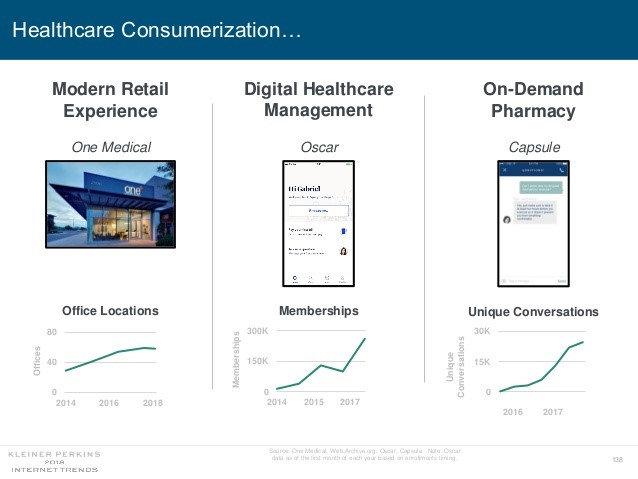
Health care features prominently in the nearly-300 slides curated by Mary Meeker in her always- informative report on Internet Trends 2018. Meeker, of Kleiner Perkins, released the report as usual at the Code Conference, held this year on 30 May 2018 in Silicon Valley. I’ve mined Meeker’s report for several years here on Health Populi: 2017 – Digital healthcare at the inflection point, via Mary Meeker 2015 – Musings with Mary Meeker on the digital/health nexus 2014 – Healthcare at an inflection point: digital trends via Mary Meeker 2013 – The role of internet technologies in reducing healthcare costs – Meeker
The US Covered Nearly 50% of Global Oncology Medicine Spending in 2017 – a market update from IQVIA
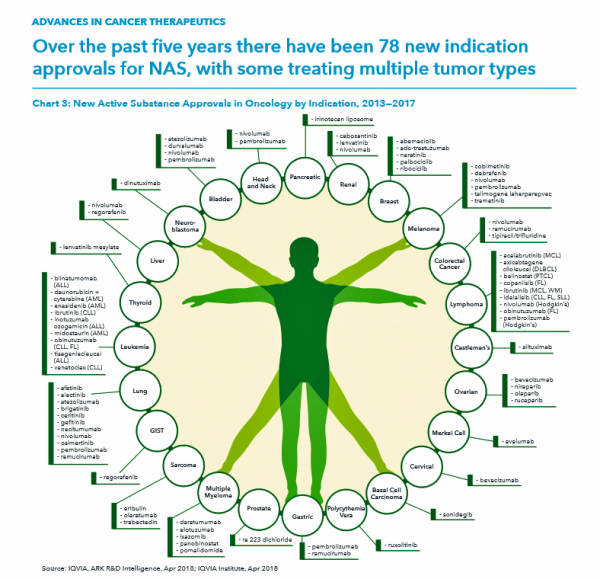
“We are at a remarkable point of cancer treatment,” noted Murray Aitken, Executive Director, IQVIA Institute for Human Data Science, in a call with media this week. 2017 was a banner year of innovative drug launches in oncology, Aitken coined, with more drugs used more extensively, driving improved patient for people dealing with cancer. This upbeat market description comes out of a report on Global Oncology Trends 2018 from the IQVIA Institute for Human Data Science. The subtitle of the report, “Innovation, Expansion and Disruption,” is appropriately put. The report covers these three themes across four sections: advances in therapies,
Health Care for a Typical Working Family of Four in America Will Cost $28,166 in 2018
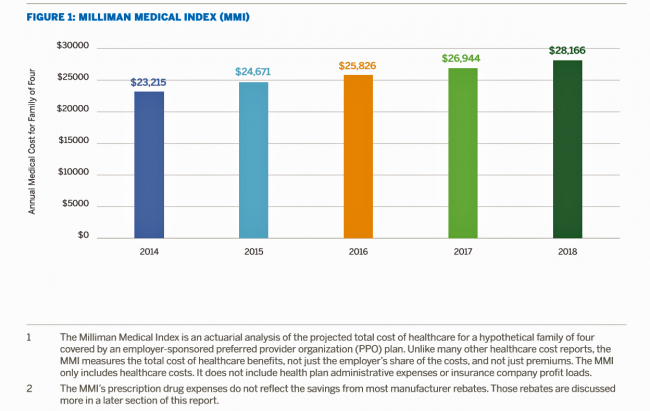
What could $28,166 buy you in 2018? A new car? A year of your child’s college education? A plot of land for your retirement home? Or a year of healthcare for a family of four? Welcome to this year’s edition of the Milliman Medical Index (MMI), one of the most important forecasts of the year in the world of the Health Populi blog and THINK-Health universe. That’s because we’re in the business of thinking about the future of health and health care through the health economics lens; the MMI is a key component of our ongoing environmental analysis of the
The U.S. is a Nation in Pain – America’s Life Expectancy Fell Again in 2016
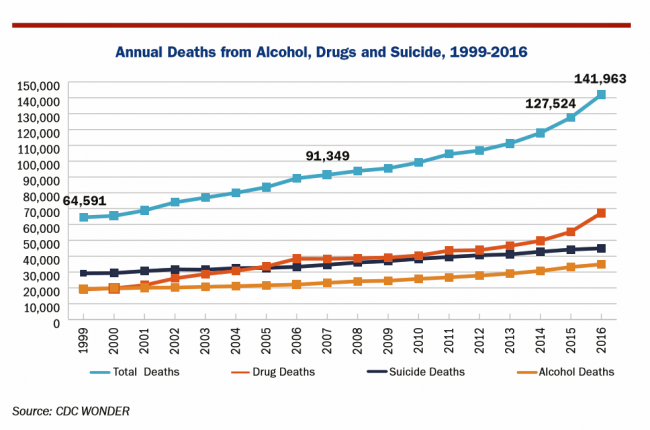
American saw the greatest number of deaths from suicide and alcohol- and drug-induced fatalities was recorded in 2016. That statistic of nearly 142,000 equates to deaths from stroke and exceed the number of deaths among Americans who died in all U.S. wars since 1950, according to Pain in the Nation Update from the Well Being Trust and Trust for America’s Health. The line graph soberly illustrates the growing tragic public health epidemic of mortality due to preventable causes, those deaths of despair as Anne Case and Sir Angus Deaton have observed in their research into this uniquely all-American phenomenon. While this
The Gap Between the Trump Administration’s Promise of Reducing Rx Costs for Consumers and What People Really Want
This is what happened to pharma stock prices on Friday after President Trump and Secretary of Health and Human Services Alex Azar outlined their new policies focusing on prescription drug prices. The graph is the Nasdaq U.S. Smart Pharmaceuticals Index (NQSSPH) from May 11, 2018, the date when POTUS and Secretary Azar made their announcement. What this upward driving curve indicates, from the start of stock trading in the morning until the ring of the closing bell, is that the pharma industry players, both manufacturers and PBMs, were quite delighted with what they heard. The blueprint for restructuring the prescription drug industry,
Having Health Insurance Is a Social Determinant of Health: the implications of growing uninsured in the U.S.
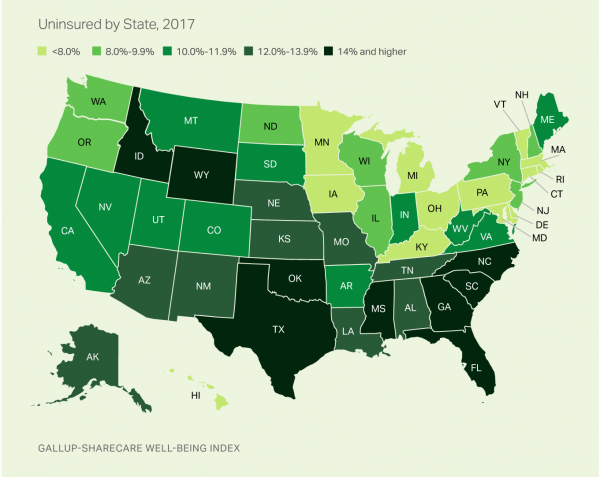
The rolls of the uninsured are growing in America, the latest Gallup-Sharecare Poll indicates. The U.S. uninsurance rate rose to 12.2% by the fourth quarter of 2017, up 1.3 percentage points from the year before. 2017 reversed advancements in health insurance coverage increases since the advent of the Affordable Care Act, and for the first time since 2014 no states’ uninsured rates fell. The 17 states with declines in insurance rates were Arizona, Colorado, Florida, Hawaii, Illinois, Indiana, Iowa, Missouri, New Mexico, New York, North Carolina, South Carolina, Texas, Utah, Washington, West Virginia, Wisconsin, and Wyoming. Among these, the greatest
Universal Health Care and Financial Inclusion – Two Sides of the Wellness Coin

