The Health of Older Americans in 2022 – Risks from the Pandemic, Isolation, and Social Determinants
For millions of older people in America, health and well-being got worse in the wake of the COVID-19 pandemic. Physical, mental and behavioral health took hits, depending on one’s living situation, social determinants of health risks, and even health plan, I write in the Medecision Liberate Health blog. In this essay on health disparities and equity for older adults, I weave together new data from, The United Health Foundation’s study on seniors’ health status in America’s Health Rankings for 2022 RAND and CMS research into seniors health disparities among Medicare Advantage
Social Determinants of Health Risks Challenge the Promise of Hospital-to-Home
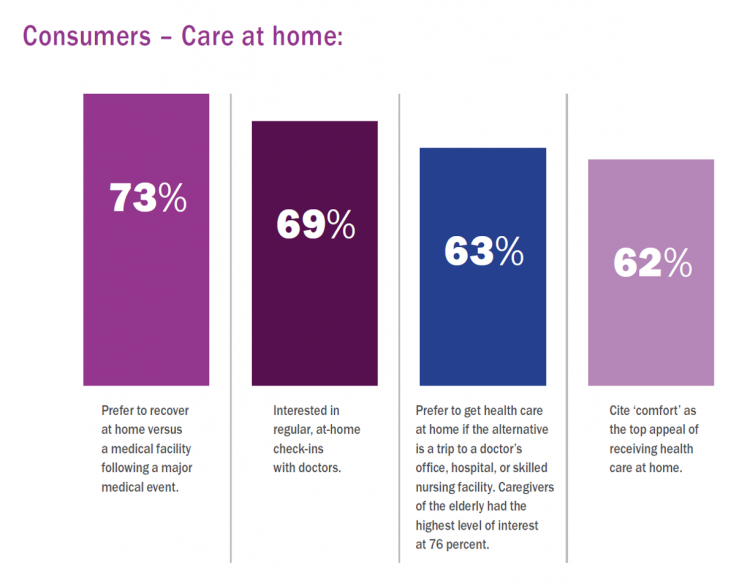
In the wake of the pandemic and growing consumer preferences, the hospital-to-home movement is gaining traction among health systems. Amidst bullish forecasts for the promise of hospital-to-home discharges, the ability for many patients to make this migration would be a difficult bridge to cross. On the promising front, recent studies reviewed through a meta-analysis published in JAMA found that hospital-to-home programs can be clinically and cost-effective for inpatients discharged from hospital. Earlier this year, McKinsey addressed how “Care at Home” ecosystems can reshape the way health systems — and people — envision patient care. This
The Patient as Consumer and Payer – A Focus on Financial Stress and Wellbeing
Year 3 into the COVID-19 pandemic, health citizens are dealing with coronavirus variants in convergence with other challenges in daily life: price inflation, civil and social stress, anxiety and depression, global security concerns, and the safety of their families. Add on top of these significant stressors the need to deal with medical bills, which is another source of stress for millions of patients in America. I appreciated the opportunity to share my perspectives on “The Patient As the Payer: How the Pandemic, Inflation, and Anxiety are Reshaping Consumers” in a webinar hosted by CarePayment on 25 May 2022. In this
Pondering War, Peace, Democracy and Dad on Memorial Day, 2022
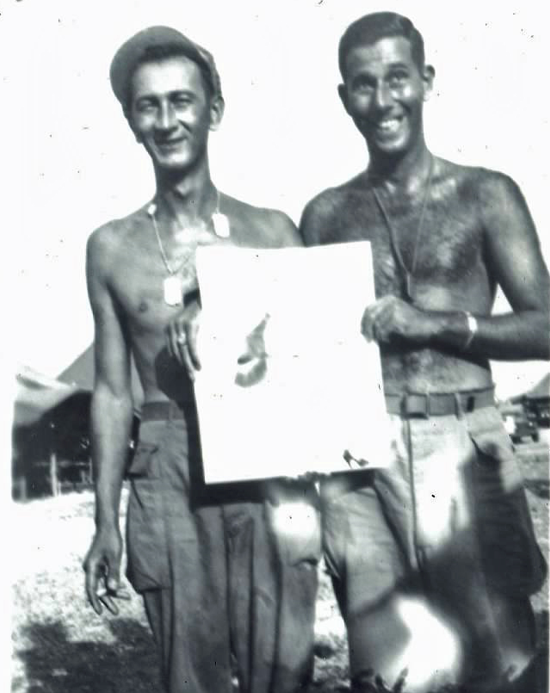
My father, Charles Sarasohn, was a member of the U.S. Army serving as a Jungleer in World War II. He fought in the Pacific Theatre, in New Guinea and the Philippines. Dad’s the one on the right, holding what was a cheeky pin-up drawing. The root of the noun “Jungleer” is “jungle.” Dad carried a long gun with a bayonet on the end, a sort of small sword he and his Best Generation Band of Brothers in the 41st Infantry Division of the U.S, Army used to slash their way through the
How Trust and Geopolitics Will Impact Health and Business – Edelman 2022 Trust Barometer at the World Economic Forum in Davos

When we think about the state of Trust in in mid-2022, there is some good news: Trust is rising (at least in democratic countries, while falling in autocratic ones). The bad news: the gap in Trust has dramatically widened between higher-income people compared with those earning lower-incomes, globally. And that gap is “tinder” that can be quickly sparked into a socio-political fire in countries around the world, Richard Edelman cautioned today when introducing the latest look at the 2022 Edelman Trust Barometer, focusing on geopolitics and business. We have never seen numbers like this
Stress Is Playing A Big Role in Consumers’ Food Habits: Food-As-Medicine Update from IFIC
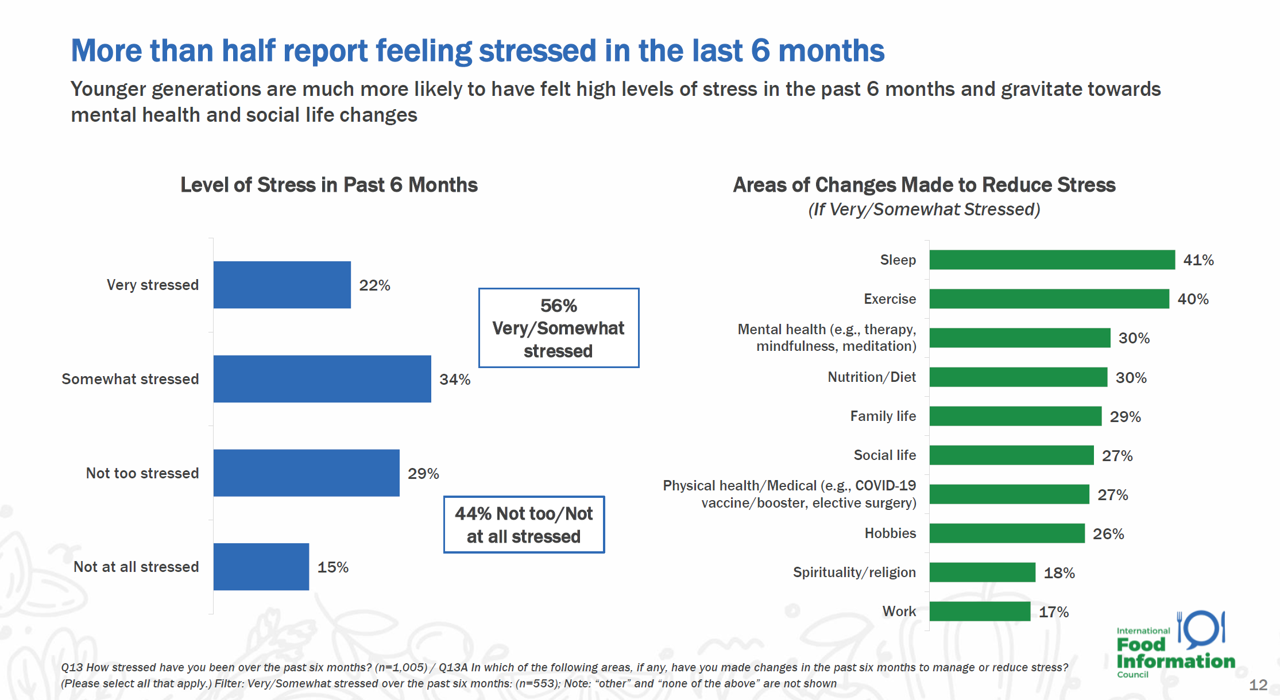
The COVID-19 pandemic accelerated consumers, globally, to take on more DIY roles as well as self-care for health and well-being. In addition, anxiety and stress are mainstream across demographics and have impacted the way people select and consume food, based on findings in the 2022 Food and Health Survey from the International Food Information Council (IFIC). In this 17th annual consumer survey, IFIC points to two underlying macro trends that are re-shaping peoples’ relationship with food and health: the pandemic’s impact, and “significant” generational shifts in taste, consumption, and values about nutrition and sustainability.
