Health Care and the Democratic Debates – Part 1 – Medicare For All, Rx Prices, Guns and Mental Health

Twenty Democratic Presidential candidates each have a handful of minutes to make their case for scoring the 2020 nomination, “debating” last night and tonight on major issues facing the United States. I watched every minute, iPad at the ready, taking detailed notes during the 120 minutes of political discourse conducted at breakneck speed. Lester Holt, Savannah Guthrie, and Jose Diaz-Balart asked the ten candidates questions covering guns, butter (the economy), immigration, climate change, and of course, health care — what I’m focusing on in this post, the first of two-debate-days-in-a-row. The first ten of twenty candidates in this debate were,
Talk to Me About My Health, Medicare Advantage Beneficiaries Tell J.D. Power
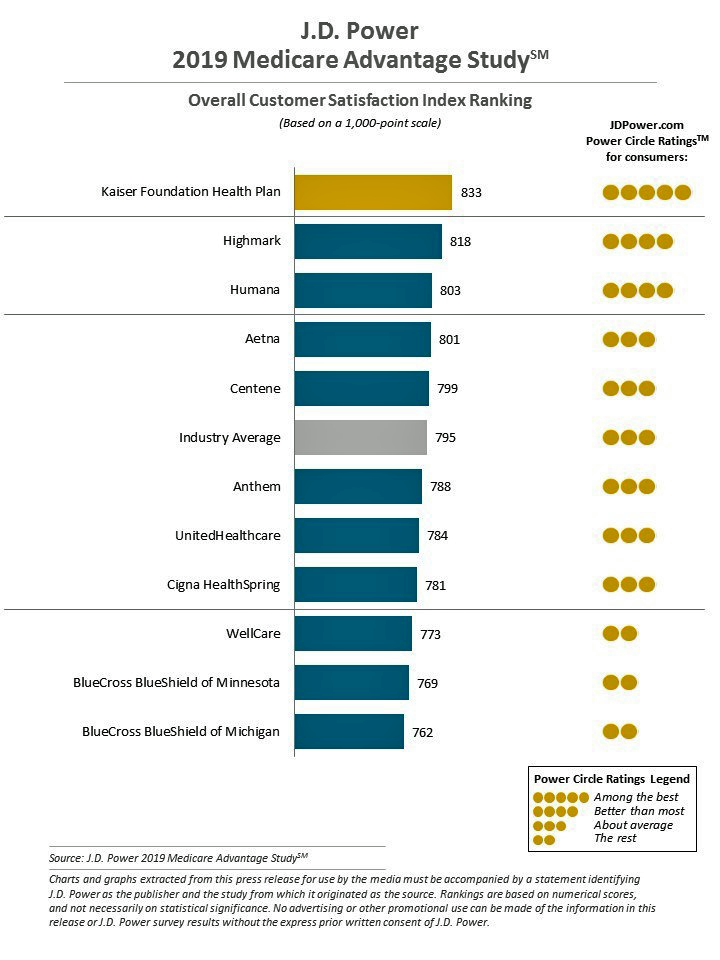
Cost is the major reason why Medicare Advantage plan beneficiaries switch plans, but people who switch also tend to have lower satisfaction scores based on non-cost factors. Those ratings have a lot to do with information and communication, according to J.D. Power’s 2019 Medicare Advantage Plan Study. The Study explores MA beneficiaries’ views on six factors: Coverage and benefits Provider choice Cost Customer service Information and communication, and Billing and payment. Kaiser Foundation Health Plan garnered the top spot for the fifth year in-a-row. By feature, Kaiser achieved 5 “Power Circles” for all factors except for cost and provider choice,
Americans Could Foster a Health Consumer Movement, Families USA Envisions
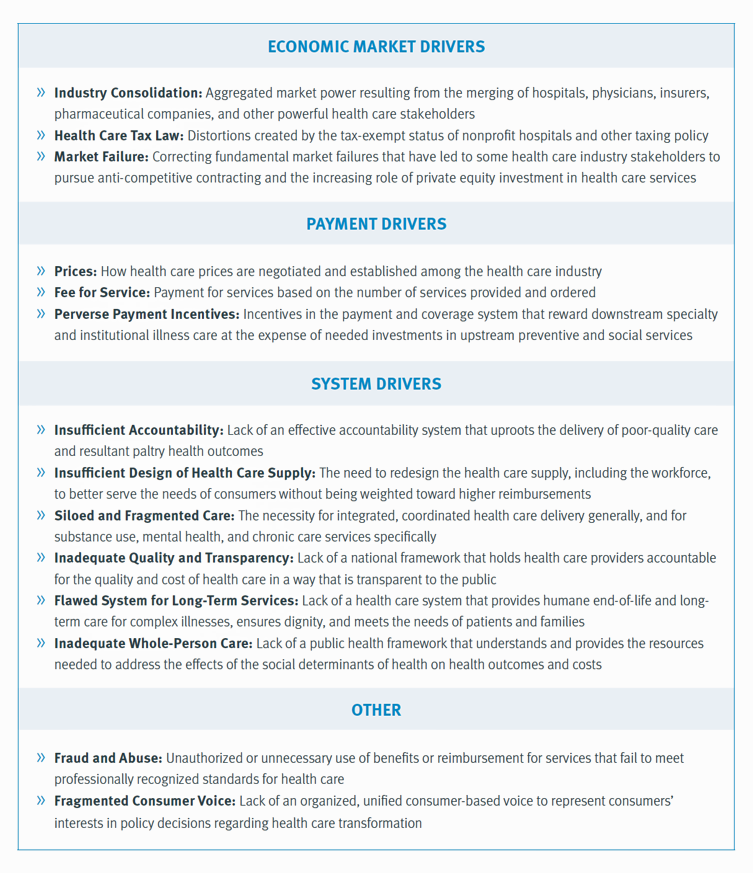
Employers, health care providers, unions, leaders and — first and foremost, consumers — must come together to build a more accessible, affordable health care system in America, proposes a call-to-action fostered by a Families USA coalition called Consumers First: The Alliance to Make the Health Care System Work for Everyone. The diverse partners in this Alliance include the American Academy of Family Physicians, AFSCME (the largest public service employees’ union in the U.S.), the American Benefits Council (which represents employers), the American Federation of Teachers (AFT), First Focus (a bipartisan children’s advocacy organization), and the Pacific Business Group on Health
How Consumers’ Belt-Tightening Could Impact Health/Care – Insights from Deloitte’s Retail Team

Over the ten years between 2007 and 2017, U.S. consumer spending for education, food and health care substantially grew, crowding out spending for other categories like transportation and housing. Furthermore, income disparity between wealthy Americans and people earning lower-incomes dramatically widened: between 2007-2017, income for high-income earners grew 1,305 percent more than lower-incomes. These two statistics set the kitchen table for spending in and beyond 2019, particularly for younger people living in America, considered in Deloitte’s report, The consumer is changing, but perhaps not how you think. The authors are part of Deloitte Consulting’s Retail team. The retail spending data
Two-Thirds of Americans Say Healthcare Doesn’t Work Well, in RealClear Politics Poll

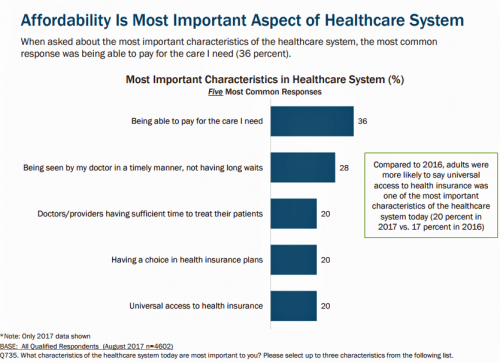
Health care is the top issue facing the U.S. today, one in three Americans says, with another one-fourth pointing to the economy. Together, health care + the economy rank the top issues for 62% of Americans. Health care and the economy are, in fact, intimately tied in every American’s personal household economy I assert in my book, HealthConsuming: From Health Consumer to Health Citizen. This poll from RealClear Politics, conducted in late April/early May 2019, makes my point that the patient is the consumer and, facing deductibles and more financial exposure to footing the medical bill, the payor. Fully
The 3 A’s That Millennials Want From Healthcare: Affordability, Accessibility, Availability

With lower expectations of and satisfaction with health care, Millennials in America seek three things: available, accessible, and affordable services, research from the Transamerica Center for Health Studies has found. Far and away the top reason for not obtaining health insurance in 2018 was that it was simply too expensive, cited by 60% of Millennials. Following that, 26% of Millennials noted that paying the tax penalty plus personal medical expenses were, together, less expensive than available health options. While Millennials were least likely to visit a doctor’s office in the past year, they had the most likelihood of making a
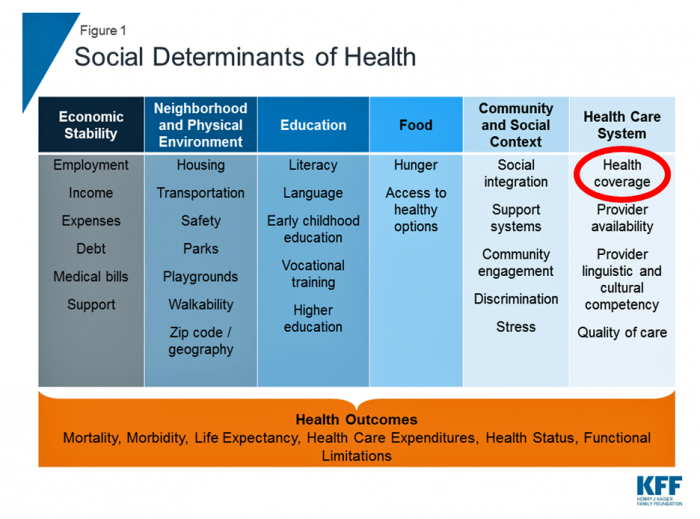
Scaling the Social Determinants of Health – McKinsey and Kaiser’s Bold Move

People who are in poor health or use more health care services are more likely to report multiple unmet social needs, such as food insecurity, unsafe neighborhoods, lack of good housing, social isolation, and poor transportation access, found through a survey conducted by McKinsey. The results are summarized in Addressing the Social Determinants of Health. The growing recognition of the influence of social determinants reached a tipping point last week with the news that Kaiser-Permanente would work with Unite US to scale services to people who need them. The mainstreaming of SDoH speaks to the awareness that health is made
Prescription Drug Costs In America Through the Patient Lens, via IQVIA, GoodRx and a New $2 Million Therapy

Americans consumed 17.6 prescriptions per person in 2018, two in three of which treated chronic conditions. Welcome to Medicine Use and Spending in the U.S. , the annual review of prescription drug supply, demand and Rx pricing dynamics from the IQVIA Institute for Human Data Science. In a call with analysts this week in which I participated, the Institute’s Executive Director Murray Aitken discussed the report which looks back at 2018 and forward to 2023 with scenarios about what the U.S. prescription drug market might look like five years from now. The report is organized into four sections: medical use
Assessing the GAO’s Report on Single-Payer Healthcare in America: Let’s Re-Imagine Workflow

Calls for universal health care, some under the banner of Medicare for All,” are growing among some policy makers and presidential candidates looking to run in 2020. As a response, the Chairman of the House Budget Committee in the U.S. Congress, Rep. John Yarmuth (D-Ky.), asked the Congressional Budget Office (CBO) to develop a report outlining definitions and concepts for a single-payer health care system in the U.S. The result of this ask is the report, Key Design Components and Considerations for Establishing a Single-Payer Health Care System, published on 1st May by the CBO. The report provides
Will Health Consumers Morph Into Health Citizens? HealthConsuming Explains, Part 5

The last chapter (8) of HealthConsuming considers whether Americans can become “health citizens.” “Citizens” in this sense goes back to the Ancient Greeks: I return to Hippocrates, whose name is, of course, the root of The Hippocratic Oath that physicians take. Greece was the birthplace of Democracy with a capital “D.” Hippocrates’ book The Corpus is thought to be one of the first medical textbooks. The text covered social, physical, and nutritional influences, and the concept of “place” for health and well-being. Here, the discussion detailed the roles of air and water for health. The Hippocratic texts also coached doctors to
A Dose of Optimism Is a Prescription for Financial Health, Says Frost Bank