Two weeks in a row, The Economist, the news magazine headquartered in London, included two special reports stapled into the middle of the magazines. Universal health care was covered in a section on 28 April 2018, and coverage on financial inclusion was bundled into the 5th May edition. While The Economist’s editors may not have intended for these two reports to reinforce each other, my lens on health and healthcare immediately, and appreciatively, connected the dots between healthcare coverage and financial wellness. The Economist, not known for left-leaning political tendencies whatsoever, lays its bias down on the cover of the section here: universal healthcare
How Walmart Could Bolster Healthcare in the Community

Walmart has been a health/care destination for many years. The company that defined Big Box stores in their infancy grew in healthcare, health and wellness over the past two decades, pioneering the $4 generic prescription back in 2006. Today, that low-cost generic Rx is ubiquitous in the retail pharmacy. A decade later, can Walmart re-imagine primary care the way the company did low-cost medicines? Walmart is enhancing about 500 of 3500 stores, and health will be part of the interior redecorating. Walmart has had ambitious plans in healthcare since those $4 Rx’s were introduced. Here’s a New York Times article from
What Would Healthcare Feel Like If It Acted Like Supermarkets – the 2018 Temkin Experience Ratings
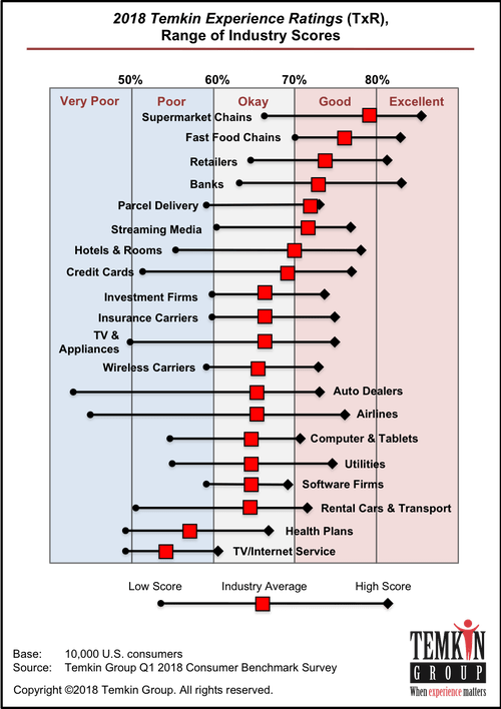
U.S. consumers rank supermarkets, fast food chains, retailers, and banks as their top performing industries for experience according to the 2018 Temkin Experience Ratings. Peoples’ experience with health plans rank at the bottom of the roster, on par with rental cars and TV/Internet service providers. If there is any good news for health plans in this year’s Temkin Experience Ratings compared to the 2017 results, it’s at the margin of “very poor” performance: last year, health plans has the worst performance of any industry (with the bar to the furthest point on the left as “low scoring”). This year, it
Sounds Like A John Denver Song: Virginia and Colorado Towns Rank High As Healthy Communities