Reimagining Health Care Without Walls – Deloitte’s Vision
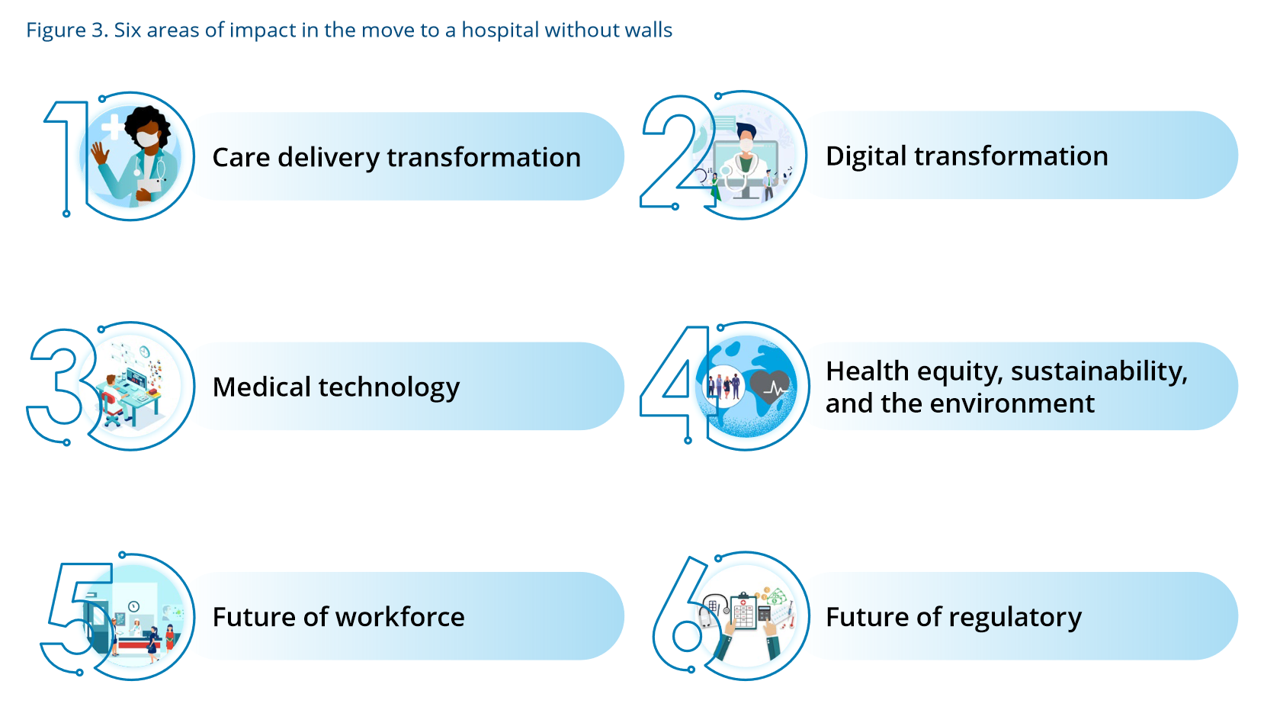
Delivering health care during the heights of the COVID-19 pandemic proved to both patients and their clinicians that virtual care was not only a viable channel for care, but very often a preferable “place” to collaborate for treatment. Even before the coronavirus pandemic emerged in early 2020, telehealth and the hospital-to-home movement were beginning to become part of a portfolio of delivery modes across the continuum of care. Deloitte spells out the current and future prospects for the Hospital in the future “without” walls in a new report that spells out driving forces, future scenarios, and impacts on a business long
Three in Five People 50+ in the US Will Likely Use Telehealth In the Future – An Update from AARP
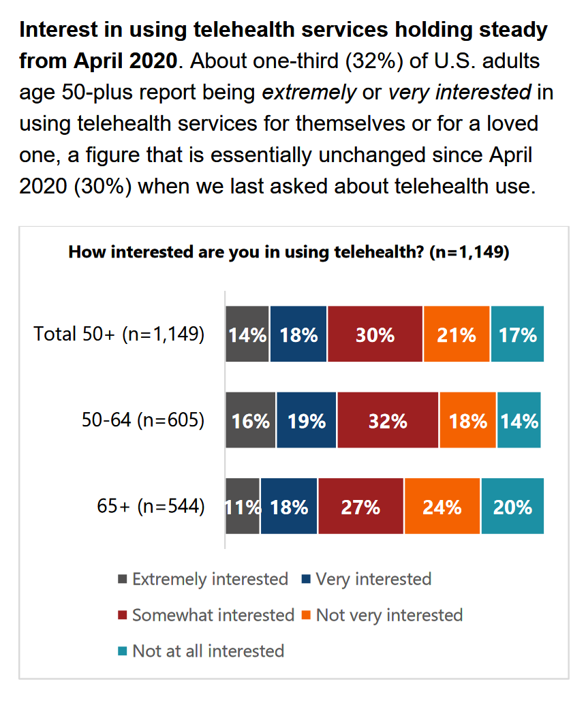
“Telehealth certainly appears to be here to stay,” the AARP forecasts in An Updated Look at Telehealth Use Among U.S. Adults 50-Plus from AARP. Two years after the emergence of the COVID-19 pandemic, one-half of U.S. adults over 50 said they or someone in their family had used telehealth. In early 2022, over half of those over 50 (the AARP core membership base) told the Association they would likely use telehealth in the future. This future expectation varies by race, the implications of which I discuss below in
Telehealth Update from the AMA – Setting the Context for ATA 2022 [Spoiler Alert: Doctors Want to Keep Using Telehealth]
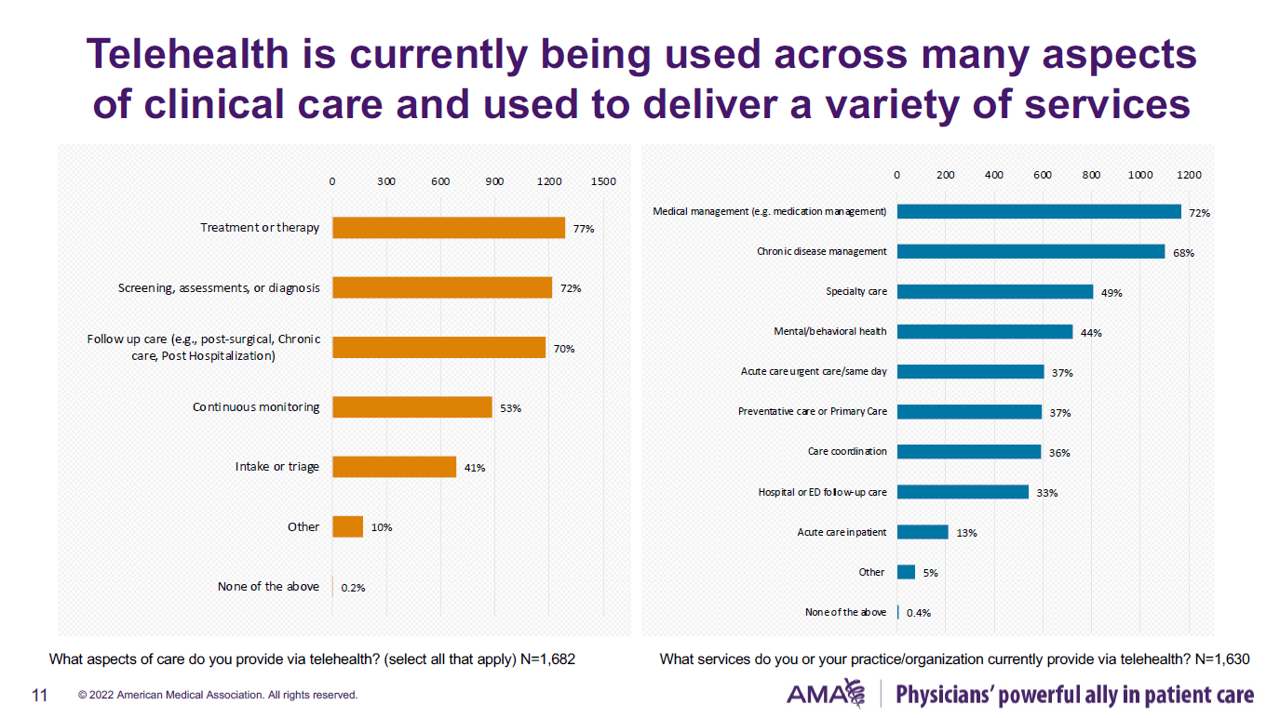
Four in five U.S. physicians were using telehealth to care for patients at the end of 2021. Among those doctors who were not providing telehealth by late 2021, just over one half never did so during the COVID-19 pandemic, according to the 2021 Telehealth Survey Report from the AMA. This report provides insightful context for the upcoming annual ATA Conference for 2022, being held in-person in Boston kicking off May 1st. The meeting will be a strategically important, as the title of the conference asks: “What Now? Creating An Opportunity in a Time of
How Health Gets Built – The Building H Index Thinking Health-By-Design

“It’s hard to be healthy in the U.S. today.” That is the underlying premise and reason for The Building H Index. Health happens outside of doctors’ offices and hospital operating rooms. Health is made in our homes, in our communities, in our daily lives as we go about working, playing, learning, and praying. Too often, in those daily life-flows, making a healthy decision is harder than defaulting to a less-healthy one. Sometimes, it’s pretty impossible given the state of, say, air quality that we breathe, lack of fresh produce and whole foods at the corner market, or seductively designed automobiles
The Color of Care – Oprah and The Smithsonian Channel Partner on Health Equity