People define their personal health and well-being broadly, well beyond physical health. Mental wellness, physical appearance, social connections, and financial wellness all add into our self-health definitions. Mind Over Money is a consumer study conducted by Frost Bank, working with FleischmanHillard, connecting the dots between optimism and financial health. The top-line of the study is that people who are optimists have roughly two-thirds fewer days of financial stress per year than pessimists. Put another way, pessimists stress about finances 62% of the year, shown in the first chart from the study. This translates into 62% of optimists having better financial
Americans’ Trust in U.S. Healthcare Lags Tech — and Women Are Particularly Cynical
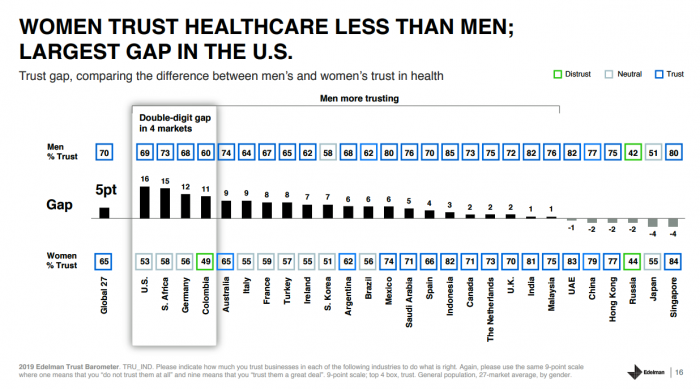
The 2019 Edelman Trust Barometer measured the biggest gap in trust for the healthcare industry between the U.S. “informed public” and the mass population. Fewer American women, too, trust the healthcare industry than men do. “This inequality of trust may be reflective of the mass population continuing to feel left behind as compared to others, even as they recognize the advances that are being made that could benefit them. Given tone and tenor of the day, and particularly among mass population, healthcare may continue to see increasing demands for change and regulation,” Susan Isenberg, Edelman’s head of healthcare, notes in
World Health Day 2019: Let’s Celebrate Food, Climate, Insurance Coverage and Connectivity
Today, 7 April, is World Health Day. With that in mind, I devote this post to three key social determinants of health (SDOH) that are top-of-mind for me these days: food for health, climate change, and universal health coverage. UHC happens to be WHO’s focus for World Health Day 2019. [As a bonus, I’ll add in a fourth SDOH in the Hot Points for good measure and health-making]. Why a World Health Day? you may be asking. WHO says it’s, “a chance to celebrate health and remind world leaders that everyone should be able to access the health care they need,
In the Modern Workplace, Workers Favor More Money, New Kinds of Benefits, and Purpose
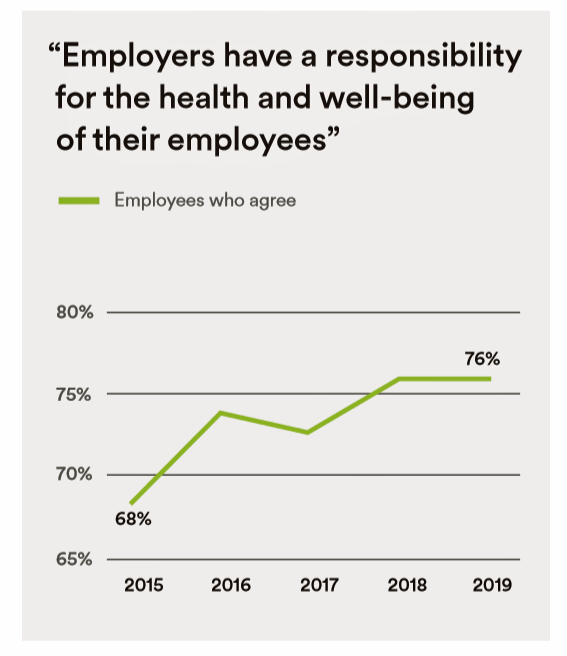
Today, April 2nd, is National Employee Benefits Day. Who knew? To mark the occasion, I’m mining an important new report from MetLife, Thriving in the New Work-Life World, the company’s 17th annual U.S. employee benefit trends study with new data for 2019. For the research, MetLife interviewed 2,500 benefits decision makers and influencers of companies with at least two employees. 20% of the firms employed over 10,000 workers; 20%, 50 and fewer staff. Companies polled represented a broad range of industries: 11% in health care and social assistance, 10% in education, 9% manufacturing, 8% each retail and information technology, 7%
In the U.S., Patients Consider Costs and Insurance Essential to Their Overall Health Experience
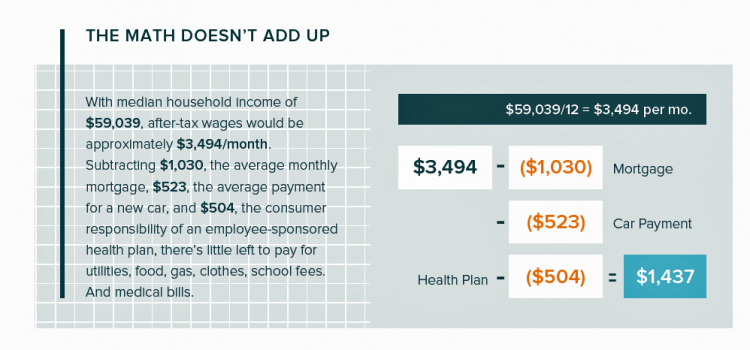
Patients in the U.S. assume the role of payor when they are enrolled in high-deductible health plans. People are also the payor when dealing with paying greater co-payments for prescription drugs, especially as new therapeutic innovations come out of pipelines into commercial markets bearing six-digit prices for oncology and other categories. For mainstream Americans, “the math doesn’t add up” for paying medical bills out of median household budgets, based on the calculations in the 2019 VisitPay Report. Given a $60K median U.S. income and average monthly mortgage and auto payments, there’s not much consumer margin to cover food, utilities, petrol,
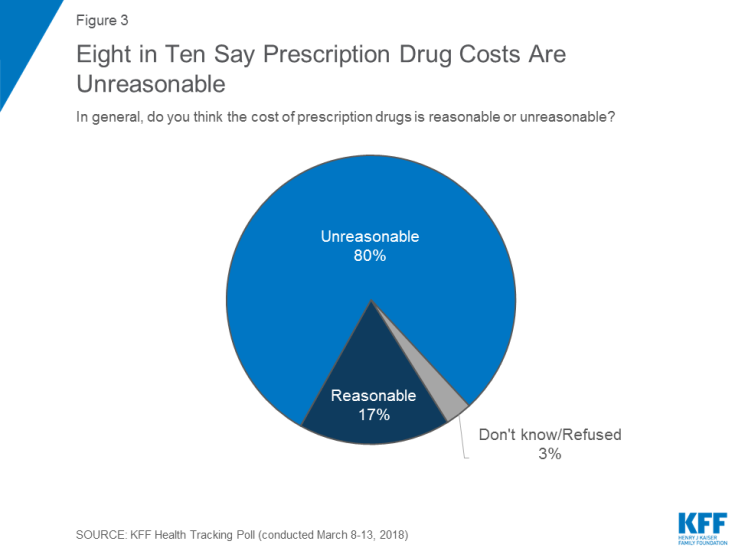
Most Americans Blame Drug Companies, Insurers, and Hospitals for High Health Care Costs

There’s little agreement between Democrats and Republicans on a plethora of issues in American public life. But one issue that brings U.S. citizens together is agreement that the cost of health care is too high in the country, and that pharma, health plans, and providers are to blame. Welcome to health politics in America as of March 2019, according to The Public and High U.S. Health Care Costs, a poll conducted by POLITICO and the Harvard T.H. Chan School of Public Health. The first chart illustrates the common ground shared by Americans by party affiliation, with vast majorities across parties playing
Having Health Insurance Is A Social Determinant of Health
Health insurance was on the collective minds of American voters in the 2018 midterm elections. Health care, broadly defined, drove many people to the polls voting with feet and ballots to protect their access to a health plan covering a pre-existing condition or to protest the cost of expensive prescription drugs. These were the two top health care issues among voters in late 2018, a Kaiser Family Foundation poll at the time assessed. Yesterday, President Trump verbally re-branded the Republican Party as “the party of healthcare.” That Presidential pronouncement was tied to a letter written on U.S. Department of Justice
Isn’t It Eyeconic? Vision Care in the Evolving Health Care Ecosystem

The vision/optical industry is one piece of the health/care ecosystem, but the segment has not been as directly impacted by patients’ new consumer muscles until just about now. It feels like the vision industry is at an inflection point at this moment, I intuited during yesterday’s convening of Decoding the Consumer: The new science of customer behavior, the theme of the 13th annual global leadership summit hosted by Vision Monday, a program of Jobson Medical Information which is part of the WebMD family. I was grateful to have an opportunity to share my views with attendees on the vision patient as
The Evolution of Self-Care for Consumers – Learning and Sharing at CHPA
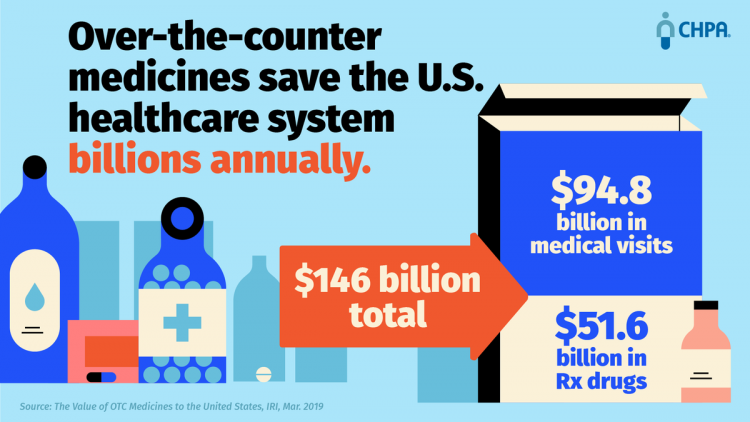
Self-care in health goes back thousands of years. Reading from Hippocrates’ Corpus about food and clean air’s role in health sounds contemporary today. And even in our most cynical moments, we can all hearken back to our grandmothers’ kitchen table wisdom for dealing with skin issues, the flu, and broken hearts. The annual conference of the Consumer Healthcare Products Association (CHPA) convened this week, and I was grateful to attend and speak on the evolving retail health landscape yesterday. Gary Downing, CEO of Clarion Brands and Chairman of the CHPA Board, kicked off the first day with a nostalgic look
Medical Issues Are Still The #1 Contributor to Bankruptcy in the U.S., An AJPH Study Asserts
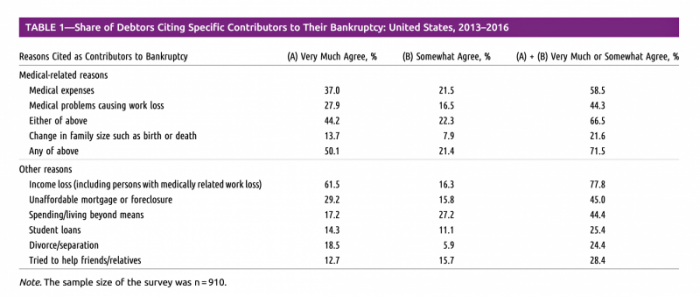
Medical costs in America are still the top contributor to personal bankruptcy in the U.S., a risk factor in two-thirds of bankruptcies filed between 2013 and 2016. That’s a sad fiscal fact, especially as more Americans gained access to health insurance under the Affordable Care Act, according to a study published this month in the American Journal of Public Health (AJPA). Between 2013 and 2016, about 530,000 bankruptcies were filed among U.S. families each year associated with medical reasons, illustrated in Table 1 from the study. The report, Medical Bankruptcy: Still Common Despite the Affordable Care Act, updates research from 2007 which
Patients, Health Consumers, People, Citizens: Who Are We In America?

“Patients as Consumers” is the theme of the Health Affairs issue for March 2019. Research published in this trustworthy health policy publication covers a wide range of perspectives, including the promise of patients’ engagement with data to drive health outcomes, citizen science and participatory research where patients crowdsource cures, the results of financial incentives in value-based plans to drive health care “shopping” and decision making, and ultimately, whether the concept of patients-as-consumers is useful or even appropriate. Health care consumerism is a central focus in my work, and so it’s no surprise that I’ve consumed every bit of this publication. [In
National Health Spending Will Reach Nearly 20% of U.S. GDP By 2027
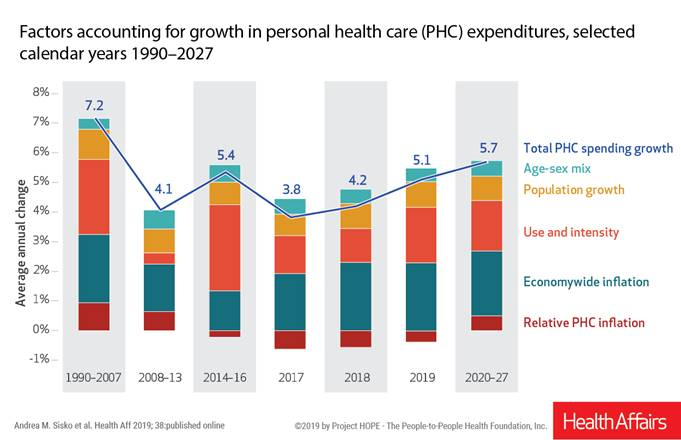
National health spending in the U.S. is expected to grow by 5.7% every year from 2020 to 2027, the actuaries at the Centers for Medicare and Medicaid Services forecast in their report, National Health Expenditure Projections, 2018-2927: Economic And Demographic Trends Drive Spending And Enrollment Growth, published yesterday by Health Affairs. For context, note that general price inflation in the U.S. was 1.6% for the 12 months ending January 2019 according to the U.S. Bureau of Labor Statistics. This growth rate for health care costs exceeds every period measured since the high of 7.2% recorded in 1990-2007. The bar chart illustrates the
Telehealth and Virtual Care Are Melting Into “Just” Health Care at HIMSS19