If it’s true that “your ZIP code is more important than your genetic code,” you’d look for a job in 22046, buy a house there, and plant your roots. You’d find yourself in Falls Church, Virginia, named number one in the Healthiest Communities rankings of 500 U.S. towns. You can see a list of all of the communities here. The project is a collaboration between the Aetna Foundation and U.S. News & World Report, with help from the University of Missouri Center for Applied Research and Engagement Systems (CARES) and a team from the National Committee on Vital and Health
The New Financial Toxicity in Health Care: The Cost of Hospitalization
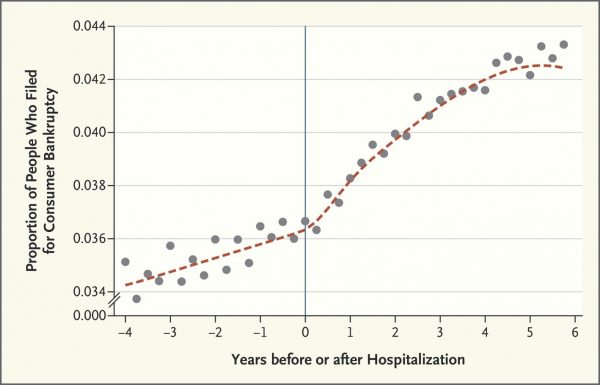
In healthcare, we use the word “toxicity” when it comes to taking a new medicine, especially a strong therapy to cure cancer. That prescription may be toxic as a harmful side effect on our journey to getting well. The concept of “financial toxicity” for cancer patients was raised by concerned clinicians at Sloane-Kettering Medical Center, who discussed the topic on 60 Minutes in 2014 and have published papers on the issue. Beyond strong medicines, a new financial toxicity has emerged for patients due to hospital inpatient admissions. A new article in the New England Journal of Medicine studies Myth and
Patient Privacy And Cyber In-Security at HIMSS 2018
Nearly one-half of Americans experienced a personal data breach in the past three years, the third annual national cybersecurity survey found. Ensuring privacy and cybersecurity should become integrated into the healthcare industry’s consideration of a patient’s consumer experience. This makes sense, given that privacy and cybersecurity ranked the second highest priority to hospitals and healthcare providers polled in HIMSS 2018 Healthcare Leadership Survey. Providers put patient safety as #1. Appropriately, privacy and security were hot topics at HIMSS Annual Conference this year, in respond to providers’ demands for more education and concerns around the challenges. Let’s put these concerns in
More Working Americans Enrolled in High-Deductible Health Plans in 2017
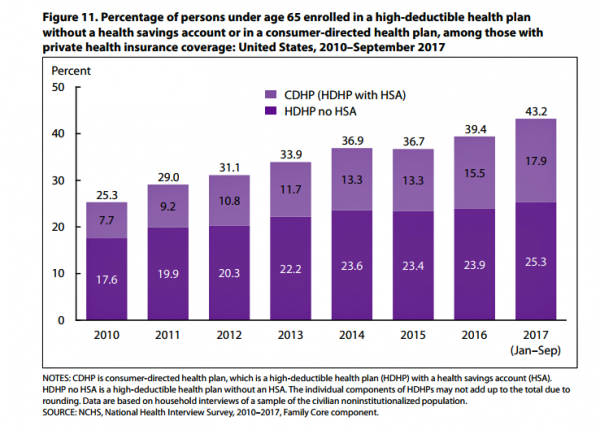
Over four in 10 U.S. workers were enrolled in a high-deductible health plan in the first 9 months of 2017, according to the latest research published by the National Center for Health Statistics, part of the Centers for Disease Control in the U.S. Department of Health and Human Services. The report details Health Insurance Coverage: Early Release of Estimates From the National Health Interview Survey, January-September 2017. About 28 million people were uninsured in the U.S. in 2017, about the same proportion as in 2016 — but nearly 20 million fewer than in 2010, as the line chart illustrates. The
Consumer Health and Patient Engagement – Are We There Yet?

Along with artificial intelligence, patient engagement feels like the new black in health care right now. Perhaps that’s because we’re just two weeks out from the annual HIMSS Conference which will convene thousands of health IT wonks, users and developers (I am the former), but I’ve received several reports this week speaking to health engagement and technology that are worth some trend-weaving. As my colleague-friends Gregg Masters of Health Innovation Media (@2healthguru) and John Moore of Chilmark Research (@john_chilmark) challenged me on Twitter earlier this week: are we scaling sustained, real patient engagement and empowerment yet? Let’s dive into the
The $4 Trillion Health Economy of 2020
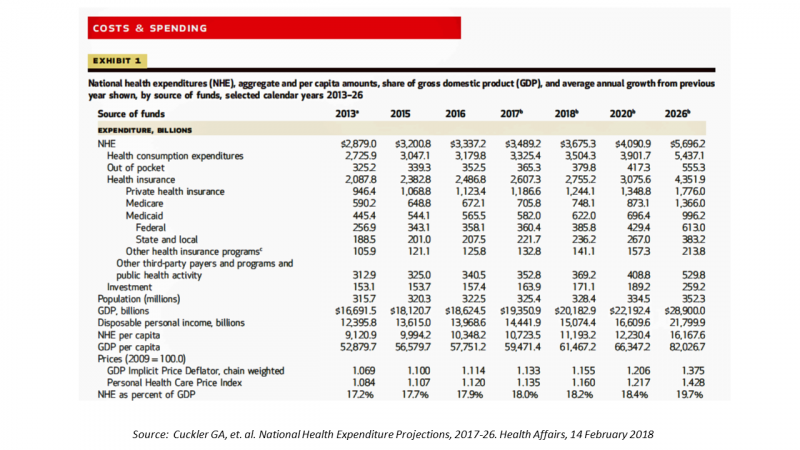
In 2020, national health expenditures (NHE) in the United States will exceed $4 trillion to cover 334.5 million Americans. That equates to 18.4% of the Gross Domestic Product (GDP) and $12,230.40 of health spending per person. I sat in on a press call today with researchers from the Office of the Actuary working in the Centers for Medicare and Medicaid Services (CMS) to review the annual forecast of the NHE, published in Health Affairs in a statistically-dense eleven page article titled, National Health Expenditure Projections, 2017-2026: Despite Uncertainty, Fundamentals Primarily Drive Spending Growth. What are those “fundamentals” pushing up healthcare spending?
When Buying a Pair of Jeans Competes With Filling a Prescription at CVS in Target

Stories about three fashion brands have me thinking about women and their health economics. Stay with me. Target unveiled its new line of clothing, Universal Thread, which features pieces that are accessible to women who may be dealing with physical limitations or sensory challenges. I first read about Universal Thread on The Mighty website, which is a community of over 1 million people interested in connecting on health and disabilities. As The Mighty described, the brand Universal Thread, “is centered around denim since it is a staple in many women’s wardrobes, but denim can be uncomfortable for many people with disabilities
Getting Real About Social Determinants of Health
New research points out that real people live real lives, and our assumptions about social determinants of health (SDOH) may need to be better informed by those real lives. I read three reports in the past week sobering up my bullish #SDOH ethos dealing with food deserts, transportation, and health service access — three key social determinants of health. To remind you about the social determinants, here’s a graphic from Kaiser Family Foundation that summarizes the key pillars of SDOH. Assumption 1: Food deserts in and of themselves diminish peoples’ healthy nutrition lifestyles. Low-income households who are exposed to the same food-buying
U.S. Workers Say Health Care is the Most Critical Issue Facing the Nation
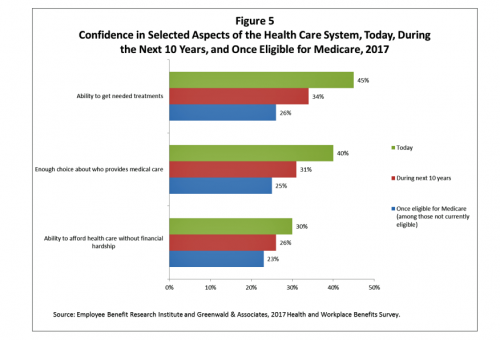
Health care ranks highest among working Americans as the top critical issue facing the country, well above terrorism, the role of the Federal government, unemployment and jobs, education, immigration and taxes. Over half of American workers also rate the country’s healthcare system as “poor” or “fair,” based on the results of the EBRI/Greenwald & Associates Health and Workplace Benefits Survey. Workers dissatisfaction with U.S. healthcare is based largely on cost: one-half of workers experienced an increase in health care costs in the past year. Furthermore, only 22% are satisfied with the cost of their health insurance plan, 18% are satisfied
Warren Buffett’s Healthcare Cost Tapeworm & His Alliance with Amazon and JPMorgan