A new documentary and educational campaign on health equity will be launched on May 1st, 2022, from Oprah’s Harpo Productions studio partnering with The Smithsonian Channel. The Color of Care documents stories of people who have lost loved ones in the COVID-19 pandemic as well as expert interviews with frontline workers and public health experts and researchers sharing data on systemic racism in health care that has underpinned racial health disparities since slavery was instituted in America. Oprah’s website talked about the project, quoting her saying, “At the height of the pandemic, I read something that stopped me in
How Business Can Bolster Determinants of Health: The Marmot Review for Industry

“Until now, focus on….the social determinants of health has been for government and civil society. The private sector has not been involved in the discussion or, worse, has been seen as part of the problem. It is time this changed,” asserts the report, The Business of Health Equity: The Marmot Review for Industry, sponsored by Legal & General in collaboration with University College London (UCL) Institute of Health Equity, led by Sir Michael Marmot. Sir Michael has been researching and writing about social determinants of health and health equity for decades, culminating publications
In the New Inflationary Era, Gas and Health Care Costs Top Household Budget Concerns
Inflation and rising prices are the biggest problem facing America, most people told the Kaiser Family Foundation March 2022 Health Tracking Poll. Underpinning that household budget concern are gas and health care costs. Overall, 55% of people in the U.S. pointed to inflation as the top challenge the nation faces (ranging from 46% of Democrats to 70% of Republicans). Second most challenging problem facing the U.S. was Russia’s invasion into Ukraine, noted by 18% of people — from 14% of Republicans up to 23% of Democrats. The COVID-19 pandemic has fallen far down Americans’ concerns list tied third place with
McKinsey’s Six Shifts To Add Life to Years — and One More to Consider
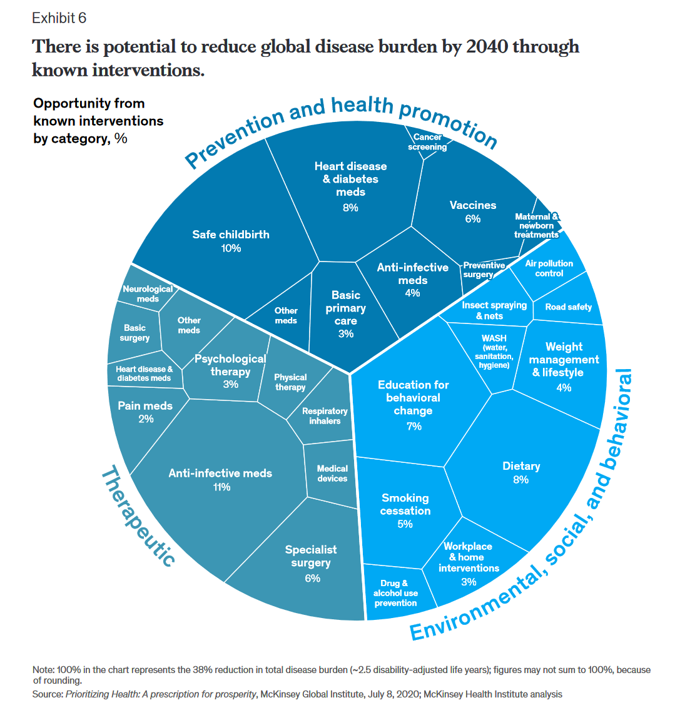
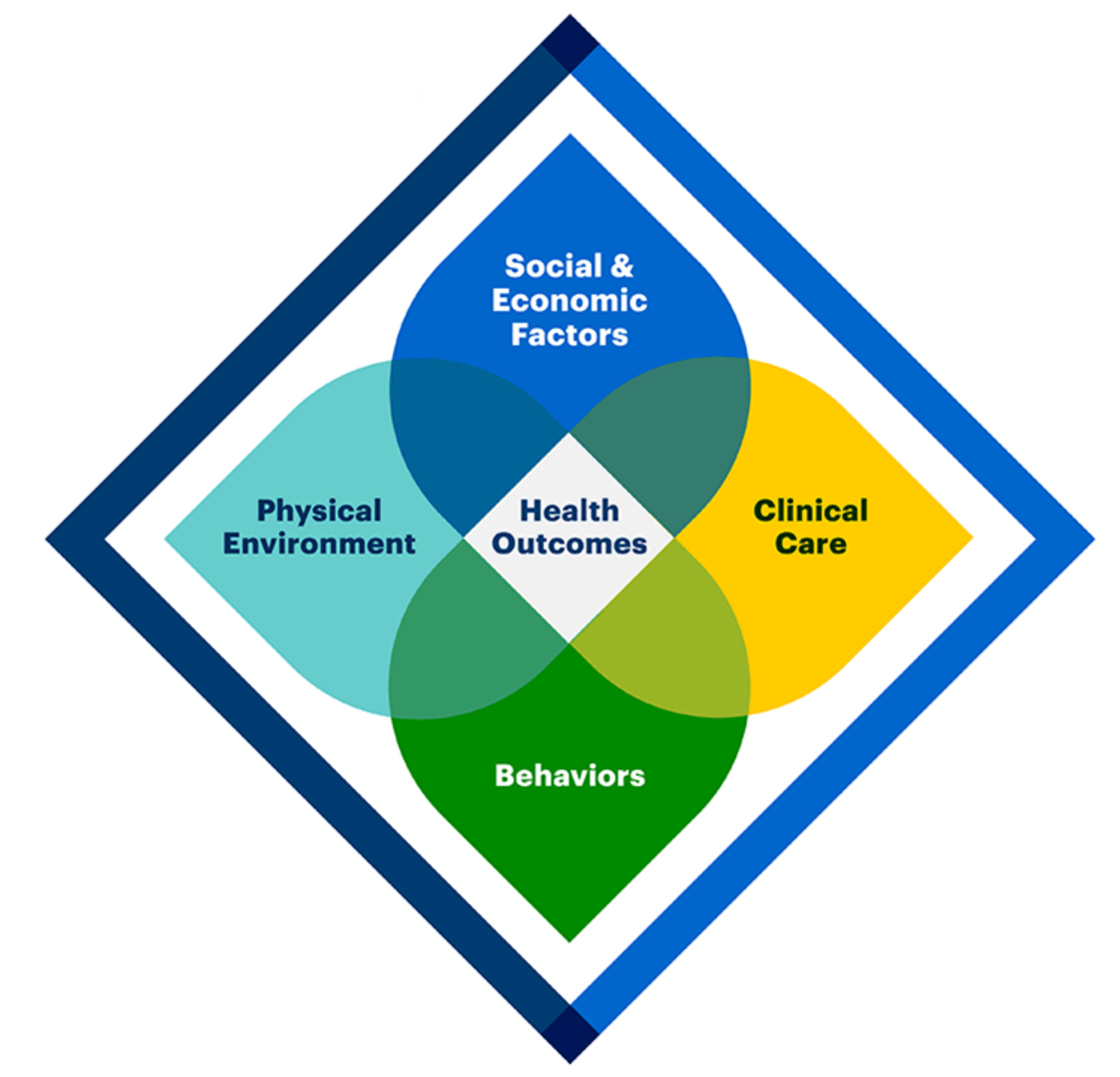
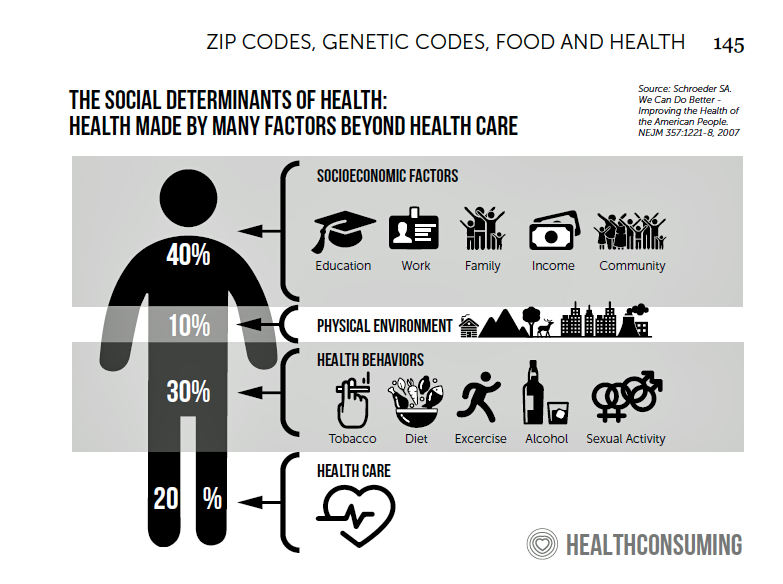
People spend one-half of their lives in “less-than-good health,” we learn early in the paper, Adding years to life and life to years from the McKinsey Health Institute. In this data-rich essay, the McKinsey team at MHI sets out an agenda that could help us add 45 billion extra years of higher-quality life equal to an average of six years per person (depending on your country and population demographics). The first graphic from the report illustrates four dimensions of health and the factors underneath each of them that can bolster or diminish our well-being: personal behaviors (such as sleep and diet),
Can a Food-As-Medicine App Extend Chronic Health Management at the Grocery Store?