Just as we experienced “e-business” departments blurring into ecommerce and everyday business processes, so is “telehealth” morphing into, simply, health care delivery as one of many channels and platforms. Telehealth and virtual care are key education topics and exhibitor presences at HIMSS19. Several factors underpin the adoption of telehealth in 2019: Consumers’ demand for accessible, lower-cost health care services as people face greater financial responsibility for paying the medical bill (via high-deductible health plans and greater out-of-pocket costs for co-payments) Some consumers’ lacking or losing health insurance as ACA coverage eroded in the past two years, resulting in these patients
The Cost of Prescription Drugs, Doctors and Patient Access – A View from HIMSS19
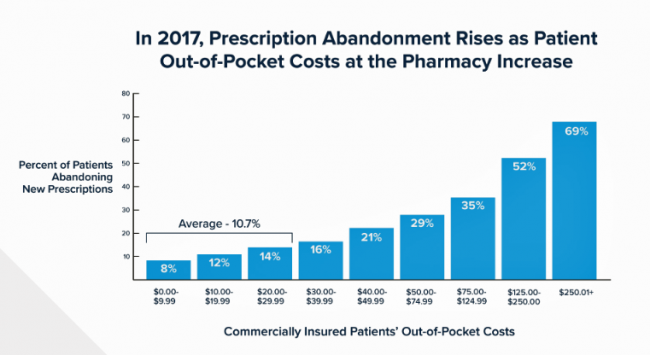
Most patient visits to doctors result in a prescription written for a medicine that people retrieve from a pharmacy, whether retail in the local community or via mail order for a maintenance drug. This one transaction generates a lot of data points, which individually have a lot of importance for the individual patient. Mashed with other patients’, prescription drug utilization data can combine with more data to be used for population health, cost-effectiveness, and other constructive research pursuits. At HIMSS19, there’s an entire day devoted to a Pharma Forum on Tuesday 12 February, focusing on pharma-provider-payor collaborations. Allocating a full
The Consumer and the Payor, Bingo and Trust: My Day At Medecision Liberator Bootcamp

To succeed in the business of health information technology (HIT), a company has to be very clear on the problems it’s trying to address. Now that EHRs are well-adopted in physicians’ practices and hospitals, patient data have gone digital, and can be aggregated and mined for better diagnosis, treatment, and intelligent decision making. There’s surely lots of data to mine. And there are also lots of opportunities to design tools that aren’t very useful for the core problems we need to solve, for the clinicians on the front-lines trying to solve them, and for the patients and people whom we
In U.S. Health Care, It’s Still the Prices, Stupid – But Transparency and Consumer Behavior Aren’t Working As Planned
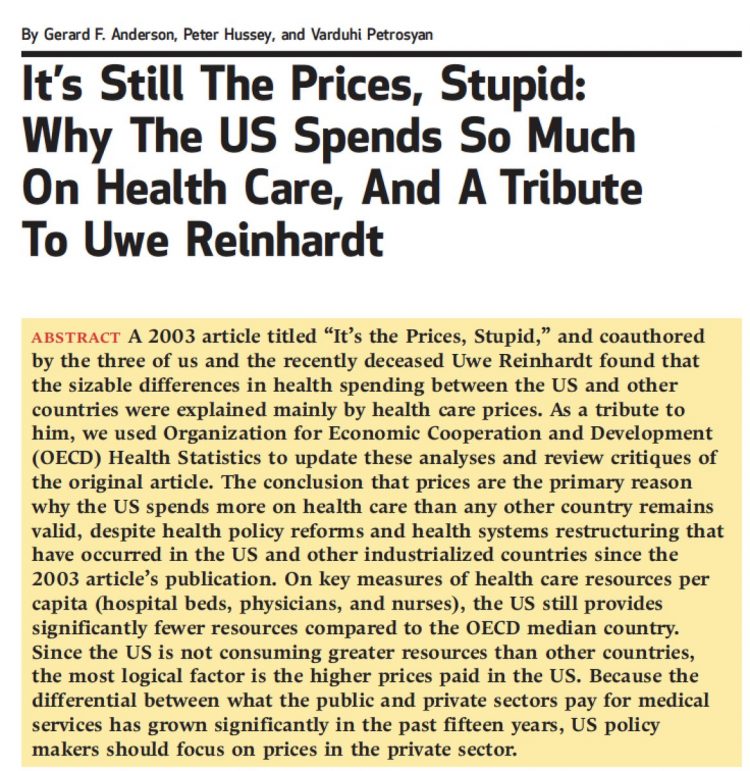
I’m glad to be getting back to health economic issues after spending the last couple of weeks firmly focused on consumers, digital health technologies and CES 2019. There’s a lot for me to address concerning health care costs based on news and research published over the past couple of weeks. We’ll start with the centerpiece that will provide the overall context for this post: that’s the ongoing research of Gerard Anderson and colleagues under the title, It’s Still The Prices, Stupid: Why The US Spends So Much On Health Care, And A Tribute To Uwe Reinhardt. It is bittersweet to
The Caveats for Health/Care at CES 2019

According to the Cambridge Dictionary, a “caveat” is, “a warning to consider something before doing anything more.” It is fitting that CES is held in Las Vegas, land of high risk and, with a lot of luck, reward. With that theme in mind, I depart LAS airport tonight on an aptly-named red-eye flight back home after spending an entire week here. I’m pondering not what I saw — some of which I covered daily over the past week — but what I didn’t see. Consider these the caveats for health/care at #CES2019. In no particular order… Where was the Chairman of
The Consumer as Payor – Retail Health at CES 2019

All health/care is retail now in America. I say this as most people in the U.S. who have health insurance must take on a deductible of some amount, which compels that insured individual to spend the first dollar on medical services up until they meet their financial commitment. At that point, health insurance kicks in, and then the insured may have to spend additional funds on co-payments for general medicines and services, and coinsurance for specialty drugs like injectables and high-cost new therapies. The patient is a consumer is a payor, I asserted today during my talk on the expanding
Heart Health at #CES2019 – Food and Tech as Medicine

Self-care is the new health care as patients, now consumers at greater financial risk for medical spending, are learning. At #CES2019, I’m on the lookout for digital technologies that can help people adopt and sustain healthy behaviors that can help consumers save money on medical care and enhance quality of life-years. This week’s heart-and-food tech announcements at #CES2019 coincide with an FDA recall on a popular drug prescribed to treat hypertension (high blood pressure). Using food and tech as medicine can help people avoid going on medications like statins and others for heart health. An important example of this self-care
Costs, Consumerism, Cyber and Care, Everywhere – The 2019 Health Populi TrendCast

Today is Boxing Day and St. Stephens Day for people who celebrate Christmas, so I share this post as a holiday gift with well-wishes for you and those you love. The tea leaves have been brewing here at THINK-Health as we prepared our 2019 forecast at the convergence of consumers, health, and technology. Here’s our trend-weaving of 4 C’s for 2019: costs, consumerism, cyber and care, everywhere… Health care costs will continue to be a mainstream pocketbook issue for patients and caregivers, with consequences for payors, suppliers and ultimately, policymakers. Legislators inside the DC Beltway will be challenged by the
While National Health Care Spending Growth Slowed in 2017, One Stakeholder’s Financial Burden Grew: The Consumer’s

National health care spending growth slowed in 2017 to the post-recession rate of 3.9%, down from 4.8% in 2016. Per person, spending on health care grew 3.2% to $10,739 in 2017, and the share of GDP spent on medical care held steady at 17.9%. Healthcare spending in America is a $3.5 trillion micro-economy…roughly the size of the entire GDP of Germany, and about $1 trillion greater than the entire economy of France. These annual numbers come out of the annual report from the Centers for Medicare and Medicaid Services, published yesterday in Health Affairs. Underneath these macro-health economic numbers is
Most Americans Want the Federal Government to Ensure Healthcare for All

Most people in the U.S. believe that the Federal government should ensure that their fellow Americans, a new Gallup Poll found. This sentiment has been relatively stable since 2000 except for two big outlying years: a spike of 69% in 2006, and a low-point in 2003 of 42%. In 2006, Medicare Part D launched, which may have boosted consumers’ faith in Federal healthcare programs. In contrast, in 2013 the Affordable Care Act was in implementation and consumer-adoption mode, accompanied by aggressive anti-“Obamacare” campaigns in mass media. That’s the top lighter green line in the first chart. But while there’s majority support
Healthcare Is Local: Channeling Tip O’Neill in the 2018 Midterm Election Results

As Tip O’Neill’s mantra goes, “All politics is local.” In the U.S. 2018 midterm elections, healthcare voting seems to have translated as a local issue, falling into O’Neill’s axiom. In this election, healthcare was the most important voting issue for consumers, PwC found, ranking above the economy, national security, and education. On this morning after 2018 midterm election results are (mostly) out, it looks like healthcare was a local and state issue for U.S. 2018 midterm voters. The Democrats flipped more than 23 seats in the U.S. House of Representatives to gain control of that chamber. The Senate is up
Vote As If Your Health Depended Upon It; Learning from Governor Kasich on Voting Day 2018

…because it does. “Citizens scare politicians,” I heard Governor John Kasich say to Nicole Wallace on her show Deadline: White House yesterday, just hours from today’s U.S. 2018 midterm elections. Governor Kasich has led the Buckeye State since 2011, and his second and final term ends in January 2019. The Governor expanded Medicaid under the Affordable Care Act in the State of Ohio, discussed in this insightful Washington Post article. “I am my brothers’ and sisters’ keeper,” Kasich told Wallace. The Governor asserted this in the context of the role of protecting his fellow citizens for health and well-being, for
Healthcare and the F-Word: Health Politics Rank High on November 6, 2018

“Let’s get this thing f-ing done,” Martha McSally passionately asserted on May 4, 2017. Paul Ryan said, on the floor of the U.S. House of Representatives without cursing, “A lot of us have waited seven years to cast this vote.” McSally, who represents Tucson, Arizona, in the U.S. Congress, is running to replace retiring Senator Jeff Flake. McSally was one of the 217 Republicans in the House who voted to repeal the Affordable Care Act, subsequently celebrating a victory in the Rose Garden of the White House with jubilant peers. The final vote was 217-213. Here’s the final roll call
Consumers Want Help With Health: Can Healthcare Providers Supply That Demand?

Among people who have health insurance, managing the costs of their medical care doesn’t rank as a top frustration. Instead, attending to health and wellbeing, staying true to an exercise regime, maintaining good nutrition, and managing stress top U.S. consumers’ frustrations — above managing the costs of care not covered by insurance. And maintaining good mental health and staying on-track with health goals come close to managing uncovered costs, Oliver Wyman’s 2018 consumer survey learned. These and other important health consumer insights are revealed in the firm’s latest report, Waiting for Consumers – The Oliver Wyman 2018 Consumer Survey of US
Healthcare Costs Stress Out U.S. Voters One Week Ahead of 2018 Mid-Term Elections

With seven days until voters go to the polls for what some call the most momentous U.S. election in decades, most Americans say that healthcare costs are a major stress, second only to money. So warns the Sixth Annual Nationwide TCHS Consumers Healthcare Survey, with the tagline: “Stressed Out: Americans and Healthcare.” Perhaps this is why healthcare has become a top voting issue for the 2018 mid-term elections that will be held on November 6 one week from today. The first chart illustrates that healthcare costs, the economy, and family responsibilities all closely cluster as sources of stress for a
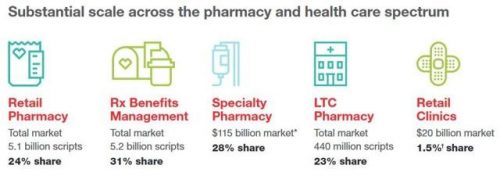
CVS + Aetna: Inflection Point in US Healthcare, Merger Approved Update

CVS Health’s acquisition of Aetna was approved this week by U.S. Federal regulators after months of scrutinizing the antitrust-size-market control implications of the deal. I wrote this post on the deal as an inflection point in American healthcare on 3rd December 2017 when CVS and Aetna announced their marriage intentions. This post updates my initial thoughts on the deal, given the morphing US healthcare market on both the traditional health services front and fast-evolving retail health environment. The nation’s largest retail pharmacy chain signed a deal to combine with one of the top three health insurance companies. The deal
As Workers’ Healthcare Costs Increase, Employers Look to Telehealth and Wearable Tech to Manage Cost & Health Risks
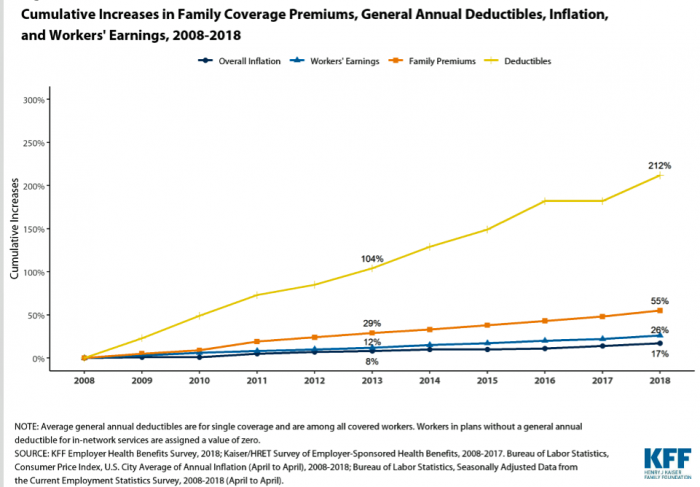
Family premiums for health insurance received at the workplace grew 5% in 2018: to $19,616, according to the 2018 KFF Employer Health Benefits Survey released today by the Kaiser Family Foundation (KFF). These two trends combine for a 212% increase in workers’ deductibles in the past decade. This is about eight times the growth of workers’ wages in the U.S. in the same period. Thus, the main takeaway from the study, KFF President and CEO Drew Altman noted, is that rising health care costs absolutely remain a burden for employers — but a bigger problem for workers in America. Given that
Most U.S. Physicians, Burned Out, Favor A Flavor of Single Payer Health System