The fact that the average U.S. employer committed to spend nearly $27,000 a year for a PPO to cover a family of 4 in America in 2017 is the most important rationale underlying the announcement that Amazon, Berkshire-Hathaway, and JP Morgan made on 30th January 2017. That news immediately shook Wall Street trading, sending downward shocks down the proverbial spines of healthcare insurance plans and suppliers to the industry — legacy healthcare companies that scale patient-members and healthcare supplies, like pills and surgical implants. The “new competition” chart published in the Wall Street Journal in the morning illustrates those shock
Health Insurance Costs Stress US Whether We’re Rich or Not / and Why a $0 Budget for CFPB Matters for Healthcare

Health care costs cause anxiety for U.S. adults, regardless of their affluence, we learn in Uncertainty About Healthcare, the latest Stress in America poll from the American Psychological Association. The big stat is that 2 in 3 Americans say the cost of health insurance is a stressor for them or their loved ones, whether the person earns more or less than $50,000 a year. Underneath that top-line are some demographic differences. Millennials are most concerned about access to mental health care compared with Boomers and older adults. Reproductive care access is of most interest to Millennials and Gen Xers. Two-thirds
In the U.S., Spend More, Get Less Health Care: the Latest HCCI Data

Picture this scenario: you, the consumer, take a dollar and spend it, and you get 90 cents back. In what industry is that happening? Here’s the financial state of healthcare in America, explained in the 2016 Health Care Cost and Utilization Report from the Health Care Cost Institute (HCCI). We live in an era of Amazon-Primed consumers, digital couponing, and expectations of free news in front of paywalls. We are all in search of value, even as the U.S. economy continues to recover on a macroeconomic basis. But that hasn’t yet translated to many peoples’ home economics. In this personal
What Healthcare Can Learn from A Pig and Piggy Bank via Santander Bank

When patients feel disrespected in a medical exam room, they will be less likely to follow instructions they receive from a doctor. Research from the Altarum Institute revealed this fundamental finding. The chart shows that feeling respected reduces a patient’s diabetes medication adherence by a factor of nearly 2x, and is a risk factor for poorly managed diabetes. Furthermore, consumers who feel disrespected by providers are three times more likely to not believe doctors are accurate sources of information than consumers who do feel respected. And, patients with diabetes who do not feel respected are one-third more likely to have poorly
Calling Out Health Disparities on Martin Luther King Day 2018

On this day appreciating the legacy of Martin Luther King, Jr., I post a photo of him in my hometown of Detroit in 1963, giving a preliminary version of the “I Have a Dream” speech he would deliver two months later in Washington, DC. Wisdom from the speech: “But now more than ever before, America is forced to grapple with this problem, for the shape of the world today does not afford us the luxury of an anemic democracy. The price that this nation must pay for the continued oppression and exploitation of the Negro or any other minority group
Most Americans Say Healthcare is #1 Policy Issue Entering 2018