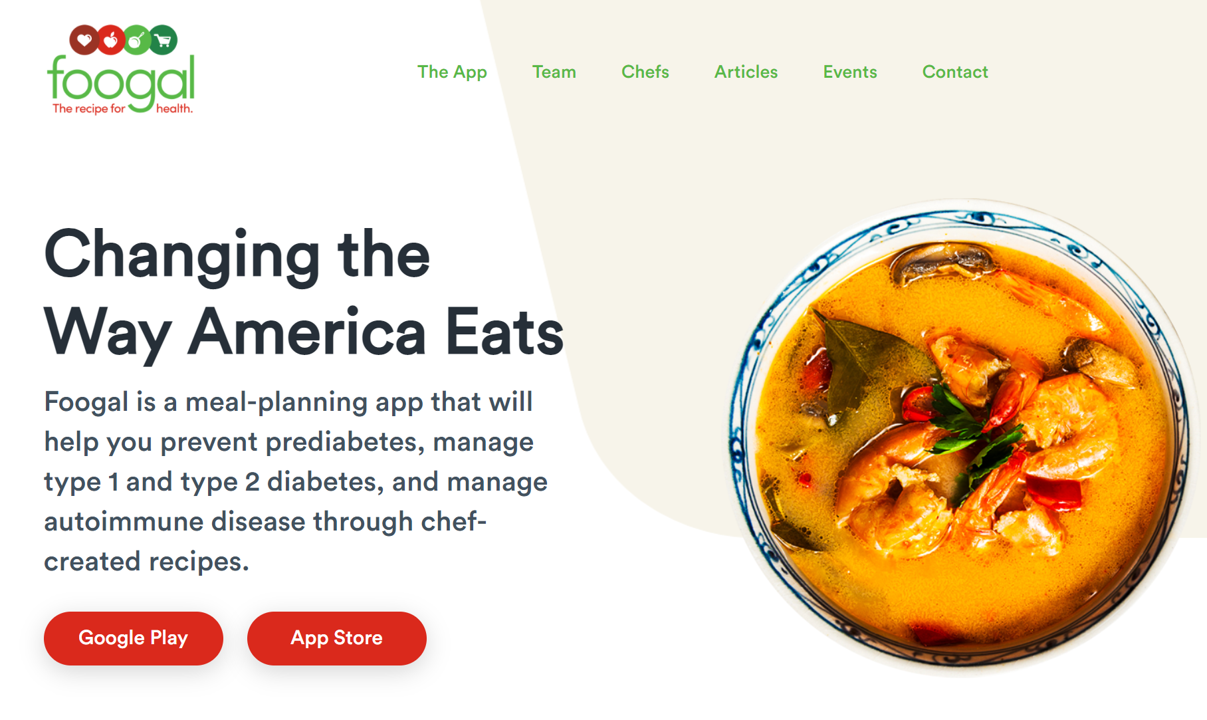
Foogal, a recipe app designed to support patients’ healthy cooking and eating, launched on 24th March. In its initial version, Foogal addresses several specific diet paradigms: for patients demanding a wellness protocol, an autoimmune protocol, or wanting to address insulin resistance. Foogal got my attention via a tweet @FoogalApp on 25th March. The snippet featured a photo of a delectable Salad Lyonnaise, one of my favorite things to eat, which adds a soft-cooked egg and bacon lardons to the greens for an easy light (and delicious!) meal. Foogal was developed by Todd Knobel, who has worked in law, in plastics,
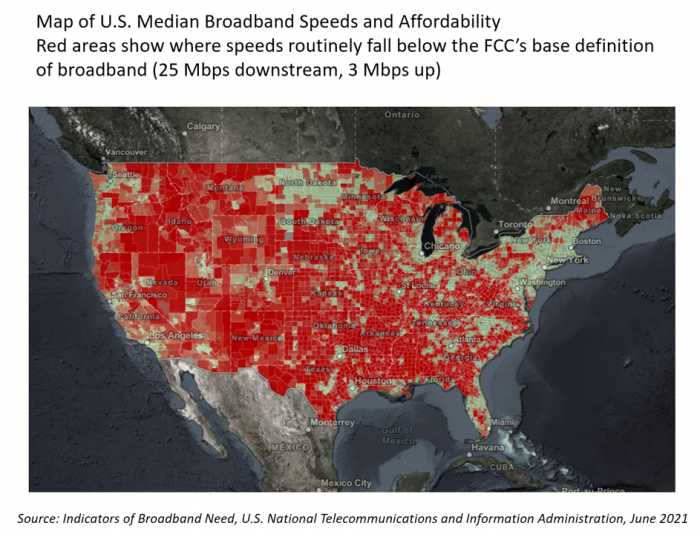
People in the U.S. Without the Internet Were More Likely To Die in the Pandemic
Access to the Internet has been a key determinant of health — or more aptly, death — during the COVID-19 pandemic. Americans lacked Internet access were more likely to die due to complications from the coronavirus, according to a study published in JAMA Network Open this month. The study’s key finding was that for every additional 1% of people living in a county who have access to the Internet, between 2.4 and 6.0 COVID-19 deaths per 100,000 were preventable. The paper asserts that, “More awareness is needed about the essential asset of technological access to reliable information, remote work, schooling
The Financial Toxicity of Health Care Costs: From Cancer to FICO Scores
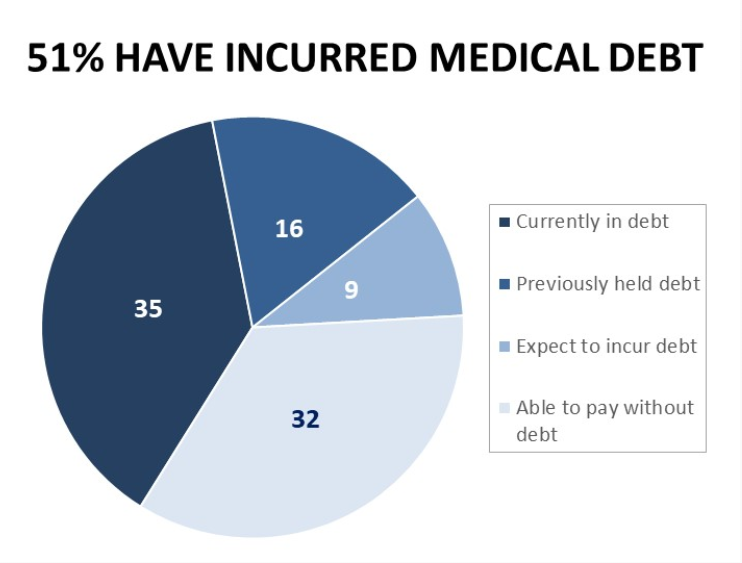
The financial toxicity of health care costs in the U.S. takes center stage in Health Populi this week as several events converge to highlight medical debt as a unique feature in American health care. “Medical debt is the most common collection tradeline reported on consumer credit records,” the Consumer Financial Protection Bureau called out in a report published March 1, 2022. CFPB published the report marking two years into the pandemic, discussing concerns about medical debt collections and reporting that grew during the COVID-19 crisis. Let’s connect the dots on: A joint announcement this week from three major credit agencies,
Primary Care in the U.S. – Still a Weak Backbone for the Health of Health Citizens
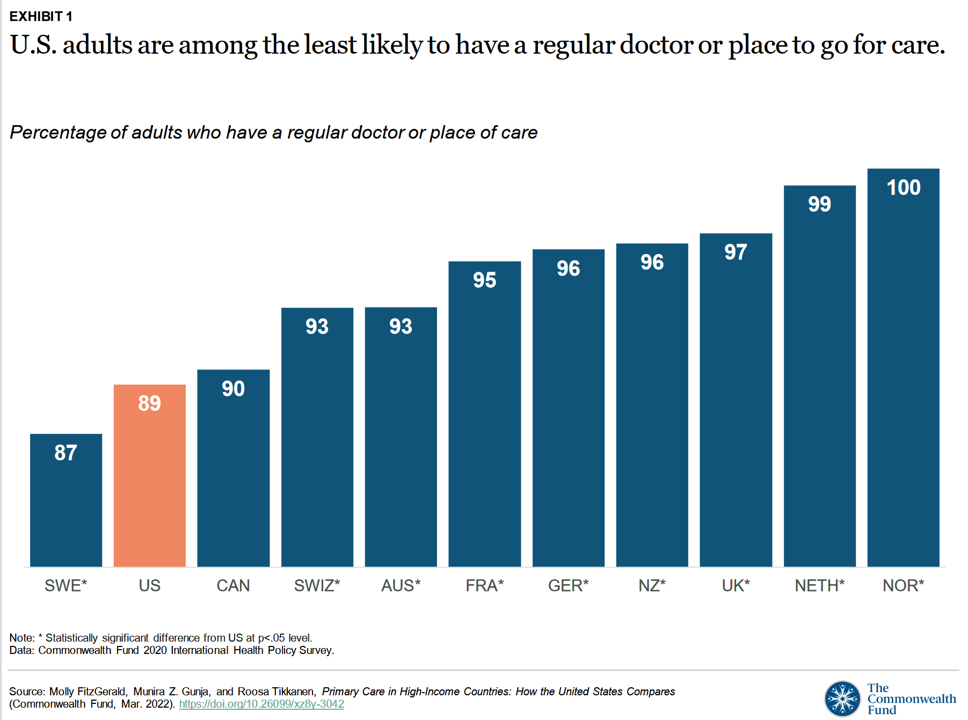
Compared with health citizens living in other wealthy countries, people living in the U.S. are still among the least likely to have a regular doctor or place to go for care. Thus, millions of Americans continue to lack access to primary care compared with peers in other nations, according to a report from The Commonwealth Fund. The Commonwealth Fund has tracked primary care access for many years, and over time has found the United States to lack the kind of primary care “backbone” that many wealthy nations have — whose health citizens also enjoy much better health outcomes that relate
Thinking About Telehealth Through the Lens of Real Estate – Listening to JLL