Most physicians feel some level of burnout, hassled by electronic health records and lost autonomy. No wonder, then, that a majority of doctors favor some type single payer health system — one-quarter fully single payer, a la Britain’s National Health Service; and another one-third a single payer combined with a private insurance option, discovered in the 2018 Survey of America’s Physicians report on practice patterns & perspectives, published by The Physicians Foundation. Eight in ten physicians are working at full-capacity or are over-extended, the survey found. Furthermore, 62% of doctors are pessimistic about the future of medicine. Physician burnout is a
When Life and Health Insurance Blur: John Hancock, Behavioral Economics, and Wearable Tech

Most consumers look to every industry sector to help them engage with their health. And those companies include the insurance industry and financial services firms, we found in the 2010 Edelman Health Engagement Barometer. John Hancock, which covers about 10 million consumers across a range of products, is changing their business model for life insurance. Here’s the press release, titled, “John Hancock Leaves Traditional Life Insurance Model Behind to Incentivize Longer, Healthier Lives.” “We fundamentally believe life insurers should care about how long and well their customers live. With this decision, we are proud to become the only U.S. life insurance
Consumers Don’t Know What They Don’t Know About Healthcare Costs

The saving rate in the U.S. ranks among the lowest in the world, in a country that rates among the richest nations. So imagine how well Americans save for healthcare? “Consumers are not disciplined about saving in general,” with saving for healthcare lagging behind other types of savings, Alegeus observes in the 2018 Alegeus Consumer Health & Financial Fluency Report. Alegeus surveyed 1,400 U.S. healthcare consumers in September 2017 to gauge peoples’ views on healthcare finances, insurance, and levels of fluency. As patients continue to take on more financial responsibility for healthcare spending in the U.S., they are struggling with finances and
Surprise, Surprise: Most Americans Have Faced a “Surprise” Medical Bill

Most Americans have been surprised by a medical bill, a NORC AmeriSpeak survey found. Who’s responsible? Nearly all Americans (86% net responsible) first blame health insurance companies, followed by hospitals (82%). Fewer U.S. patients blamed doctors and pharmacies, although a majority of consumers still put responsibility for surprise healthcare bills on them (71% and 64% net). Most of the surprise bills were for charges associated with a physician’s service or lab test. Most surprise charges were not due to the service being excluded from a health plans provider network. The poll was conducted among 1,002 U.S. adults 18 and over
Pre-Existing Conditions: A Trans-Party, National Health Priority
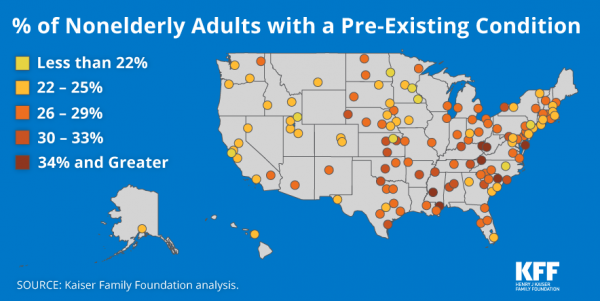
Pre-existing conditions impact Americans north, south, east and west, the Kaiser Family Foundation maps. But those maladies aren’t evenly distributed across the U.S.: the highest incidences of people with pre-existing conditions are generally dotted in the eastern half of the U.S., in diverse metropolitan areas. This study looks at non-elderly adults, people between 18 and 64 years of age. That is, working-age U.S. adults who would be prospects for private health insurance coverage, whether through employers or on the individual insurance market. A striking aspect of this map is that one metro that has a higher rate of people with
More U.S. Companies Offering Health Insurance After 8 Years of Decline
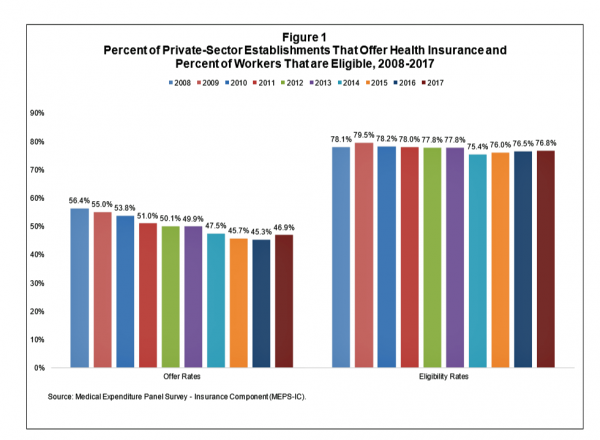
After eight years of decline, more U.S. employers offered health insurance to workers in 2017, EBRI reports in its latest Issue Brief. In 2017, 46.9% of U.S. companies offered health insurance to their employees, up by 1.6 percentage points from a low of 45.3% in 2016. For perspective, ten years earlier in 2008, 56.4% of employers offered health insurance, shown in the first bar chart (Figure 1 from the EBRI report). The largest percentage point increase in health plan offer-rates came from the smallest companies, those with less than 10 employees: while 21.7% of those companies offered health insurance in
Disruption Is Healthcare’s New Normal
Googling the words “disruption” and “healthcare” today yielded 33.8 million responses, starting with “Riding the Disruption Wave in Healthcare” from Bain in Forbes, Accenture’s essay on “Big Bang Disruption in Healthcare,” and, “A Cry for Encouraging Disruption” in the New England Journal of Medicine Catalyst. This last article responded to the question, “Can we successfully deliver better quality care for patients at a lower cost?” asked by François de Brantes, Executive Director of the Health Care Incentives Improvement Institute. “Disruption” as a noun and an elephant in our room has been with us in healthcare since the September/October 2000 issue of
FANGs & MAGA – Meet WaWa for Health, Walgreens and Walmart

While Amazon and Google get lots of positive PR and media attention as major healthcare industry disruptors, don’t forget about two big “W’s,” Walgreens and Walmart, in the healthcare innovator mix. I recently read The Four in which Scott Galloway explains the dominance of Amazon, Apple, Google and Facebook in consumers’ everyday lives. These four tech-behemoths each have their particular designs on healthcare innovation, or disruption in the eyes of, say, Epic and Cerner working on health IT systems, or GE and IBM if you’ve been pioneers in health data or big-iron information technology. Then in the past week, the
Healthcare, and Especially Covering Pre-Existing Conditions, Ranks High for Voters in 2018
President Trump and his administrative have been trying to make the ACA fail, claim most U.S. adults. Thus, the public holds the POTUS and the Republican party responsible for moving the Affordable Care Act forward….or not, according to the July 2018 Kaiser Health Tracking Poll conducted by the Kaiser Family Foundation (KFF). Health care will be a key issue in the 2018 mid-term elections that will be held in November. Among U.S. voters’ key health care concerns in 2018, one ranks “most” or “very important” for two-thirds of Americans: that is continuing to protect people with pre-existing health conditions. Other issues
Healthcare Policies We Can Agree On: Pre-Existing Conditions, Drug Prices, and PillPack – the June 2018 KFF Health Tracking Poll
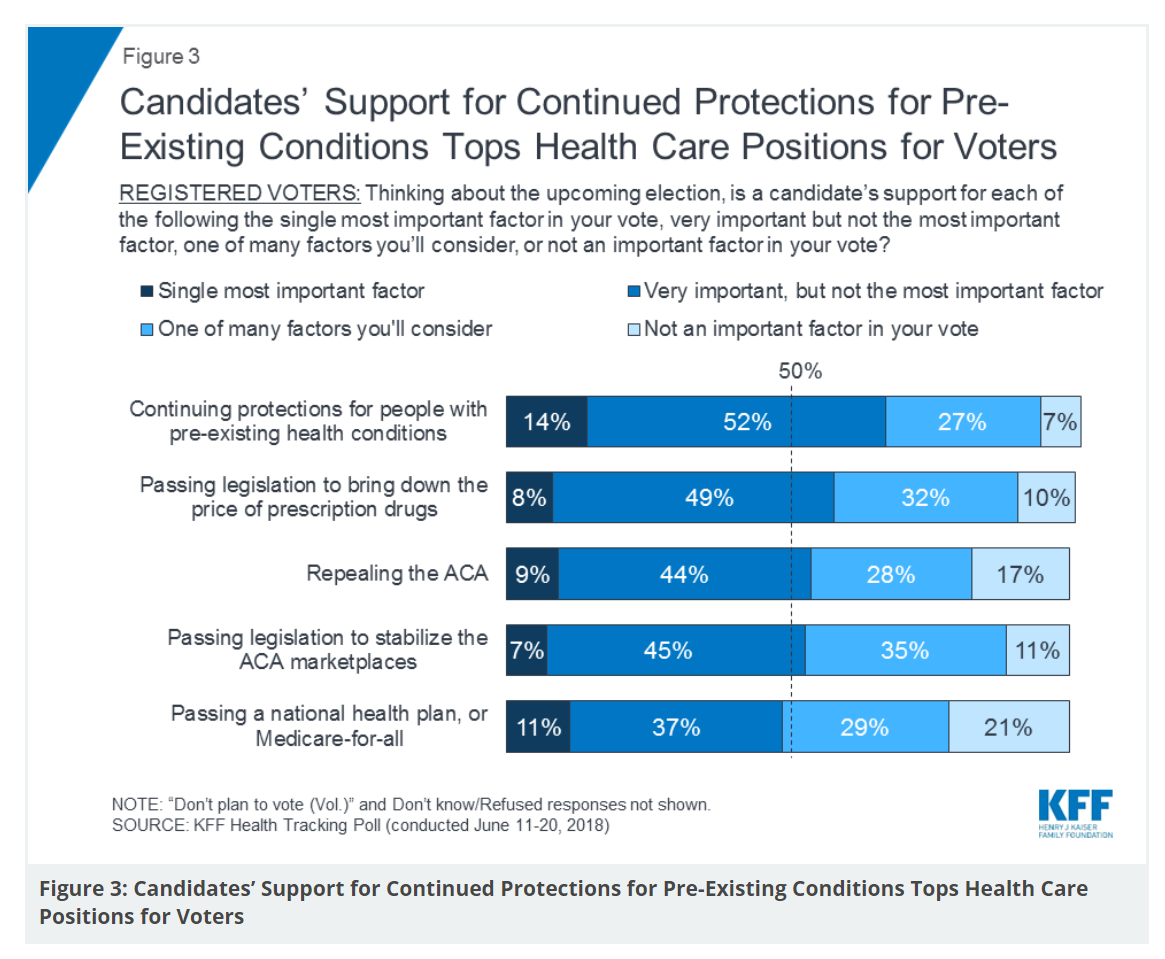
There are countless chasms in the U.S. this moment in social, political, and economic perspectives. but one issue is on the mind of most American voters where there is evidence of some agreements: health care, as evidenced in the June 2018 Health Tracking Poll from Kaiser Family Foundation. Top-line, health care is one of the most important issues that voters want addressed in the 2018 mid-term elections, tied with the economy. Immigration, gun policy, and foreign policy follow. While health care is most important to voters registered as Democrats, Republicans rank it very important. Among various specific health care factors, protecting
Obese, Access-Challenged and Self-Rationing: America’s Health Vs Rest-of-World

The U.S. gets relatively low ROI for its relatively exorbitant spending on healthcare, noted once again in the latest Health at a Glance, the annual OECD report on member nations’ healthcare systems. The report includes U.S. country data asking, “How does the United States compare?” with its sister OECD countries. The answer is, “not well across most population health, access, and mortality measures.” For the Cliff’s Notes/Where’s Waldo top-line of the research, find the two long bars in this chart heading “south” of the OECD average, and one long blue bar going “north.” The northern climbing bar
The True Costs of Diabetes Go Well Beyond the Wallet

The daily life of a person managing diabetes feels many costs: at work, on relationships, at play, during sleep, on time, on mental health, and to be sure, on personal finances. The True Cost of Diabetes report from Upwell details the many tolls on the person with diabetes. The first-order impact for a patient engaging in self-care to manage diabetes is time that the many tasks in a day borrow from work, sleep, home-keeping, and relationships. Seventy percent of PwD (people with diabetes) checks blood sugar at least once a day (41% one to two times, 29% three to five
It Could Take Five Generations for a Low-Income US Family to Reach Average Income in America

Social mobility in America has a lot of friction: children of wealthier people tend to grow into affluence, and children of low-income parents tend to struggle to move up the income and education ladder, according to A Broken Social Elevator: How to Promote Social Mobility, a new report from the OECD. The Organization for Economic Cooperation and Development studied member nations’ economies, demographics, income and opportunities to gauge each country’s social mobility. Social mobility, the OECD explains, is multi-faceted. It can refer to inter-generational mobility between parents, children, and grandchildren. Alternatively, social mobility can look at intra-generational mobility, over the course
As Medical Cost Trend Remains Flat, Patients Face Growing Health Consumer Financial Stress