Concerns about health care are, by a large margin, the top domestic policy issue U.S. voters identified as they enter 2018. The proportion of Americans citing healthcare as the top public agenda priority grew by 50% since 2016, from 31% two years ago to 48%. Taxes rank #2 this year, garnering 31% of Americans’ concerned, followed by immigration, which has remained flat cited by about one-in-four Americans. The Associated Press (AP)-NORC Center for Public Affairs Research polled 1,444 U.S. adults 18 and over between November 30 and December 4, 2017 for this survey. While one-half of Americans would like the
Let’s Increase Life Expectancy in America in 2018 – A New Year for Opioids, Social Determinants, and Financial Health
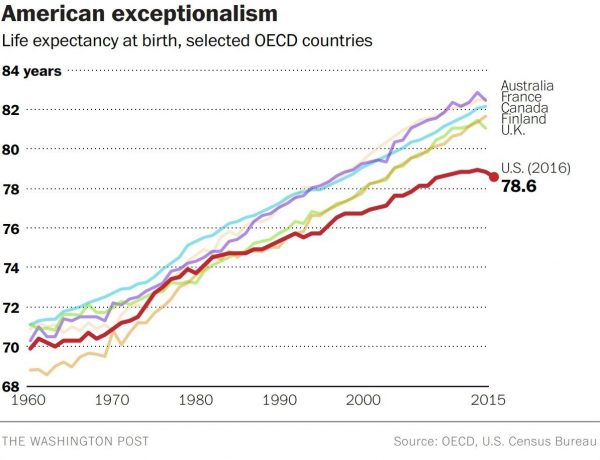
For this end-of-year post leading into 2018, I choose to address the big topic of how long we live in America, and what underpins the sobering fact that life expectancy is falling. Life expectancy in the United States declined to 78.6 years in 2016, placing America at number 37 on the list of 137 countries the World Economic Forum (WEF) has ranked in their annual Global Competitiveness Report 2017-2018. The first chart shows the declining years for Americans compared with health citizens of Australia, France, Canada, Finland, and the UK. While Australians’ and Britons’ life expectancies declined from 2015-16, their
Will Getting Bigger Make Hospitals Get Better?
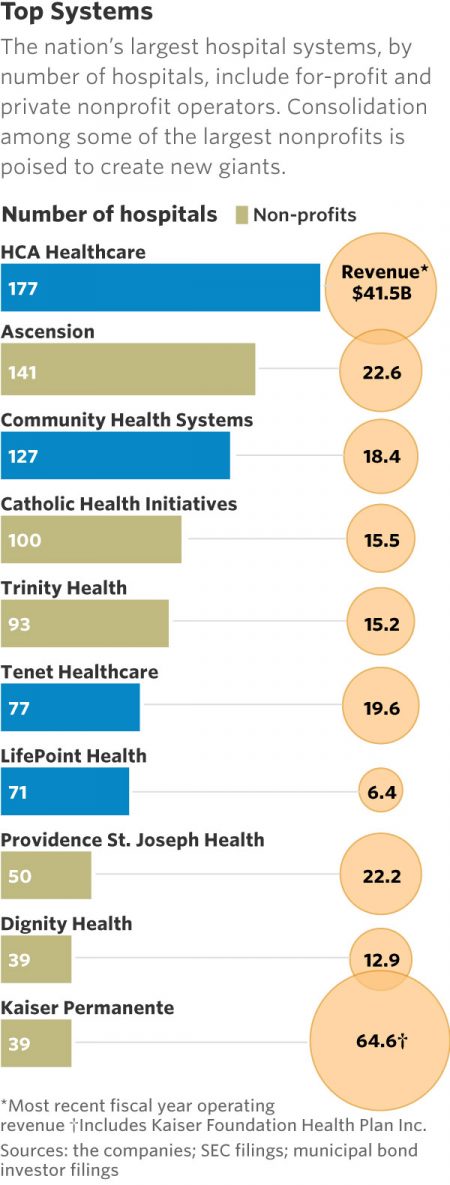
This month, two hospital mega-mergers were announced between Ascension and Providence, two of the nation’s largest hospital groups; and, between CHI and Dignity Health. In terms of size, the CHI and Dignity combination would create a larger company than McDonald’s or Macy’s in terms of projected $28 bn of revenue. (Use the chart of America’s top systems to do the math). For context, other hospital stories this week discuss in southern New Jersey. And this week, the New Jersey Hospital Association annual report called the hospital industry the “$23.4 billion economic bedrock” of the state. Add a third important item
The Patient as Payor – Consumers and the Government Bear the Largest Share of Healthcare Spending in America
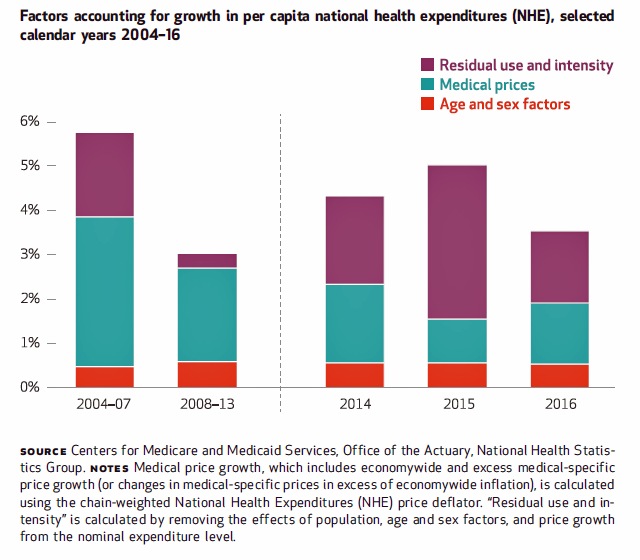
The biggest healthcare spenders in the United States are households and the Federal government, each responsible for paying 28% of the $3.3 trillion spent in 2016. Private business — that is, employers covering healthcare insurance — paid for 20% of healthcare costs in 2016, based on calculations from the CMS Office of the Actuary’s report on 2016 National Health Expenditures. The positive spin on this report is that overall national health spending grew at a slower rate in 2016, at 4.3% after 5.8% growth in 2015. This was due to a decline in the growth rates for the use of
The State of Financial Wellness and Health in America – Suffering Across the Ages
Nearly one-half of Americans are challenged by low financial well-being. Compared to emotional/mental, job/career, social, physical, and financial, it’s this last lens on personal health that gets the lowest ratings for the largest number of Americans. The second most worrying factor diminishing well-being is a tie between physical health and social health. Welcome to The uncomfortable reality of financial wellbeing, a report on the 2017 Financial Mindset Study Highlights from Alight Solutions, an HR services company. The first chart arrays the well-being rankings across the five factors, showing that just over one-half of Americans have more positive views on their emotional