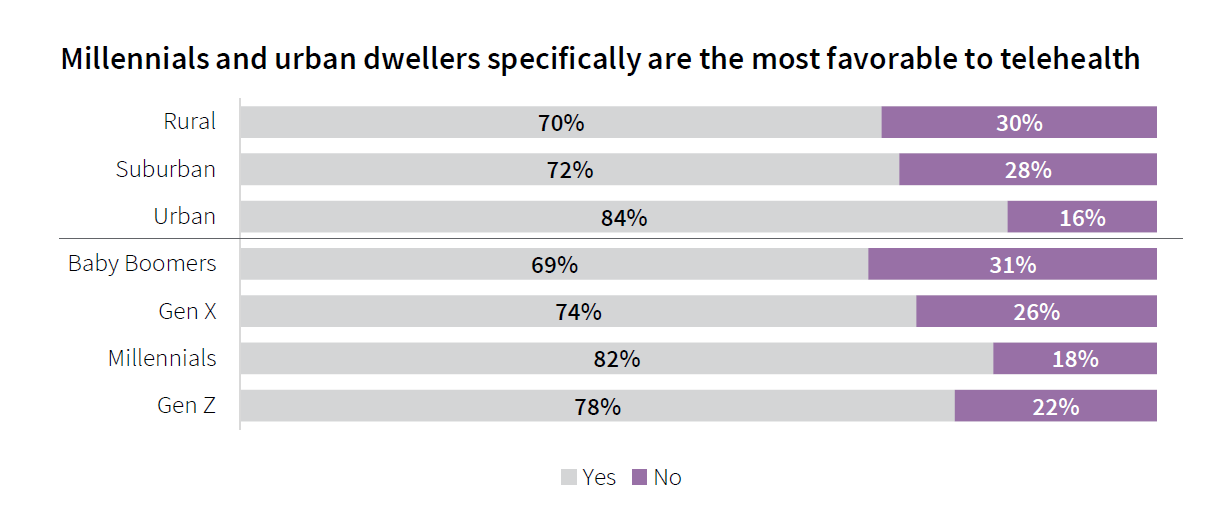
If you made your living in commercial real estate — and especially, working with hospitals’ and health systems’ office space — would the concept of telehealth be freaking you out right now? If you heed the words of JLL’s 2022 Patient Consumer Survey, you’d chill (at least a bit). The tagline on this paper is, “Convenience and choice drive patient decisions as new digital options take hold.” I was particularly keen to dig into this study based on its sponsoring organization: JLL is a real estate services company serving over a dozen vertical markets — including health care, life sciences,
Techquity: How Technology Can Help to Scale Health and Digital Equity, Live from VIVE 2022
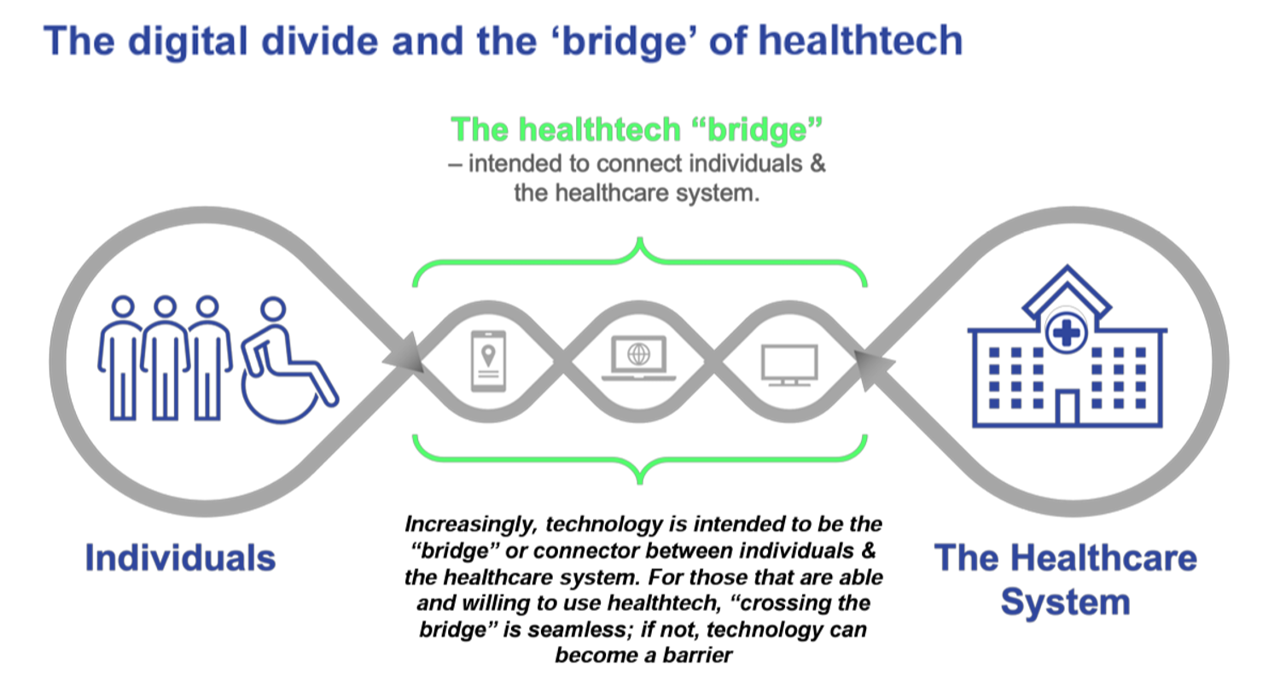
The COVID-19 pandemic revealed long-systemic health disparities in the U.S. and in other parts of the world. Income inequality, sickly environments in homes and communities (think unclean air and water), lack of public transportation and nutritious food deserts combine to limit peoples’ health and well-being., Beyond the traditional social determinants of health, such as these, we’ve called out another health risk that became crucial for life in the coronavirus pandemic era: digital connectivity, Indeed, WiFi and broadband represent the newest social determinant of health to add to a growing list of risk factors that challenge health citizens’ health. Kudos to
Love and Health: The Education of Abner Mason, SameSky Health
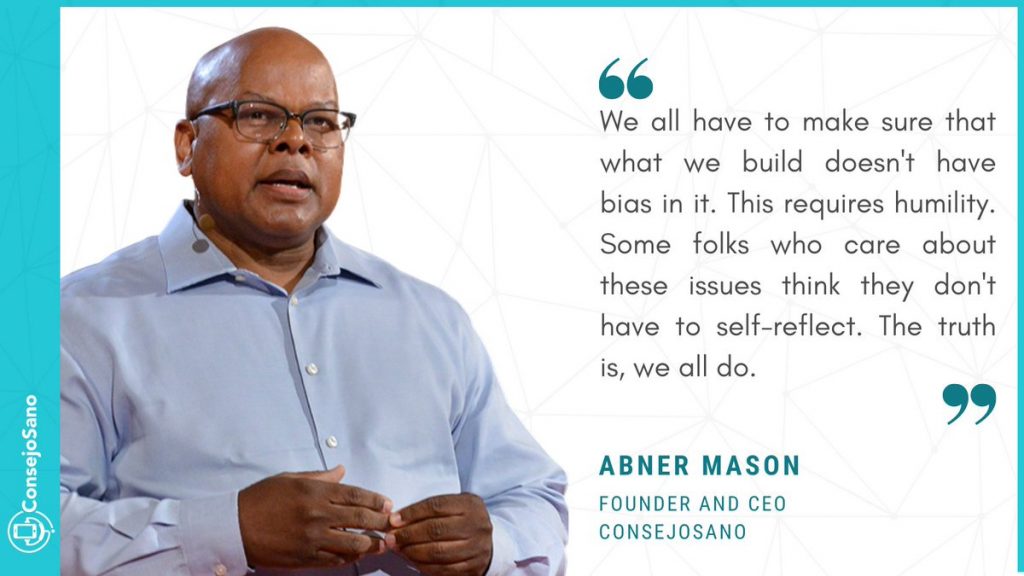
It felt super appropriate that I met up with Abner Mason, Founder of SameSky Health, on Valentine’s Day 2022. While we conversed via Zoom, Abner’s positive energy vibrated over the 5,600 miles between him in LA County and me in Brussels, Belgium – nine hours apart, but in the proverbial same room in the conversation. My initial ask of Abner was to discuss the re-branding of ConsejoSano to SameSky Health, but I first wanted to hear the man’s origin story. And that, you will learn, has everything to do with loving parents, the power of education from a young age,
“We’ve normalized a very high death toll in the U.S.” – How A Trust Deficit Has Infected America’s COVID Outcomes
Trust, or really lack thereof, is a killer app for people’s coronavirus health outcomes. That is the through-line found in a very deep dive into 177 countries’ health data published in The Lancet in a research article on pandemic preparedness and COVID-19. The Lancet study, published on 1 February 2022, was funded by the Gates Foundation in partnership with The Bloomberg Philanthropies et al. The study was researched and written up by a team of COVID-19 National Preparedness Collaborators, led by Dr. Joseph Dieleman of the University of Washington’s Institute for Health Metrics and Evaluation, a group that has been long-tracking
From Better for Me to Better for “We” — NielsenIQ’s New Consumer Hierarchy of Health