When it comes to healthcare costs, lines that decline over time are generally seen as good news. That’s how media outlets will cover the top-line of PwC’s report Medical cost trend: Behind the numbers 2019. However, there are other forces underneath the stable-looking 6.0% medical trend growth projected for 2019 that will impact healthcare providers, insurers, and suppliers to the industry. There’s this macro-health economic story, and then there’s the micro-economics of healthcare for the household. Simply put: the impact of growing financial risk for healthcare costs will be felt by patients/consumers themselves. I’ve curated the four charts from the
Doing Less Can Be Doing More for Healthcare – the Biggest Takeaway From ASCO 2018

Less can lead to more for so many things: eating smaller portions, lowering sugar consumption, and driving less in favor of walking or cycling come to mind. When it comes to healthcare utilization, doing less can also result in equal or even better outcomes. Groundbreaking research presented at this week’s ASCO meeting found that some women diagnosed with certain forms of cancer do not benefit from undergoing chemotherapy. The American Society of Clinical Oncology (ASCO) is one of the largest medical meetings annually, and at this huge meeting these research results for the TAILORx trial were huge news with big
Personalized Medicine: Consumer Concerns About Coverage, Affordability and Privacy
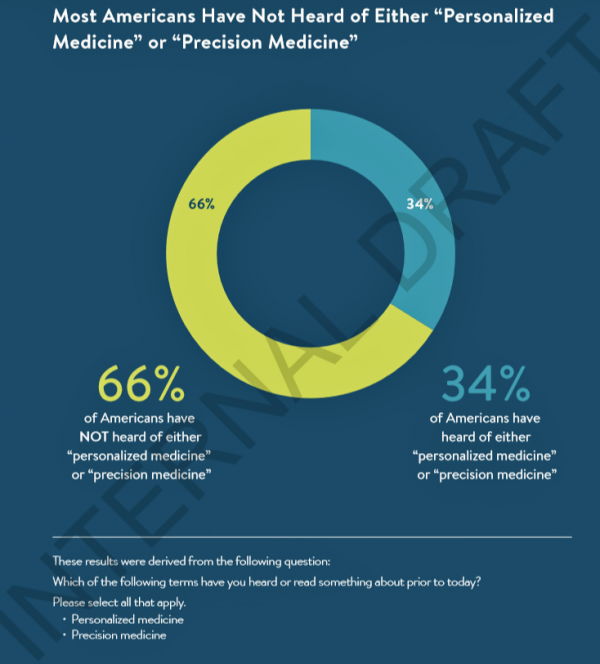
Two in 3 Americans haven’t heard the phrases “personalized medicine” or “precision medicine.” When the concept of therapies tailored to individual patients is explained, most people like the idea of diagnostic tools that can identify biological markers and marry to personal medical records data to help determine medical treatments that best fit them. This picture of U.S. consumers’ views on personalized medicine comes from a survey conducted for PMC, the Personalized Medicine Coalition, and GenomeWeb, published in May 2018. The poll results are published in Public Perspectives on Personalized Medicine, with the top-line finding that life science industry innovators must
Health Care for a Typical Working Family of Four in America Will Cost $28,166 in 2018
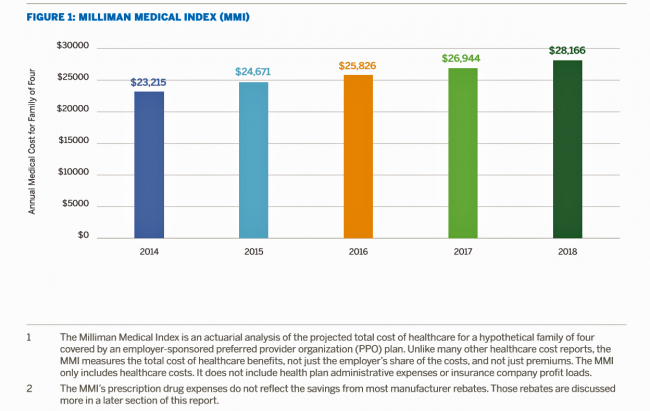
What could $28,166 buy you in 2018? A new car? A year of your child’s college education? A plot of land for your retirement home? Or a year of healthcare for a family of four? Welcome to this year’s edition of the Milliman Medical Index (MMI), one of the most important forecasts of the year in the world of the Health Populi blog and THINK-Health universe. That’s because we’re in the business of thinking about the future of health and health care through the health economics lens; the MMI is a key component of our ongoing environmental analysis of the
A Tale of Two America’s for Health
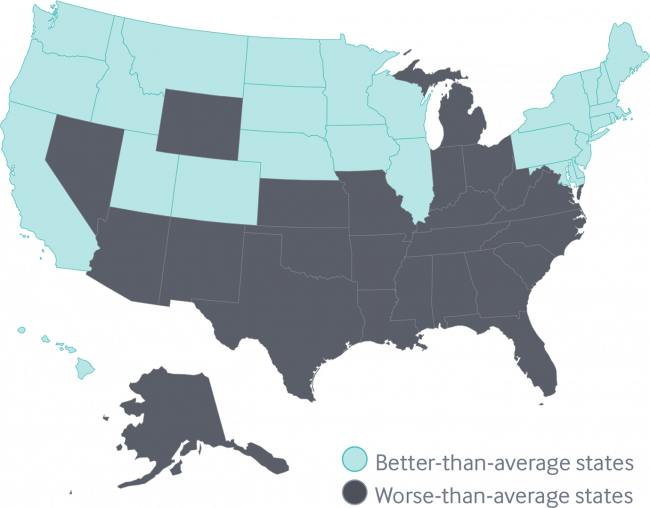
Disparities in Americans’ health vary among people living in each of the 50 states. These differences in health status generally fall into two regions: north and south, found in the Commonwealth Fund’s 2018 Scorecard on State Health System Performance. The map shows this stark geography-is-health-destiny reality: the worse-than-average states, the Fund found, run from Nevada southeast to Arizona, through New Mexico and Texas all the way to Atlantic Ocean and the Carolinas, then north west all the way up through the industrial Midwest states through Michigan to the north. Wyoming is the only non-contiguous state in the worse-performing U.S. state
The Gap Between the Trump Administration’s Promise of Reducing Rx Costs for Consumers and What People Really Want
This is what happened to pharma stock prices on Friday after President Trump and Secretary of Health and Human Services Alex Azar outlined their new policies focusing on prescription drug prices. The graph is the Nasdaq U.S. Smart Pharmaceuticals Index (NQSSPH) from May 11, 2018, the date when POTUS and Secretary Azar made their announcement. What this upward driving curve indicates, from the start of stock trading in the morning until the ring of the closing bell, is that the pharma industry players, both manufacturers and PBMs, were quite delighted with what they heard. The blueprint for restructuring the prescription drug industry,
Guns, Jobs, or Health Care? In 2018, Voters Split as to Top Issue
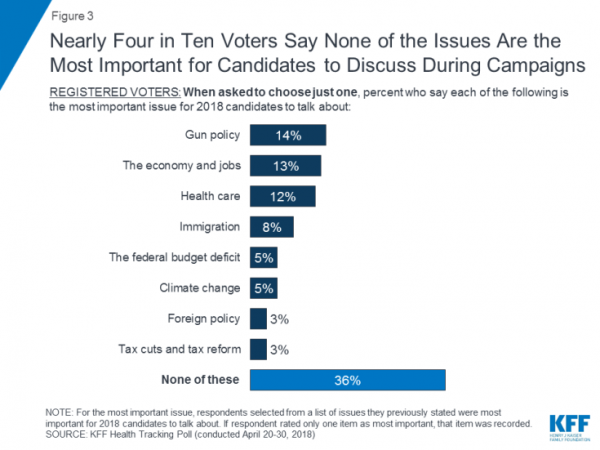
It’s a fairly even split between voting first on gun policy, jobs, or healthcare for the 2018 mid-term elections, ac cording to the May 2018 Kaiser Family Foundation Health Tracking Poll. Arguably, gun policy can cut in two ways: in light of the Stoneman Douglas High School shootings and wake-up call for #NeverAgain among both students and the public-at-large, vis-a-vis Second Amendment issue voters. And, as a growing public health issue, “guns” could also be adjacent to health. “If it isn’t a health problem, then why are all these people dying from it?” rhetorically asked Dr. Garen Wintemute, professor of emergency
Having Health Insurance Is a Social Determinant of Health: the implications of growing uninsured in the U.S.
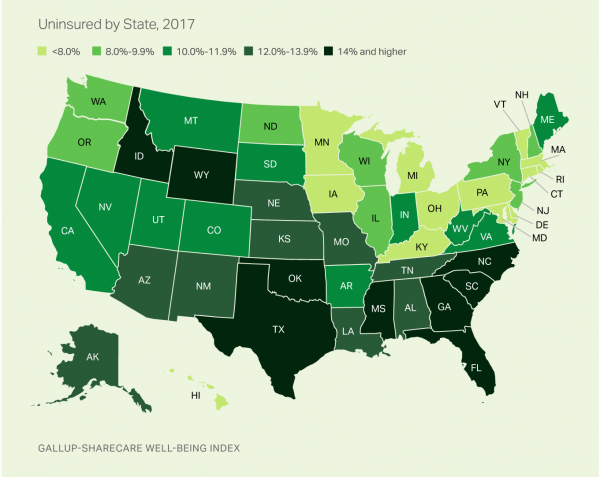
The rolls of the uninsured are growing in America, the latest Gallup-Sharecare Poll indicates. The U.S. uninsurance rate rose to 12.2% by the fourth quarter of 2017, up 1.3 percentage points from the year before. 2017 reversed advancements in health insurance coverage increases since the advent of the Affordable Care Act, and for the first time since 2014 no states’ uninsured rates fell. The 17 states with declines in insurance rates were Arizona, Colorado, Florida, Hawaii, Illinois, Indiana, Iowa, Missouri, New Mexico, New York, North Carolina, South Carolina, Texas, Utah, Washington, West Virginia, Wisconsin, and Wyoming. Among these, the greatest
Universal Health Care and Financial Inclusion – Two Sides of the Wellness Coin

Two weeks in a row, The Economist, the news magazine headquartered in London, included two special reports stapled into the middle of the magazines. Universal health care was covered in a section on 28 April 2018, and coverage on financial inclusion was bundled into the 5th May edition. While The Economist’s editors may not have intended for these two reports to reinforce each other, my lens on health and healthcare immediately, and appreciatively, connected the dots between healthcare coverage and financial wellness. The Economist, not known for left-leaning political tendencies whatsoever, lays its bias down on the cover of the section here: universal healthcare
Americans’ Trust in the Healthcare System Low Compared to Rest-of-World’s Health Citizens
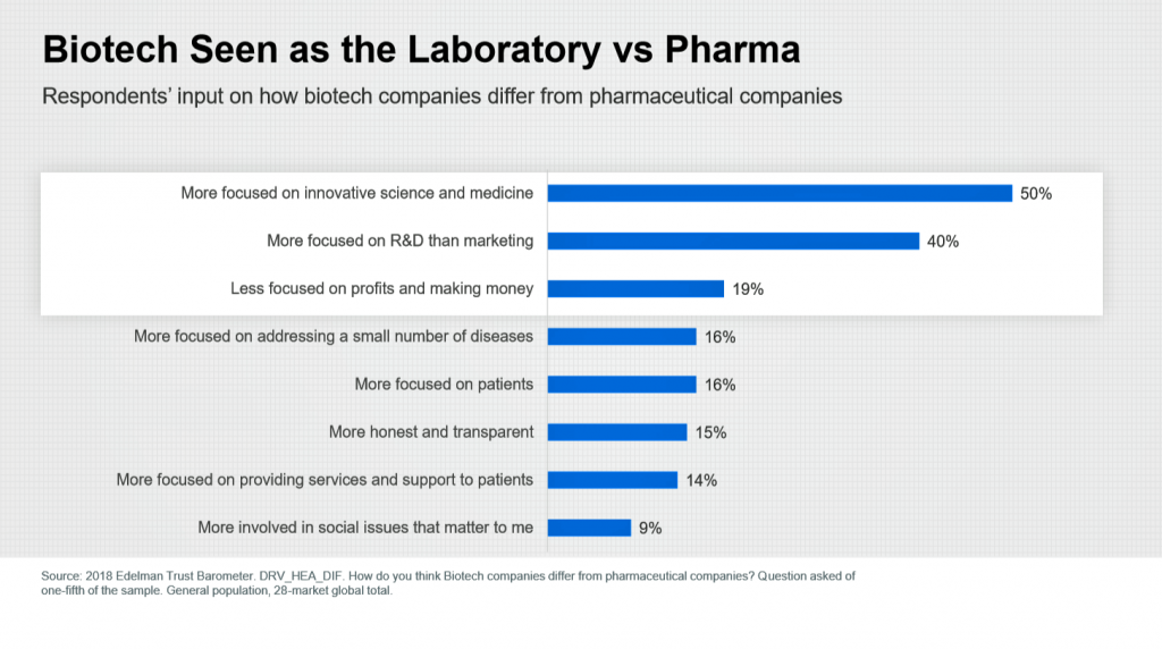
In the U.S., trust in the healthcare industry declined by 9 percentage points in just one year, declining from 62% of people trusting — that’s roughly two-thirds of Americans — down to 53% — closer to one-half of the population. I covered the launch of the 2018 Edelman Trust Barometer across all industries here in Health Populi in January 2018, when this year’s annual report was presented at the World Economic Forum in Davos as it is each year. The Edelman team shared this detailed data on the healthcare sector with me this week, for which I am grateful. Check
How Walmart Could Bolster Healthcare in the Community