High-Deductibles Do Not Automatically Inspire Healthcare Consumerism
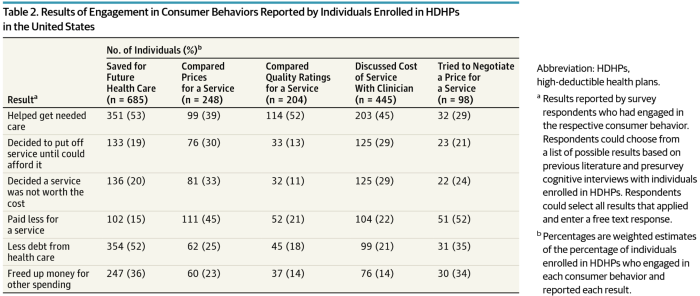
It takes more than enrolling in a high-deductible health plan (HDHP) for someone to immediately morph into an effective health care “consumer.” Research from Dr. Jeffrey Kullgren and his team from the University of Michigan found that enrollees in HDHPs could garner more benefits from these plans were people better informed about how to use them, including how to save for them and spend money once enrolled in them. The team’s research letter was published in JAMA Internal Medicine on 27 November 2017. The discussion details results of a survey conducted among 1,637 people 18 to 64 years of age
Don’t Touch My Entitlements to Pay For Tax Reform, Most Americans Say to Congress
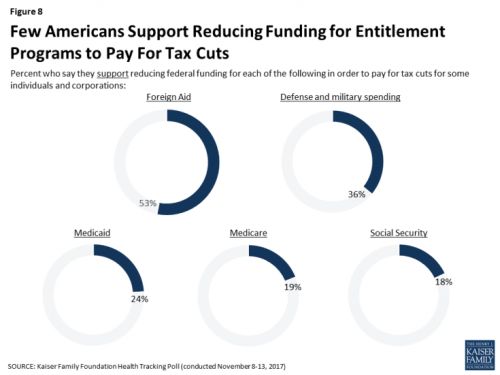
To pay for tax cuts, take money from foreign aid if you must, 1 in 2 Americans say. But do not touch my Medicaid, Medicare, or Social Security, insist the majority of U.S. adults gauged by the November 2017 Kaiser Health Tracking Poll. This month’s survey looks at Americans’ priorities for President Trump and the Congress in light of the GOP tax reforms emerging from Capitol Hill. While reforming taxes is considered a top priority for the President and Congress by 3 in 10 people, two healthcare policy issues are more important to U.S. adults: first, 62% of U.S. adults
Stress is US: Health Care Is the #1 Stressor in America
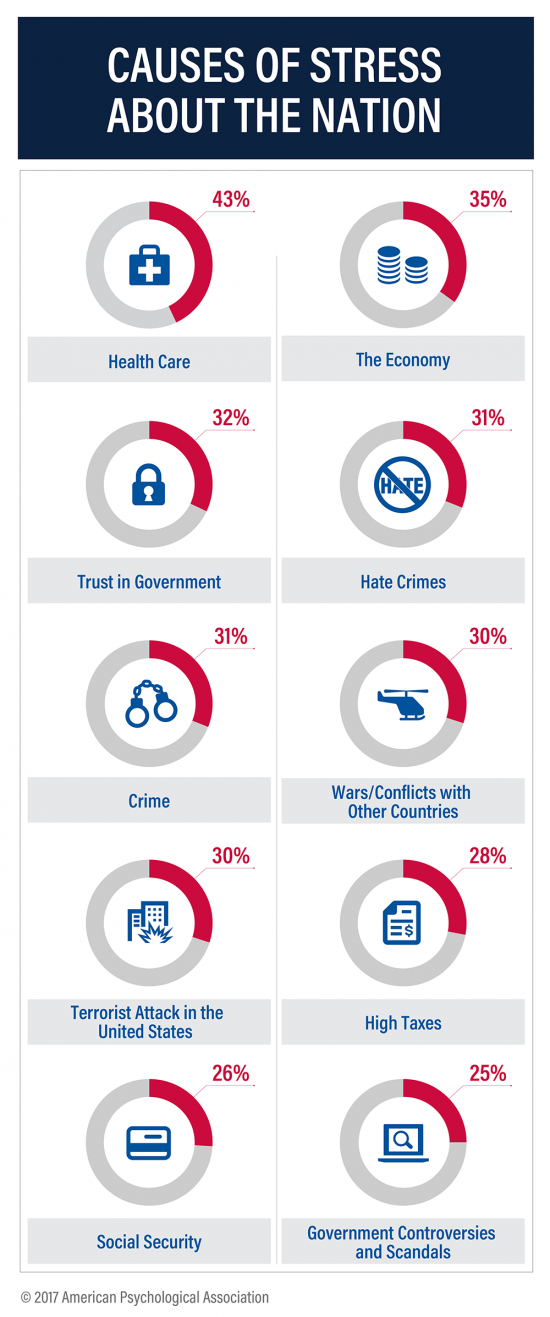
Above the economy, trust in government, crime, war, terrorism, and taxes, health care is the top cause of stress in America. For ten years, the American Psychological Association has gauged Americans’ collective mood in their ongoing study, Stress in America. The latest report is The State of Our Nation, published this month, finding that we’re at the “lowest point in our nation’s history” according to 59% of Americans. The 2016 national election in the U.S. raised the stress-stakes, when APA released a stress study we discussed here in Health Populi. The election season was a source of stress for 52%
Health Care Is 2.5 More Expensive Than Food for the Average U.S. Family
The math is straightforward. Assume “A” equals $59.039, the median household income in 2016. Assume “B” is $18,142, the mean employer-sponsored family insurance premium last year. B divided by A equals 30.7%, which is the percent of the average U.S. family’s income represented by the premium cost of health insurance. Compare that to what American households spent on food: just over $7,000, including groceries and eating out (which is garnering a larger share of U.S. eating opportunities, a topic for another post). Thus, health care represents, via the home’s health insurance premium, represents 2.5 times more than food for the
In the Post-Weinstein Era, How to Market Health to Women: Philips, Kalenji, and Libresse Getting It Right