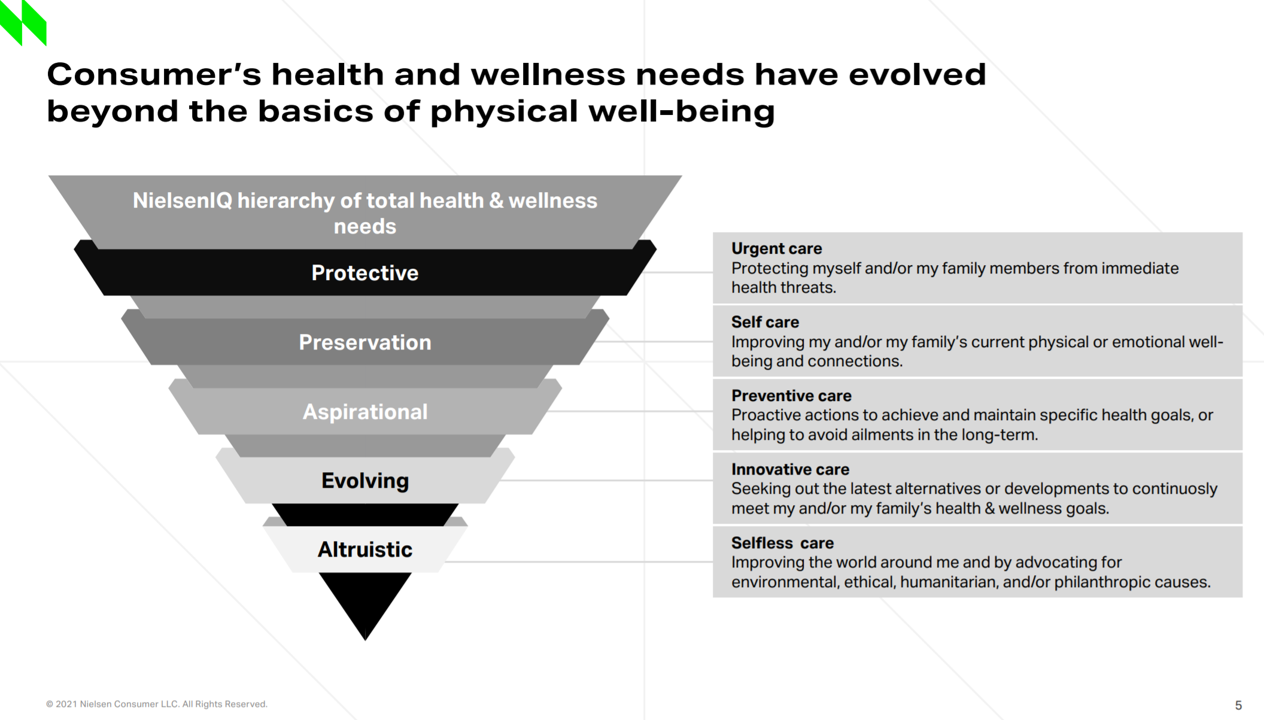
People around the world have made health a “proactive priority,” most important to live a longer, healthier life, to avoid preventable diseases, to protect against disease, and to look and feel healthier, according to NielsenIQ’s latest health and wellness report. As the triangle here illustrates, NielsenIQ has turned Maslow’s Hierarchy of Needs upside down, shifting protective and physical needs to the top rung and altruistic — the “me-to-we” ethos — at the base. Note the translations of these needs, on the ride, into the “care” flows — moving from urgent care down to self-care, preventive care, innovative care, and selfless
The Trust Deficit Is Bad for Health: A Health/Care Lens on the 2022 Edelman Trust Barometer
“Health is the cornerstone to our core needs, thereby the cornerstone to trust.” So wrote Kirsty Graham, Global Leader of Sectors and Global Chair of Health at Edelman, in an essay explaining the 2022 Edelman Trust Barometer. If it’s January, it must be time for the World Economic Forum in Davos, the annual setting for Edelman’s launch of the company’s Trust Barometer. While WEF is mostly virtual this year due to the pandemic, Edelman has released the survey of global citizens’ views on trust in institutions right on-time and in full and sobering detail. I welcome and dig into the
Building Health Equity Through Faith and Food – the Black Church Food Security Network

Members of his congregation kept going to the hospital with diet-related issues, Reverend Dr. Heber Brown, III, realized. “I got tired of praying and hoping they made it and walked out,” Reverend Brown realized. And then… “God gave us an idea and vision to be proactive on the issue of health in our congregation,” Rev. Brown explained to us yesterday on Day 2 of Real Chemistry’s Health Equity Summit. This was the seed for the Black Church Food Security Network, planting a pragmatic vision for health and well-being weaving together local food, civic empowerment, economic development, and faith. “We had
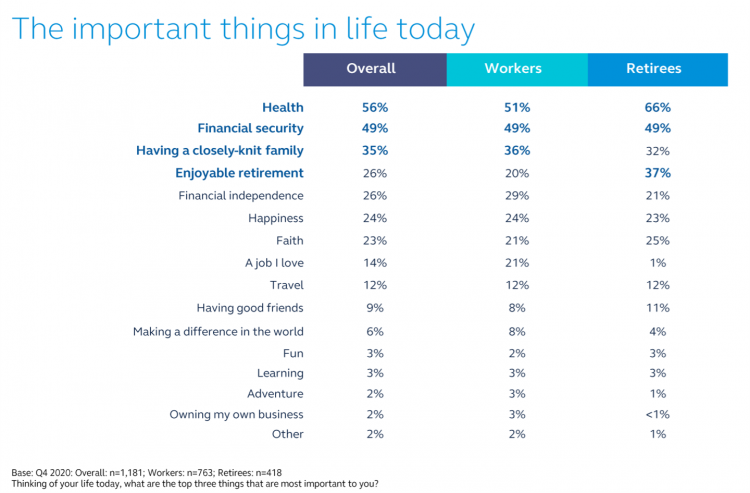
Nurses Continue to Rule in Honesty and Ethics in U.S. Professions – Healthcare Professions Still Top Gallup’s Annual Poll
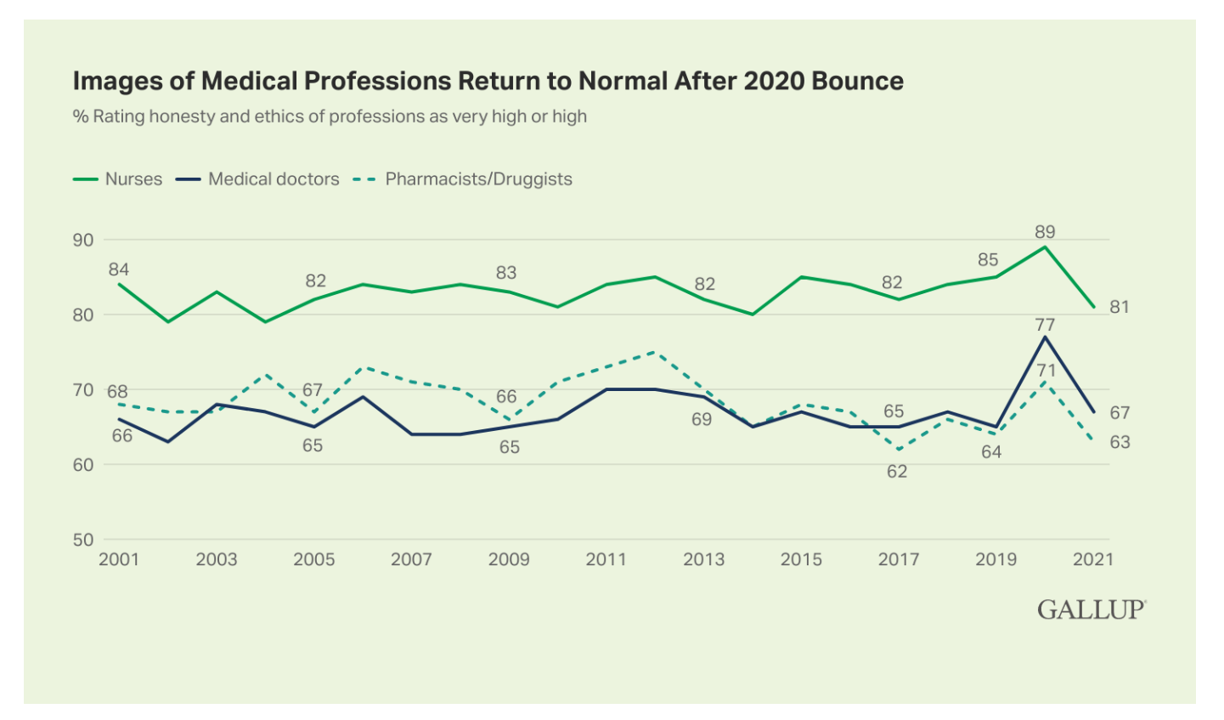
Three health care professions rank in the top four of the most honest and ethical rankings in Gallup’s annual poll on honesty and ethics in professions. And nurses are at the top of the list for the 20th year in a row. Grade-school teachers ranked third place between physicians and pharmacists, shown in the big chart of job types from most ethical to least. Perennially, the bottom-ranked posts are a mix of politicians (Members of Congress and lobbyists, state office holders), car salespeople, and the Mad Men and Women of advertising. Media professionals in TV and newspapers also polled relatively