Walmart has been a health/care destination for many years. The company that defined Big Box stores in their infancy grew in healthcare, health and wellness over the past two decades, pioneering the $4 generic prescription back in 2006. Today, that low-cost generic Rx is ubiquitous in the retail pharmacy. A decade later, can Walmart re-imagine primary care the way the company did low-cost medicines? Walmart is enhancing about 500 of 3500 stores, and health will be part of the interior redecorating. Walmart has had ambitious plans in healthcare since those $4 Rx’s were introduced. Here’s a New York Times article from
The Health of A Nation – Being Healthy In America Depends on Where You Live

In the US, when it comes to life and death, it’s good to live in Hawaii, Utah, Minnesota, North Dakota, and Iowa — the top five states with the greatest life expectancy and healthy life expectancy at birth in 2016. For health and longevity, sorry to see the lowest five ranked states are Washington DC which ranks last, along with Mississippi, Louisiana, South Carolina, and Alabama. This sober geography-is-health-destiny update was published this week in JAMA, The State of US Health, 1990-2016: Burden of Diseases, Injuries, and Risk Factors Among US States. The first chart illustrates states down the left
Livongo and Cambia Allying to Address Chronic Disease Burden and Scale Solutions to Consumers

Chronic diseases are what kill most people in the world. In the U.S., the chronic disease burden takes a massive toll on both public health and mortality, accounting for 7 in 10 deaths in America each year. That personal health toll comes at a high price and proportion of national health expenditures. A new alliance between Livongo and Cambia Health seeks to address that challenge, beginning with diabetes and scaling to other chronic conditions. Livongo has proven out the Livongo for Diabetes program, which has demonstrated positive outcomes in terms of patient satisfaction and cost-savings. The plan with Cambia is
What Would Healthcare Feel Like If It Acted Like Supermarkets – the 2018 Temkin Experience Ratings
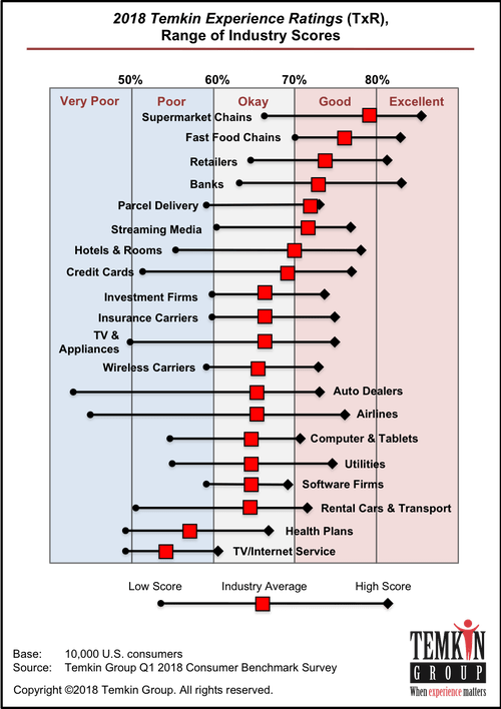
U.S. consumers rank supermarkets, fast food chains, retailers, and banks as their top performing industries for experience according to the 2018 Temkin Experience Ratings. Peoples’ experience with health plans rank at the bottom of the roster, on par with rental cars and TV/Internet service providers. If there is any good news for health plans in this year’s Temkin Experience Ratings compared to the 2017 results, it’s at the margin of “very poor” performance: last year, health plans has the worst performance of any industry (with the bar to the furthest point on the left as “low scoring”). This year, it
Please Stop Hating on Amazon, Mr. President. It’s Americans’ Favorite Brand.
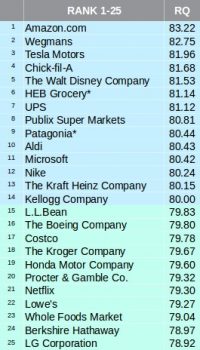
The most beloved company in America is Amazon, according to the 2018 Harris Poll Reputation Quotient Rankings which were published on 22nd March 2018. This was the third year in a row that Amazon garnered the top position in this corporate reputation poll, which gauges consumers’ views on workplace environment, social responsibility, emotional appeal, financial performance, vision and leadership, and products and services. Mr. President, why pick on Americans’ favorite brand? The brand defines the 2018 consumer’s benchmark for a best-retail experience, which is what people increasingly expect across the various interactions they have throughout a day. [As a sidebar,
The New Financial Toxicity in Health Care: The Cost of Hospitalization
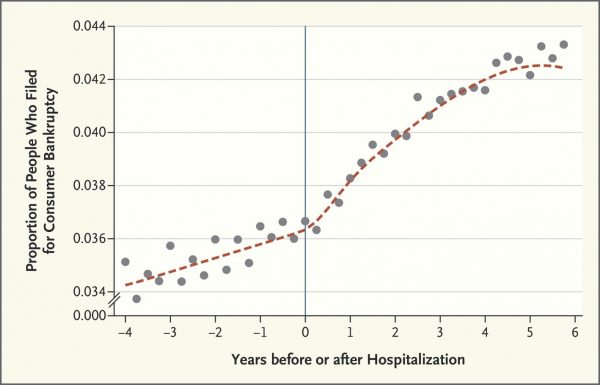
In healthcare, we use the word “toxicity” when it comes to taking a new medicine, especially a strong therapy to cure cancer. That prescription may be toxic as a harmful side effect on our journey to getting well. The concept of “financial toxicity” for cancer patients was raised by concerned clinicians at Sloane-Kettering Medical Center, who discussed the topic on 60 Minutes in 2014 and have published papers on the issue. Beyond strong medicines, a new financial toxicity has emerged for patients due to hospital inpatient admissions. A new article in the New England Journal of Medicine studies Myth and
How We Spend Versus What We Get: America’s Healthcare Spending Makes for Poor Health
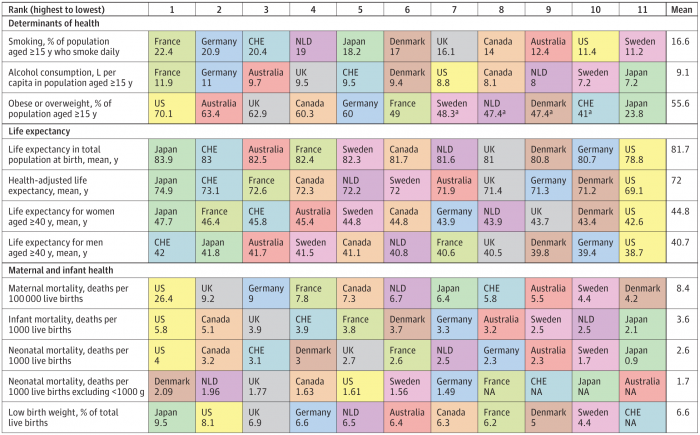
The U.S. spent nearly twice as much as other wealthy countries on healthcare, mostly due to higher prices for both labor and products (especially prescription drugs). And, America spends more on administrative costs compared to other high-income countries. What do U.S. taxpayers get in return for that spending? Lower life spans, higher maternal and infant mortality, and the highest level of obesity and overweight among our OECD peer nations. These sobering statistics were published in Health Care Spending in the United States and Other High-Income Countries this week in JAMA, the Journal of the American Medical Association. The study analyzes
Tweets at Lunch with Paul Krugman – Health IT Meets Economics

I greatly appreciated the opportunity today to attend a luncheon at the HX360 meeting which convened as part of the 2018 HIMSS Conference. The speaker at this event was Paul Krugman, who won the Nobel Prize for Economics 10 years ago and today is an iconic op-ed columnist at the New York Times And Distinguished Professor of Economics at the City University of New York (CUNY). I admit to being a bit of a groupie for Paul Krugman’s work. It tickles me to look at Rise Global’s list of the Top 100 Influential Economists:
Majority Rules? The Right to Affordable Health Care is A Right for All Americans
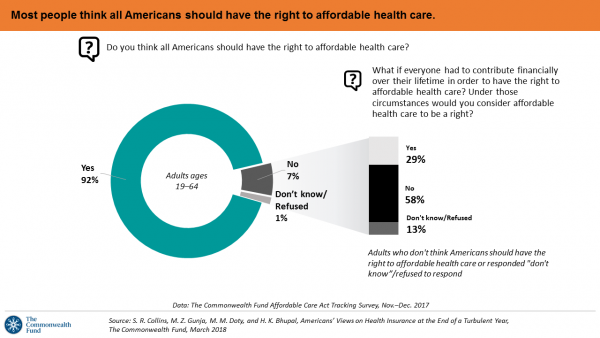
If we’re playing a game of “majority rules,” then everyone in America would have the right to affordable health care, according to a new poll from The Commonwealth Fund. The report is aptly titled, Americans’ Views on Health Insurance at the End of a Turbulent Year. The Fund surveyed 2,410 U.S. adults, age 19 to 64, by phone in November and December 2017. This is the sixth survey conducted by the Fund to track Americans’ views of the Affordable Care Act; the first survey was fielded in mid-to-fall 2013. 9 in 10 working-age adults say “yes” indeed, my fellow Americans
Add Behavioral Data to Social Determinants For Better Patient Understanding
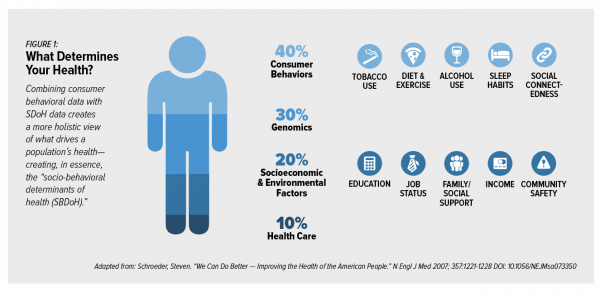
“Health agencies will have to become at least as sophisticated as other consumer/retail industries in analyzing a variety of data that helps uncover root causes of human behavior,” Gartner recommended in 2017. That’s because “health” is not all pre-determined by our parent-given genetics. Health is determined by many factors in our own hands, and in forces around us: physical environment, built environment, and public policy. These are the social determinants of health, but knowing them even for the N of 1 patient isn’t quite enough to help the healthcare industry move the needle on outcomes and costs. We need to
More Working Americans Enrolled in High-Deductible Health Plans in 2017
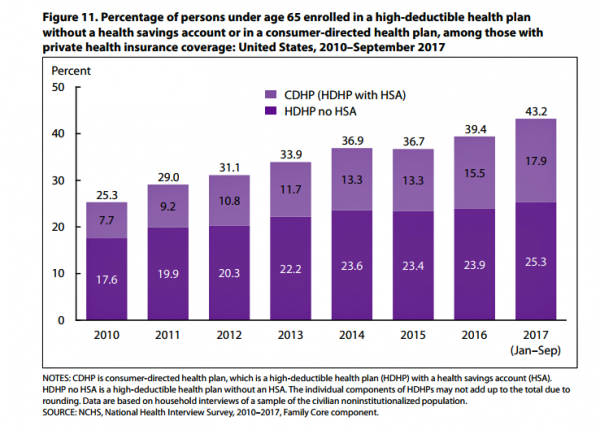
Over four in 10 U.S. workers were enrolled in a high-deductible health plan in the first 9 months of 2017, according to the latest research published by the National Center for Health Statistics, part of the Centers for Disease Control in the U.S. Department of Health and Human Services. The report details Health Insurance Coverage: Early Release of Estimates From the National Health Interview Survey, January-September 2017. About 28 million people were uninsured in the U.S. in 2017, about the same proportion as in 2016 — but nearly 20 million fewer than in 2010, as the line chart illustrates. The
The United States of Care Launches to Promote Healthcare for All of US

Let’s change the conversation and put healthcare over politics. Sounds just right, doesn’t it? If you’re reading Health Populi, then you’re keen on health policy, health economics, most of all, patients: now playing starring roles as consumers, caregivers, and payors in their own care. Andy Slavitt, former Acting Administrator of the Centers for Medicare and Medicaid Services (CMS), has assembled a diverse group of health care leaders who care about those patients/people, too, appropriately named the United States of Care. Founders include Dr. Bill Frist, former Republican U.S. Senator from Tennessee, Dave Durenberger, former Republican U.S. Senator from Minnesota, and
U.S. Workers Say Health Care is the Most Critical Issue Facing the Nation
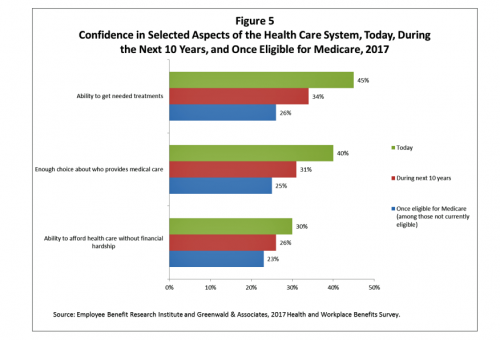
Health care ranks highest among working Americans as the top critical issue facing the country, well above terrorism, the role of the Federal government, unemployment and jobs, education, immigration and taxes. Over half of American workers also rate the country’s healthcare system as “poor” or “fair,” based on the results of the EBRI/Greenwald & Associates Health and Workplace Benefits Survey. Workers dissatisfaction with U.S. healthcare is based largely on cost: one-half of workers experienced an increase in health care costs in the past year. Furthermore, only 22% are satisfied with the cost of their health insurance plan, 18% are satisfied
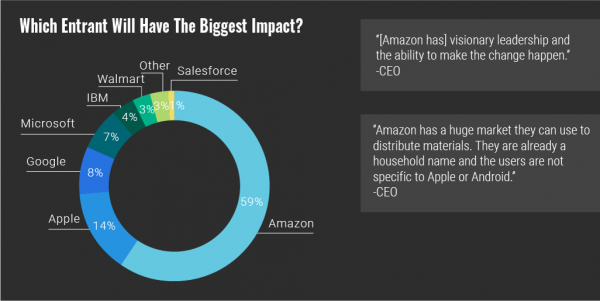
Warren Buffett’s Healthcare Cost Tapeworm & His Alliance with Amazon and JPMorgan