“With Mad Men still in charge, ad campaigns miss the mark,” an editorial published this week in the Financial Times asserts. Leave it to a fiscally conservative British publication to be spot-on about a particularly, but not uniquely, American challenge, in this post-Weinstein (Miramax), -Price (Amazon), and today, -Halperin (MSNBC) moment of sexual harassment revelations. In health/care, women are key consumers, buyers and influencers, yet under-represented in the Mad Men demographic of senior advertising executives, as the data-driven FT essay points out. So it’s especially heartening to find this month a few examples of empowering, inspiring ad campaigns getting health/care marketing
Four Things We Want in 2017: Financial Health, Relationships, Good Food, and Sleep

THINK: money and love. To find health, working-aged people seek financial stability and good relationships, according to the Consumer Health POV Report from Welltok, meQuilibrium, and Zipongo, featured in their webinar broadcast today. The online consumer survey was conducted among 2,000 full-time working U.S. adults in August 2017, segmented roughly into thirds by Boomers (37%), Gen Xers (32%), and Millennials (31%). Much lower down the priority list for healthy living are managing food, sleep, and stress based on the poll. Feeling stress is universal across most consumers in each of the three generational cohorts, especially related to work and finance.
Income Inequality For Older Americans Among Highest in the World – What This Means for Healthcare
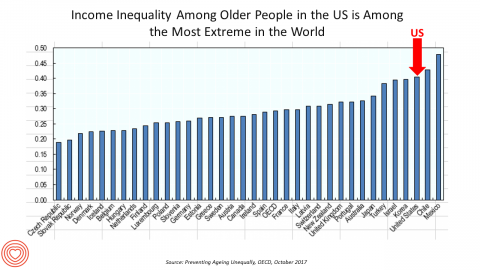
Old-age inequality among current retirees in the U.S. is already greater than in ever OECD country except Chile and Mexico, revealed in Preventing Ageing Unequally from the OECD. Key findings from the report are that: Inequalities in education, health, employment and income start building up from early ages At all ages, people in bad health work less and earn less. Over a career, bad health reduces lifetime earnings of low-educated men by 33%, while the loss is only 17% for highly-educated men Gender inequality in old age, however, is likely to remain substantial: annual pension payments to the over-65s today are
Most Americans Are Concerned About Healthcare Policy, and Costs Top the List of Concerns
4 in 5 Americans are aware of potential changes to healthcare policy brewing in Washington, DC. 92% of them are concerned about those changes, according to Healthcare Consumers in a Time of Uncertainty, the fifth annual survey from Transamerica Center for Health Studies. Peoples’ most-shared fears are losing their coverage for pre-existing conditions, out-of-pocket spending, and a ban on lifetime limits. That boils down to one thing: cost. That is, cost, for having to spend money on services not-covered by their health insurance plan; cost for out-of-pocket items under-insured, denied, or requiring coinsurance or co-payments; and, catastrophic costs that rise beyond
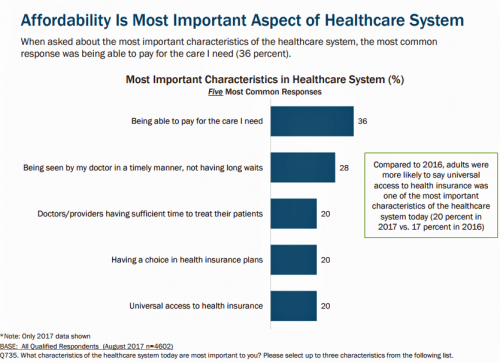
The Patient As Payor – Americans Bundle Financial Wellness and Healthcare Costs
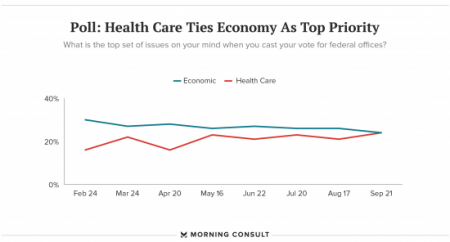
Healthcare and the economy tied for US voters’ top issue last week, as the prospects for repealing the Affordable Care Act faded by the weekend. This Morning Consult poll was published 28th September 2017, as it became clear that the Graham-Cassidy health reform bill would lose at least three key votes the legislation needed for passage: from Rand Paul, Susan Collins, and John McCain. Liz Hamel, who directs the Kaiser Family Foundation’s survey research, told Morning Consult that, “when people say ‘health care,’ they often are actually talking about the economic issue of health care.”
Out-Of-Pocket Healthcare Costs Grow in the Family Budget
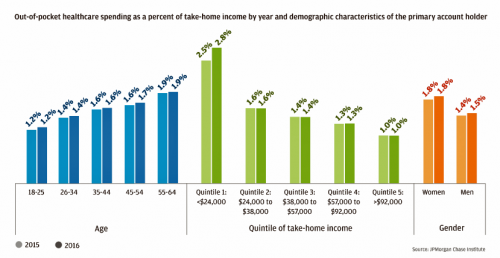
For each dollar spent on healthcare in the United States, families paid 28 cents, according to the U.S. National Health Expenditure Accounts for 2015. Welcome to the new era of Americans and medical banking, with new insights provided by the largest of banks, JP Morgan Chase, in Paying Out-of-Pocket: The Healthcare Spending of 2 Million U.S. Families, from JP Morgan Chase. Chase is the largest bank in America based on its assets. They’ve mined 2.3 million de-identified records of Chase consumers in their banking network to learn about customers’ healthcare spending. These data represent spending between 2013 and 2016, detailed
Employees Continue To Pick Up More Health Insurance Costs, Even As Their Growth Slows
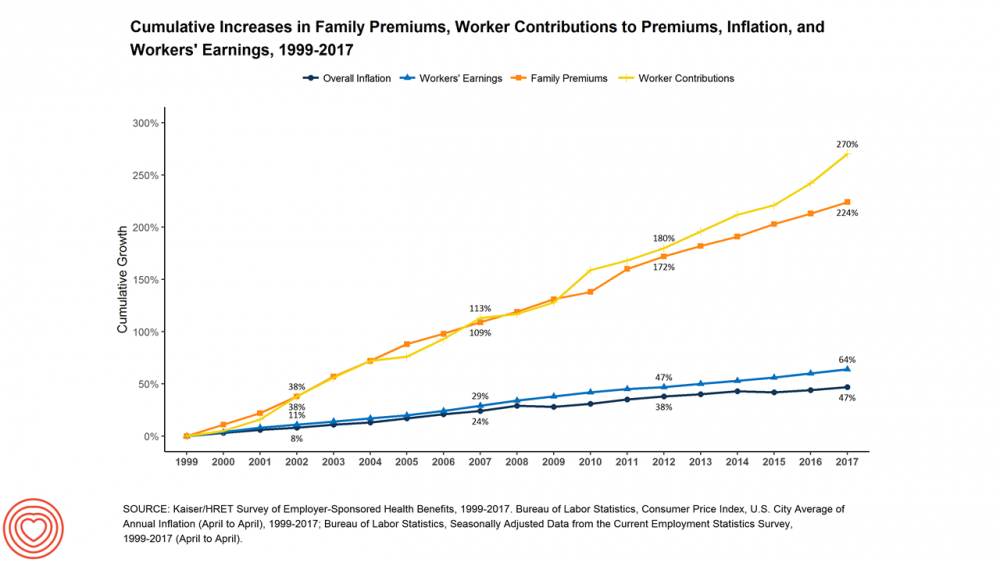
The average cost of an employer=sponsored health plan for a family reached $18,764 in 2017. While this premium grew overall by a historically relative low of 3.4%, employees covered under that plan faced an increase of 8.3% over what their plan share cost them in 2016, according to the 2017 Employer Health Benefit Survey published today by the Kaiser Family Foundation. [Here’s a link to the 2016 KFF report, which provided the baseline for this 8.3% calculation]. Average family premiums at the workplace rose 19% since 2012, a slowdown from the two previous five-year periods — 30% between 2007 and 2012, and
Patients Are Looking to Finance Healthcare Over Time
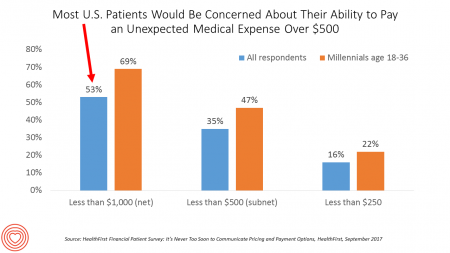
Most U.S. patients want healthcare providers to offer cost information before a procedure, and whether doctors offer financial options to help them extend payments over time. This is an automotive or home appliance procedure we’re talking about. It’s healthcare services, and American patients are now the third largest payors to providers in the nation. Thus, the title of a new report summarizing a consumer survey from HealthFirst notes, “It’s Never Too Soon to Communicate Pricing and Payment Options. The study found that two-thirds of U.S. consumers would like healthcare providers to discuss financing options; however, only 18 percent of providers have
Celebrating 10 Years of Health Populi, 10 Healthcare Milestones and Learnings

Happy anniversary to me…well, to the Health Populi blog! It’s ten years this week since I launched this site, to share my (then) 20 years of experience advising health care stakeholders in the U.S. and Europe at the convergence of health, economics, technology, and people. To celebrate the decade’s worth of 1,791 posts here on Health Populi (all written by me in my independent voice), I’ll offer ten health/care milestones that represent key themes covered from early September 2007 through to today… 1. Healthcare is one-fifth of the national U.S. economy, and the top worrisome line item in the American
Transparency in Drug Prices, from OTC to Oncology