Does Inequality Matter in the U.S.? Health and the Great Gatsby Curve
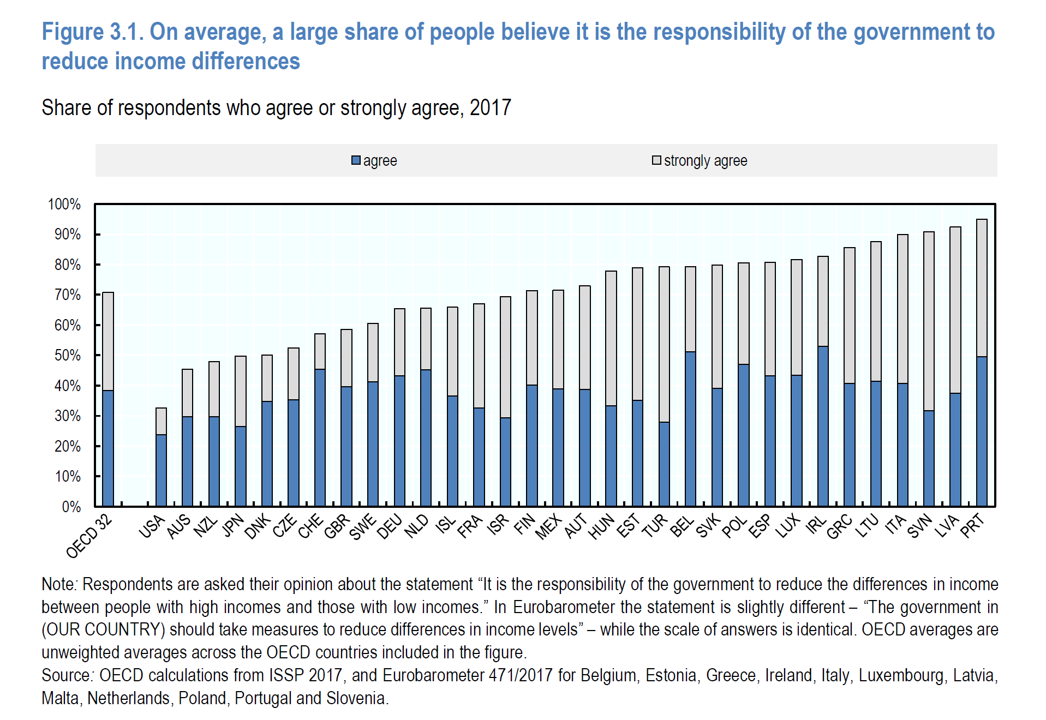
Compared with the rest of the developed world, people living in the U.S. may be concerned about income inequality, but their demand for income redistribution is the lowest among peer citizens living in 31 other OECD countries. In their latest report, Does Inequality Matter? the OECD examines how people perceive economic disparities and social mobility across the OECD 32 (the world’s developed countries from “A” Australia to “U,” the United Kingdom). Overall the OECD 32 average fraction of people who believe it is the government’s responsibility to reduce income differences among those who think disparities are too large is 80%
Health Citizens Link Their Views on Democracy, the Economy and the Pandemic
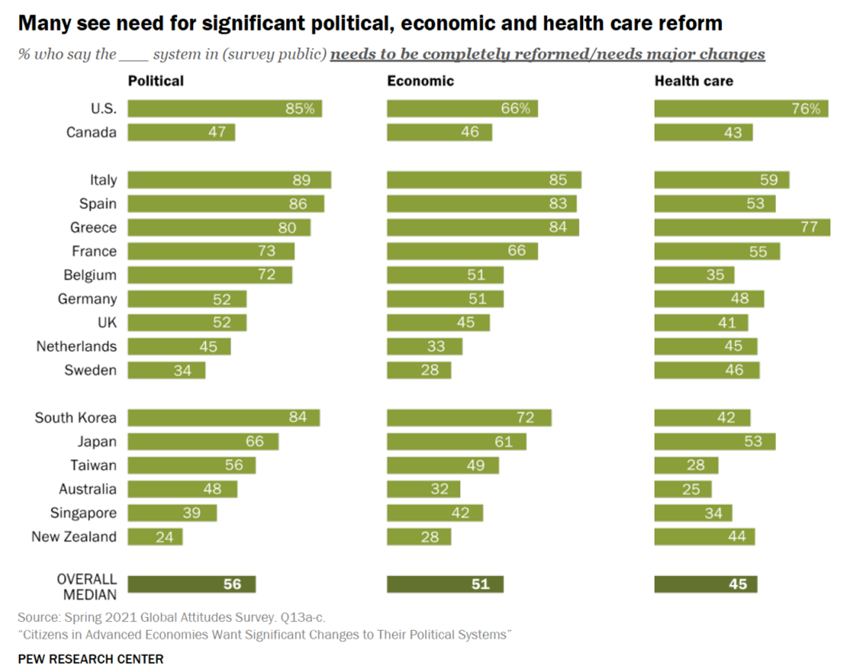
The pandemic has put health care top-of-mind for health citizens the world over. As the public health crisis continues its up-and-downticks around the globe, people are connecting health care to their national economies and politics, based on a global survey from the Pew Research Center, Citizens in Advanced Economies Want Significant Changes to Their Political Systems. For this analysis, the Pew research team assessed the views of some 2,600 health citizens living in 17 developed countries in February 2021. The study report was published in late October 2021. Shown in the first bar chart, the majority of people in at least
Still Struggling with Stress in America in 2021
“Americans remain in limbo between lives once lived and whatever the post-pandemic future holds,” the American Psychological Association observes in their latest read into Stress in America 2021, with this phase of the perennial study focused on Stress and Decision-Making During the Pandemic. The top-line: people face a daily web of risk assessment, up-ended routines, and endless news about the coronavirus locally and globally. While most people in the U.S. believe that “everything will work out” after the pandemic ends, the mental, emotional, and logistical daily distance between “now” and “then” brings uncertainty and indeed, prolonged stress. More Millennials, who
Be Mindful About What Makes Health at HLTH
“More than a year and a half into the COVID-19 outbreak, the recent spread of the highly transmissible delta variant in the United States has extended severe financial and health problems in the lives of many households across the country — disproportionately impacting people of color and people with low income,” reports Household Experiences in America During the Delta Variant Outbreak, a new analysis from the Robert Wood Johnson Foundation, NPR, and the Harvard Chan School of Public Health. As the HLTH conference convenes over 6,000 digital health innovators live, in person, in Boston in the wake of the delta
Support for Drug Price Negotiation Brings Partisans Together in the U.S.