The fact that the average U.S. employer committed to spend nearly $27,000 a year for a PPO to cover a family of 4 in America in 2017 is the most important rationale underlying the announcement that Amazon, Berkshire-Hathaway, and JP Morgan made on 30th January 2017. That news immediately shook Wall Street trading, sending downward shocks down the proverbial spines of healthcare insurance plans and suppliers to the industry — legacy healthcare companies that scale patient-members and healthcare supplies, like pills and surgical implants. The “new competition” chart published in the Wall Street Journal in the morning illustrates those shock
The 2018 Edelman Trust Barometer – What It Means for Health/Care in America

Trust in the United States has declined to its lowest level since the Edelman Trust Barometer has conducted its annual survey among U.S. adults. Welcome to America in Crisis, as Edelman brands Brand USA in 2018. In the 2018 Edelman Trust Barometer, across the 28 nations polled, trust among the “informed public” in the U.S. “plunged,” as Edelman describes it, by 23 points to 45. The Trust Index in America is now #28 of 28 countries surveyed (that is, rock bottom), dropping below Russia and South Africa. “The public’s confidence in the traditional structures of American leadership is now fully
Health Insurance Costs Stress US Whether We’re Rich or Not / and Why a $0 Budget for CFPB Matters for Healthcare

Health care costs cause anxiety for U.S. adults, regardless of their affluence, we learn in Uncertainty About Healthcare, the latest Stress in America poll from the American Psychological Association. The big stat is that 2 in 3 Americans say the cost of health insurance is a stressor for them or their loved ones, whether the person earns more or less than $50,000 a year. Underneath that top-line are some demographic differences. Millennials are most concerned about access to mental health care compared with Boomers and older adults. Reproductive care access is of most interest to Millennials and Gen Xers. Two-thirds
In the U.S., Spend More, Get Less Health Care: the Latest HCCI Data

Picture this scenario: you, the consumer, take a dollar and spend it, and you get 90 cents back. In what industry is that happening? Here’s the financial state of healthcare in America, explained in the 2016 Health Care Cost and Utilization Report from the Health Care Cost Institute (HCCI). We live in an era of Amazon-Primed consumers, digital couponing, and expectations of free news in front of paywalls. We are all in search of value, even as the U.S. economy continues to recover on a macroeconomic basis. But that hasn’t yet translated to many peoples’ home economics. In this personal
Healthcare EveryWhere: Philips and American Well Streamline Telehealth

Two mature companies in their respective healthcare spaces came together earlier this month to extend healthcare services where patients live and doctors work, via telehealth services. Philips, celebrating 127 years in business this year, has gone all-in on digital health across the continuum of care, from prevention and healthy living to the ICU and hospital emergency department. American Well is among the longest operating telehealth companies, founded in 2006. Together, these two established organizations will transcend physician offices and ERs and deliver virtual care in and beyond the U.S. I had the opportunity to sit down with Ido Schoenberg, MD,
Most Americans Say Healthcare is #1 Policy Issue Entering 2018

Concerns about health care are, by a large margin, the top domestic policy issue U.S. voters identified as they enter 2018. The proportion of Americans citing healthcare as the top public agenda priority grew by 50% since 2016, from 31% two years ago to 48%. Taxes rank #2 this year, garnering 31% of Americans’ concerned, followed by immigration, which has remained flat cited by about one-in-four Americans. The Associated Press (AP)-NORC Center for Public Affairs Research polled 1,444 U.S. adults 18 and over between November 30 and December 4, 2017 for this survey. While one-half of Americans would like the
Health Consumers Face the New Year Concerned About Costs, Security and Caring – Health Populi’s 2018 Forecast
As 2018 approaches, consumers will gather healthy New Year’s Resolutions together. Entering the New Year, most Americans are also dealing with concerns about healthcare costs, cybersecurity, and caring – for physical health, mental stress, and the nation. Healthcare costs continue to be top-of-mind for consumer pocketbook issues. Entrenched frugality is the new consumer ethos. While the economy might be statistically improving, American consumers’ haven’t regained confidence. In 2018, frugality will impact how people look at healthcare costs. 88% of US consumers are likely to consider cost when selecting a healthcare provider, a Conduent survey found. Physicians know this: 81% of
Patients Continue to Grow Healthcare Consumer Muscles, Alegeus’s 2017 Index Finds
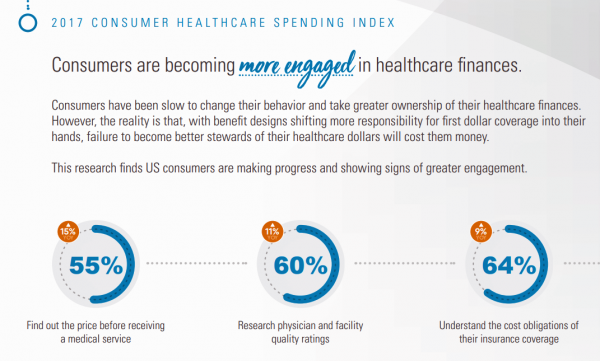
Patients’ health consumer muscles continue to get a work out as more people enroll in high-deductible health plans and face sticker shock for health insurance premiums, prescription drug costs, and that thousand-dollar threshold. The 2017 Alegeus Healthcare Consumerism Index finds growth in patients’, now consumers’, interest and competence in becoming disciplined about planning, saving, and spending for healthcare. Overall, the healthcare spending index hit 60.1 in 2017, up from 54.4 in 2016. This is a macro benchmark that represents most consumers exhibiting greater healthcare spending engagement with eyes on cost as well as adopting purchasing behaviors for healthcare. Underneath that
The Patient as Payor – Consumers and the Government Bear the Largest Share of Healthcare Spending in America
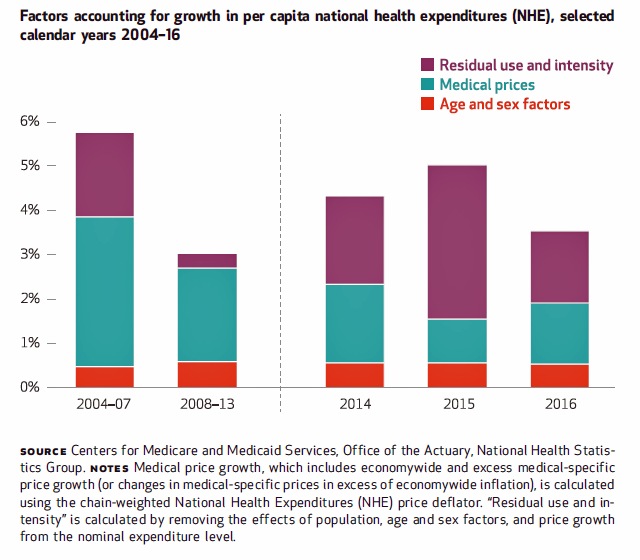
The biggest healthcare spenders in the United States are households and the Federal government, each responsible for paying 28% of the $3.3 trillion spent in 2016. Private business — that is, employers covering healthcare insurance — paid for 20% of healthcare costs in 2016, based on calculations from the CMS Office of the Actuary’s report on 2016 National Health Expenditures. The positive spin on this report is that overall national health spending grew at a slower rate in 2016, at 4.3% after 5.8% growth in 2015. This was due to a decline in the growth rates for the use of
Six Healthcare News Stories to Keep Hospital CFOs Up At Night
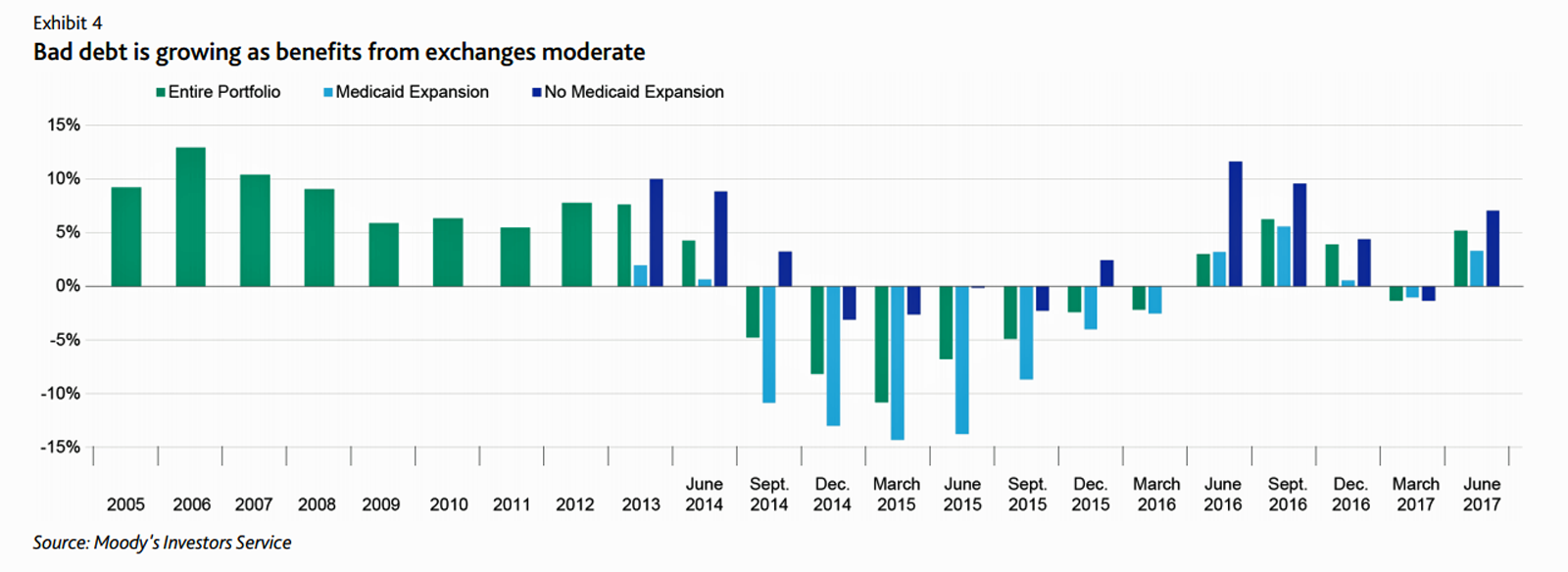
At this moment, the healthcare job I’d least like to have is that of a non-profit hospital Chief Financial Officer (CFO). Five news stories, published in the past 24 hours, tell the tale: First, Moody’s forecast for non-profit hospitals and healthcare in 2018 is negative due to reimbursement and expense pressures. The investors report cited an expected contraction in cash flow, lower reimbursement rates, and rising expense pressures in the midst of rising bad debt. Second, three-quarters of Federally Qualified Health Centers plan to lay off staff given lack of budget allocations resulting from Congressional inaction. Furthermore, if the $3.6
CVS + Aetna: An Inflection Point for American Healthcare

The nation’s largest retail pharmacy chain signed a deal to combine with one of the top three health insurance companies. The deal is valued at $69 billion. I wrote about this inflection point for U.S. healthcare four weeks ago here in Health Populi. CVS is both the biggest pharmacy and pharmacy benefit manager in the U.S., as the first chart shows. In my previous post, I talked about the value of vertical integration bringing together the building blocks of retail pharmacy and pharmacist care, retail clinics, the PBM (Caremark), along with Aetna’s health plan member base and business. As Amazon and other
U.S. Healthcare Spending & Outcomes in Five Charts: #EpicFail in the 2017 OECD Statistics
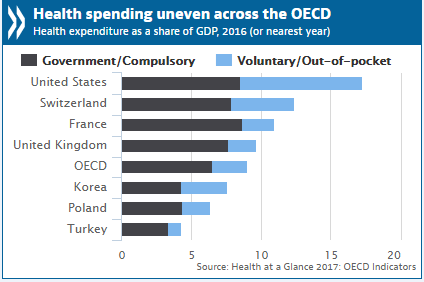
“Spend more. Get less.” If a retailer advertised using these four words, how many consumers would buy that product or service? This is the American reality of healthcare spending in 2016, told in the OECD report, Health at a Glance 2017. I present five charts from the study in this post, which together take the current snapshot health-economic lesson for the U.S. First, look at health expenditures as a share of gross domestic product: the U.S. is number one above Switzerland, France, and the UK, and about two times the OECD average. Note, too, the proportion of out-of-pocket and so-called
Health Care Is 2.5 More Expensive Than Food for the Average U.S. Family
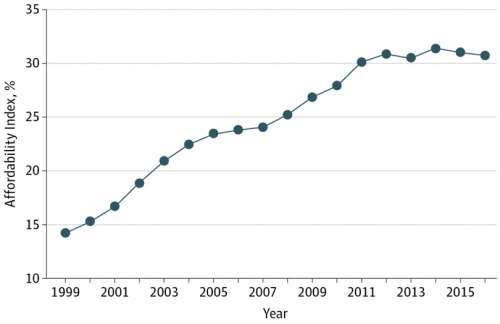
The math is straightforward. Assume “A” equals $59.039, the median household income in 2016. Assume “B” is $18,142, the mean employer-sponsored family insurance premium last year. B divided by A equals 30.7%, which is the percent of the average U.S. family’s income represented by the premium cost of health insurance. Compare that to what American households spent on food: just over $7,000, including groceries and eating out (which is garnering a larger share of U.S. eating opportunities, a topic for another post). Thus, health care represents, via the home’s health insurance premium, represents 2.5 times more than food for the
A Health Consumer Perspective on CVS+Aetna
A response to Amazon’s potential moves in healthcare and pharmacy…strategic positioning for the post-Trump healthcare landscape…vertical integration to better manage healthcare utilization and costs…these, and other rationale have been offered by industry analysts and observers of the discussions between CVS and Aetna, for the former to acquire the latter. “A pharmacy chain buying a health insurance company?” many have asked me over the past few days. These inquiring minds include people who work both inside and outside of health/care. I ask back: in 2017 and in the future, “What is a pharmacy? What is a health plan?” See the
CVS Health in Talks to Acquire Aetna – The Changing Retail Health Landscape