While on vacation in Bermuda, I found a box of private label ibuprofen for $2.45 for 20 – 200mg tablets, and one for Advil PM for $10.50 for the same number of pills, same strength. I’ve just returned from a lovely week’s holiday. When I travel, whether for work or vacation, it’s always a sort of Busman’s Holiday for me as I love to seek out health destinations wherever I go. So it was natural for me to spot the Dockyard Pharmacy at the port in Hamilton and wander in. I made my way back to the well-stocked pharmacy counter,
Patients’ Healthcare Payment Problems Are Providers’, Too
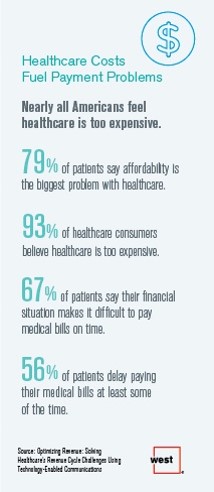
Three-quarters of patients’ decisions on whether to seek services from healthcare providers are impacted by high deductible health plans. This impacts the finances of both patients and providers: 56% of patients’ payments to healthcare providers are delayed some of the time, noted in Optimizing Revenue: Solving Healthcare’s Revenue Cycle Challenges Using Technology Enabled Communications, published today by West. Underneath that 56% of patients delaying payments, 12% say they “always delay” payment, and 16% say they “frequently delay” payment. West engaged Kelton Global to survey 1,010 U.S. adults 18 and over along with 236 healthcare providers to gauge their experiences with
A Couple Retiring Today Will Need $275,000 For Health Care Expenses
A 65-year-old couple in America, retiring in 2017, will need to have saved $275,000 to cover their health and medical costs in retirement. This represents a $15,000 (5.8%) increase from last year’s number of $260,000, according to the annual retirement healthcare cost study from Fidelity Investments. This number does not include long-term care costs — only medical and health care spending. Here’s a link to my take on last year’s Fidelity healthcare retirement cost study: Health Care Costs in Retirement Will Run $260K If You’re Retiring This Year. Note that the 2016 cost was also $15,000 greater than the retirement healthcare costs calculated
Women’s Access to Health Care Improved Under the Affordable Care Act
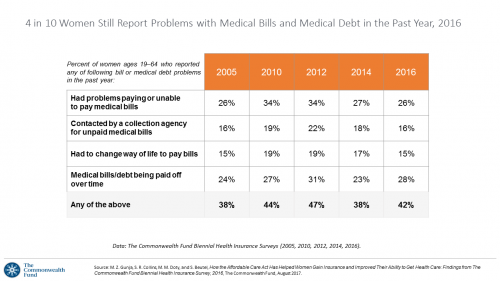
The Affordable Care Act (ACT) was implemented in 2010. Since the inception of the ACA, the proportion of uninsured women in the U.S. fell by nearly one-half, from 19 million in 2010 to 11 million in 2016. The Commonwealth Fund has documented the healthcare gains that American women made since the ACA launch in their issue brief, How the Affordable Care Act Has Helped Women Gain Insurance and Improved Their Ability to Get Health Care, published earlier this month. The first chart talks about insurance: health care plan coverage, which is the prime raison d’être of the ACA. It’s
Cost and Personalization Are Key For Health Consumers Who Shop for Health Plans
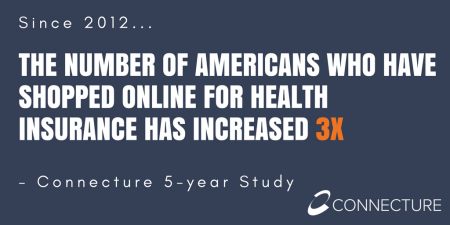
Between 2012 and 2017, the number of US consumers who shopped online for health insurance grew by three times, from 14% to 42%, according to a survey from Connecture. Cost first, then “keeping my doctor,” are the two top considerations when shopping for health insurance. 71% of consumers would consider switching their doctor(s) to save on plan costs. Beyond clinician cost, health plans shoppers are also concerned with prescription drug costs in supporting their decisions. 80% of consumers would be willing to talk with their doctors about prescription drug alternatives, looking for a balance between convenience
Employer Health Benefits Stable In the Midst of Uncertain Health Politics
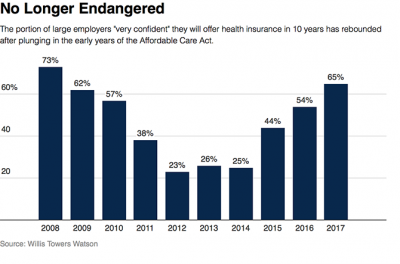
As we look for signs of stability in U.S. health care, there’s one stakeholder that’s holding firm: employers providing healthcare benefits. Two studies out this week demonstrate companies’ commitment to sponsoring health insurance benefits….with continued tweaks to benefit design that nudges workers toward healthier behaviors, lower cost-settings, and greater cost-sharing. As Julie Stone, senior benefits consultant with Willis Towers Watson (WLTW), noted, “The extent of uncertainty in Washington has made people reluctant to make changes to their benefit programs without knowing what’s happening. They’re taking a wait-and-see attitude.” First, the Willis Towers Watson 22nd annual Best Practices in Health Care Employer
Patients Want Doctors To Know How Much Their Drugs Cost
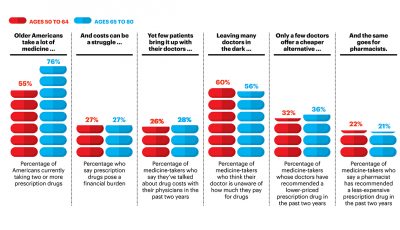
Patients want their doctors to know what their personal costs for medicines are; 42% of patients also believe their doctor is aware of how much they spend on prescription drugs. However, 61% of these people have not talked with doctors about drug prices. Nor do most doctors have access to this kind of information at the individual patient level. One important tactic to addressing overall healthcare costs, and managing the prescription drug line item in those costs, is discussed in Doctors and Pharmacists: An Underused Resource to Manage Drug Costs for Older Adults, a report on a survey sponsored
Learning From Adam Niskar – Living Beyond The Wheelchair

After diving into Walnut Lake in suburban Detroit, Adam Niskar sustained a spinal injury that would paralyze much of his body for the rest of his life. The trauma didn’t paralyze his life and living, though. But today, my family will celebrate that life at Adam’s memorial service. Adam was my cousin. He was one of the best-loved people on the planet, and that was part of a therapeutic recipe that sustained him from the traumatic accident in 1999 until Monday, July 31st, 2017, when Adam passed away from complications due to an infection that, this time around, his body




 Thank you, Jared Johnson, for including me on the list of the
Thank you, Jared Johnson, for including me on the list of the  I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a