Just a few days since CVS Health announced the company would be working with mega-health insurer Anthem on a prescription drug management program, the pharmacy chain today is reportedly in talks to buy Aetna, the national health insurance company, according to CNBC and other credible news outlets like the Wall Street Journal. Remember that Aetna’s bid to acquire Humana was scuttled earlier this year after many months of negotiation and positioning, along with FTC scrutiny about antitrust. That insurance merger “died” on one day in February 2017 along with an Anthem-CIGNA deal, covered here by CNN. A deal between CVS
Most Americans Are Concerned About Healthcare Policy, and Costs Top the List of Concerns
4 in 5 Americans are aware of potential changes to healthcare policy brewing in Washington, DC. 92% of them are concerned about those changes, according to Healthcare Consumers in a Time of Uncertainty, the fifth annual survey from Transamerica Center for Health Studies. Peoples’ most-shared fears are losing their coverage for pre-existing conditions, out-of-pocket spending, and a ban on lifetime limits. That boils down to one thing: cost. That is, cost, for having to spend money on services not-covered by their health insurance plan; cost for out-of-pocket items under-insured, denied, or requiring coinsurance or co-payments; and, catastrophic costs that rise beyond
What Health Plans Must Learn from Amazon
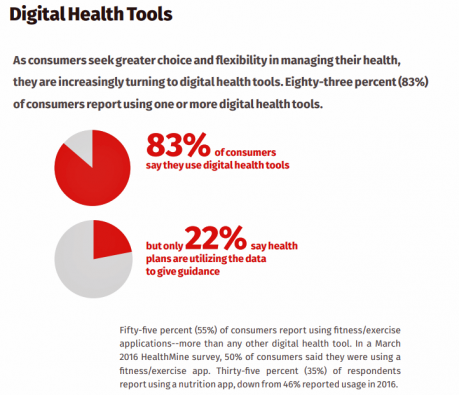
One in two U.S. consumers told Aflac that enrolling in health insurance should feel like an experience on Amazon. But health consumers still lack that high benchmark retail experience with health plans, based on new research published in HealthMine’s 2017 Health Intelligence Report focusing on communication and digital healthcare tools. “Most members believe health plan communications are impersonal and centered around bills rather than healthcare guidance,” HealthMine asserts in the introduction to the report. That’s about as un-Amazon as we can imagine. Top findings from HealthMine’s research are that: 3 in 4 consumers don’t think their health insurance plan
What Patients Feel About Technology, Healthcare Costs and Social Determinants
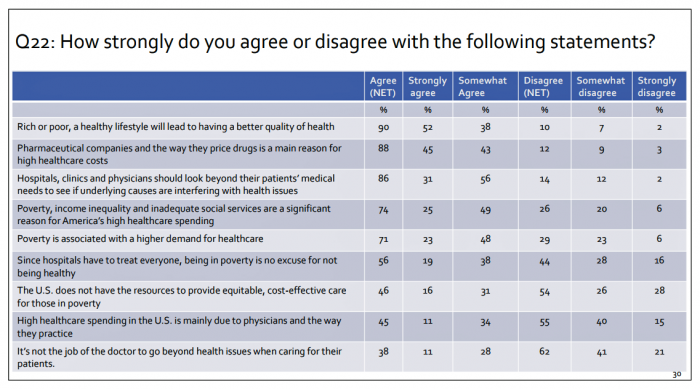
U.S. consumers feel positive about the roles of technology and social determinants in improving healthcare, but are concerned about costs, according to the 2017 Patient Survey Report conducted for The Physicians Foundation. The survey gauged patients’ perspectives across four issues: the physician-patient relationship, the cost of healthcare, social determinants of health, and lifestyle choices. Two key threads in the research explain how Americans feel about healthcare in the U.S. at this moment: the role of technology and the cost of health care. First, the vast majority of consumers view technology, broadly defined, as important for their health care. 85% of people
Consumers Use Digital Health Tools But Still Struggle with Health Literacy

While more U.S. patients are use digital health tools and take on more clinical and financial decision making for their health care, people also have gaps in health engagement and health literacy. Three studies published in early October 2017 provide insights into the state of healthcare consumerism in America. The 2017 UnitedHealthcare Consumer Sentiment Survey found that a plurality of Americans (45%) turn first to primary care providers (doctors or nurses) as their source for the first source of information about specific health symptoms, conditions or diseases. 28% of people also use the internet or mobile health apps as their
The Patient As Payor – Americans Bundle Financial Wellness and Healthcare Costs
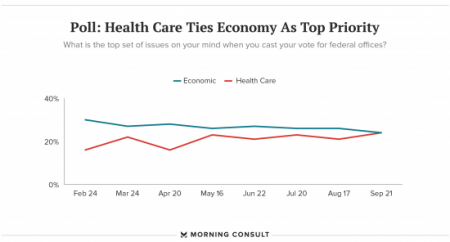
Healthcare and the economy tied for US voters’ top issue last week, as the prospects for repealing the Affordable Care Act faded by the weekend. This Morning Consult poll was published 28th September 2017, as it became clear that the Graham-Cassidy health reform bill would lose at least three key votes the legislation needed for passage: from Rand Paul, Susan Collins, and John McCain. Liz Hamel, who directs the Kaiser Family Foundation’s survey research, told Morning Consult that, “when people say ‘health care,’ they often are actually talking about the economic issue of health care.”
Out-Of-Pocket Healthcare Costs Grow in the Family Budget
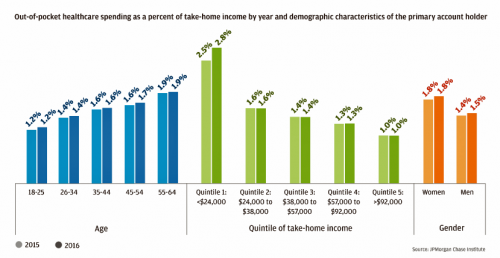
For each dollar spent on healthcare in the United States, families paid 28 cents, according to the U.S. National Health Expenditure Accounts for 2015. Welcome to the new era of Americans and medical banking, with new insights provided by the largest of banks, JP Morgan Chase, in Paying Out-of-Pocket: The Healthcare Spending of 2 Million U.S. Families, from JP Morgan Chase. Chase is the largest bank in America based on its assets. They’ve mined 2.3 million de-identified records of Chase consumers in their banking network to learn about customers’ healthcare spending. These data represent spending between 2013 and 2016, detailed
Prescription Drug Coverage at Work: Common, Complex, and Costly
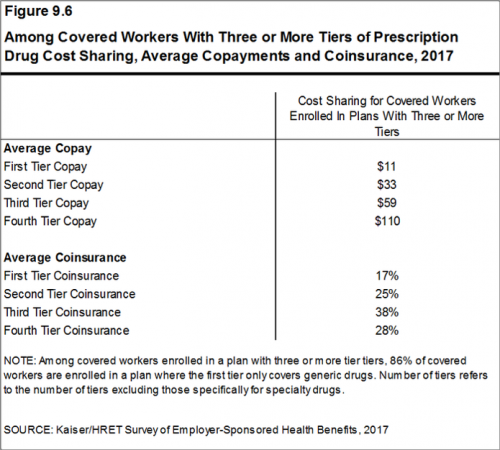
Getting health insurance at work means also having prescription drug coverage; 99% of covered workers’ companies cover drugs, based on the 2017 Employer Health Benefits Survey released by the Kaiser Family Foundation (KFF). I covered the top-line of this important annual report in yesterday’s Health Populi post, which found that the health insurance premium for a family of four covered in the workplace has reached $18,764 — approaching the price of a new 2017 small car according to the Kelley Blue Book. The complexities of prescription drug plans have proliferated, since KFF began monitoring the drug portion of health benefits
Employees Continue To Pick Up More Health Insurance Costs, Even As Their Growth Slows
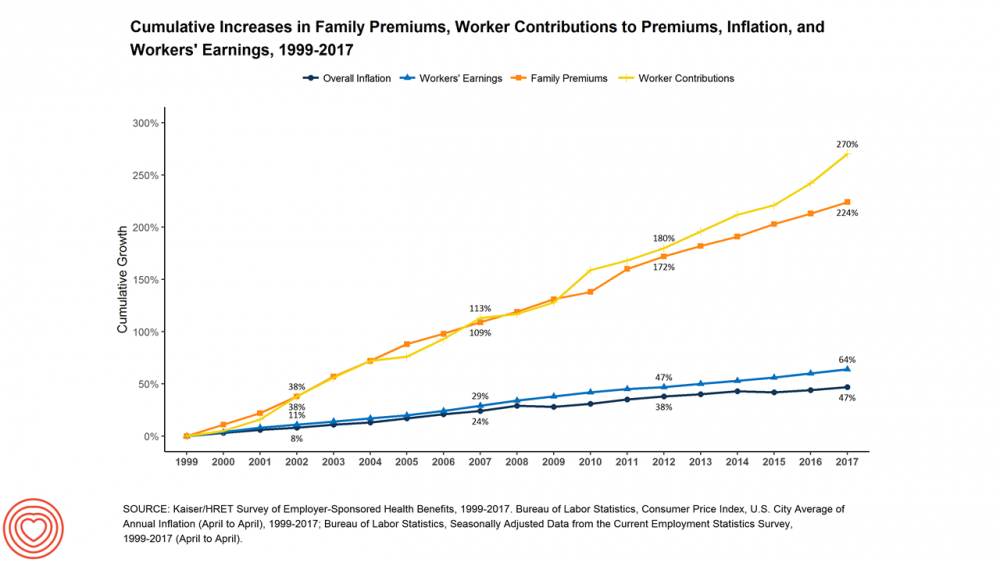
The average cost of an employer=sponsored health plan for a family reached $18,764 in 2017. While this premium grew overall by a historically relative low of 3.4%, employees covered under that plan faced an increase of 8.3% over what their plan share cost them in 2016, according to the 2017 Employer Health Benefit Survey published today by the Kaiser Family Foundation. [Here’s a link to the 2016 KFF report, which provided the baseline for this 8.3% calculation]. Average family premiums at the workplace rose 19% since 2012, a slowdown from the two previous five-year periods — 30% between 2007 and 2012, and
Patients Are Looking to Finance Healthcare Over Time
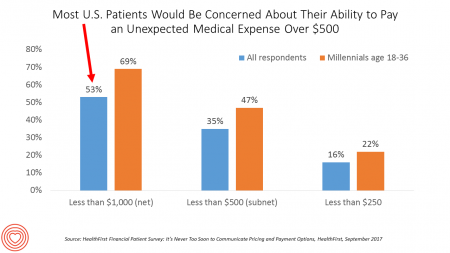
Most U.S. patients want healthcare providers to offer cost information before a procedure, and whether doctors offer financial options to help them extend payments over time. This is an automotive or home appliance procedure we’re talking about. It’s healthcare services, and American patients are now the third largest payors to providers in the nation. Thus, the title of a new report summarizing a consumer survey from HealthFirst notes, “It’s Never Too Soon to Communicate Pricing and Payment Options. The study found that two-thirds of U.S. consumers would like healthcare providers to discuss financing options; however, only 18 percent of providers have
Celebrating 10 Years of Health Populi, 10 Healthcare Milestones and Learnings

Happy anniversary to me…well, to the Health Populi blog! It’s ten years this week since I launched this site, to share my (then) 20 years of experience advising health care stakeholders in the U.S. and Europe at the convergence of health, economics, technology, and people. To celebrate the decade’s worth of 1,791 posts here on Health Populi (all written by me in my independent voice), I’ll offer ten health/care milestones that represent key themes covered from early September 2007 through to today… 1. Healthcare is one-fifth of the national U.S. economy, and the top worrisome line item in the American





 Thank you, Jared Johnson, for including me on the list of the
Thank you, Jared Johnson, for including me on the list of the  I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a