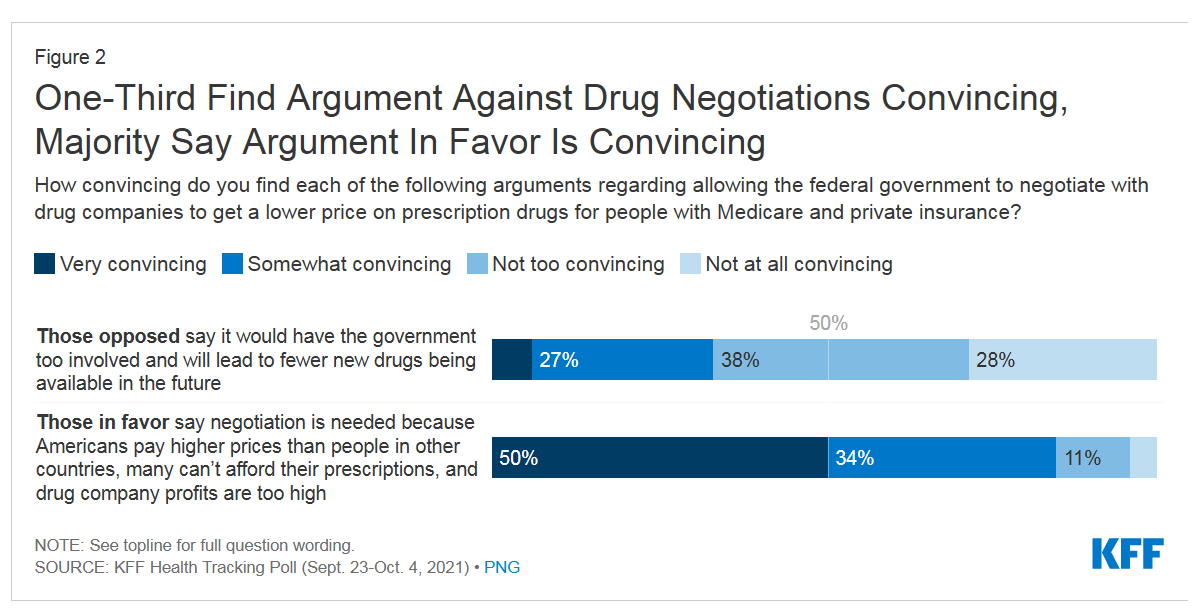
Most U.S. adults across political parties favor allowing the Federal government authority to negotiate for drug prices — even after hearing the arguments against the health policy. Drug price negotiation, say by the Medicare program, is a unifying public policy in the current era of political schisms in America, based on the findings in a special Kaiser Family Foundation (KFF) Health Tracking Poll conducted in late September-early October 2021. Overall, 4 in 5 Americans favor allowing the Federal government negotiating power for prescription drug prices, shown in the first chart from the KFF report. By party, nearly all Democrats agree
The Biggest Threat to Our Health Isn’t the Next Pandemic or Cancer…It’s Climate Change
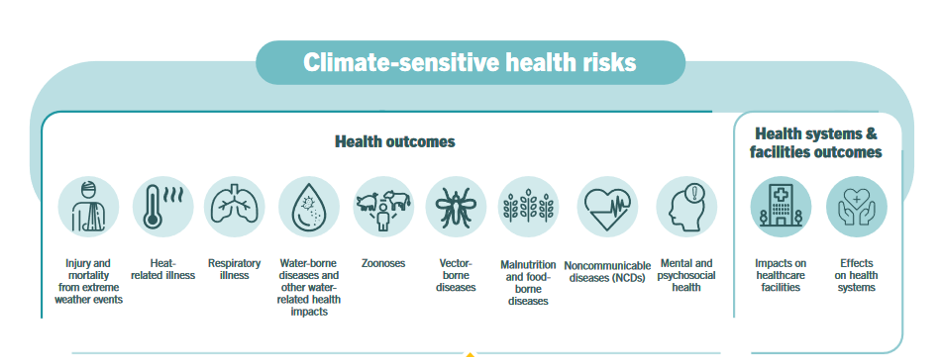
Before the coronavirus emerged, the top causes of death in developed countries were heart disease, cancers, diabetes, and accidents. Then COVID-19 joined the top-10 list of killers in the U.S. and the issue of pandemic preparedness for the next “Disease X” became part of global public health planning. But the biggest health threat to human life is climate change, according to a new report from the World Health Organization titled The Health Argument for Climate Action. It’s WHO’s special report on climate change and health, dedicated to the memory of Ella Kissi-Debrah — a child who died succumbing to impacts
Consider Mental Health Equity on World Mental Health Day
COVID-19 exacted a toll on health citizens’ mental health, worsening a public health challenge that was already acute before the pandemic. It’s World Mental Health Day, an event marked by global and local stakeholders across the mental health ecosystem. On the global front, the World Health Organization (WHO) describes the universal phenomenon and burden of mental health on the Earth’s people… Nearly 1 billion people have a mental disorder Depression is a leading cause of disability worldwide, impacting about 5% of the world’s population People with severe mental disorders like schizophrenia tend to die as much as 20 years earlier
Genentech’s Look Into the Mirror of Health Inequities

In 2020, Genentech launched its first study into health inequities. The company spelled out their rationale to undertake this research very clearly: “Through our work pursuing groundbreaking science and developing medicines for people with life-threatening diseases, we consistently witness an underrepresentation of non-white patients in clinical research. We have understood inequities and disproportionate enrollment in clinical trials existed, but nowhere could we find if patients of color had been directly asked: ‘why?’ So, we undertook a landmark study to elevate the perspectives of these medically disenfranchised individuals and reveal how this long-standing inequity impacts their relationships with the healthcare system
Necessity is the Mother(board) – How COVID-19 Inspires Local Communities to Build Broadband
“The simple fact is that the federal and state governments are doing almost nothing to help people who have a broadband service available that partially meets their needs but abuses them with regular price hikes, spotty reliability, and poor customer service. Local governments will continue to step in to build better networks because communities have very few other options.” That “necessity is the mother” motivation to build broadband comes from Christopher Mitchell, Director of the Community Broadband Networks Initiative at the Institute for Local Self-Reliance (ILSR). [FYI, Mitchell’s Twitter handle is @communitynets]. Mitchell is quoted in the story, New data
A Nutrition Label for Health IT
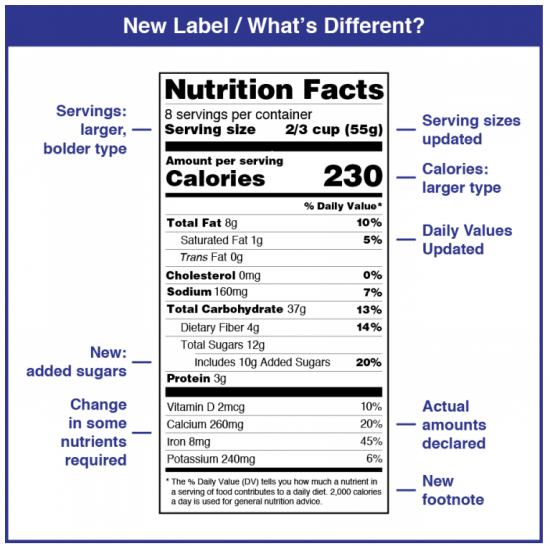
“Shouldn’t we, as a society, demand a nutrition label on our algorithms?” asked Dr. John Halamka. Dr. Halamka, President of the Mayo Clinic Platform, was speaking at the HIMSS 2021 annual conference on the meeting’s digital channel. Artificial intelligence and health equity were two key themes discussed during #HIMSS21, and Dr. Halamka’s concerns echoed through the week-long event. To illustrate the need for a healthier approach to AI, he offered this scenario: “If I use a data set of one million Scandinavian Lutherans to create the most amazing EKG algorithm ever and then we decide to use it in Spain,
Health Disparities in America: JAMA Talks Structural Racism in U.S. Health Care

“Racial and ethnic inequities in the US health care system have been unremitting since the beginning of the country. In the 19th and 20th centuries, segregated black hospitals were emblematic of separate but unequal health care,” begins the editorial introducing an entire issue of JAMA dedicated to racial and ethnic disparities and inequities in medicine and health care, published August 17, 2021. This is not your typical edition of the Journal of the American Medical Association. The coronavirus pandemic has changed so many aspects of American health care for so many people, including doctors. Since the second quarter of 2020,
Nurses and Aides Are Beloved and Deserve Higher Pay; and a Spotlight on the Filipinx Frontline
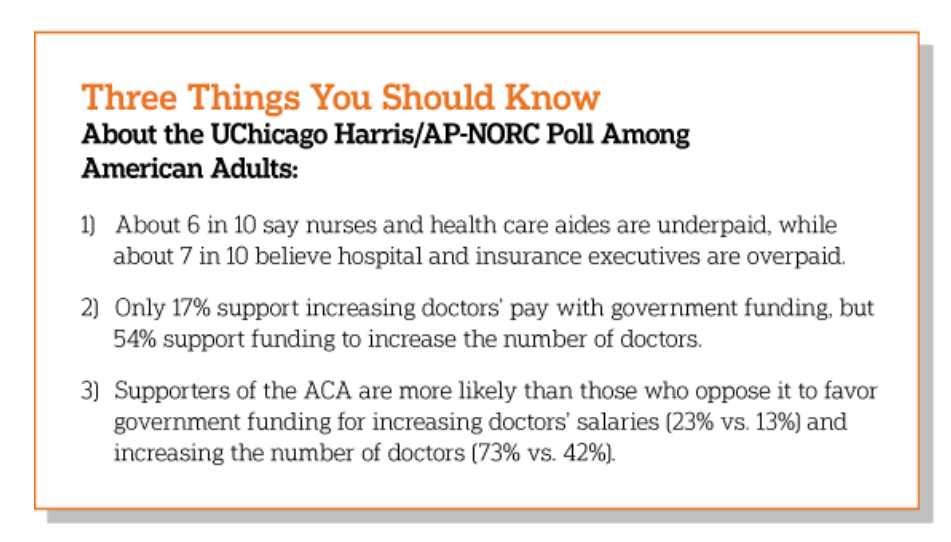
A majority of Democrats, Independents, and Republicans agree that nurses are underpaid. Most Americans across political parties also believe that hospital executives are overpaid, according to a poll from The Associated Press-NORC Center for Public Affairs Research. The survey analysis is aptly titled, Most Americans Agree That Nurses and Aides Are Underpaid, While Few Support Using Federal Dollars to Increase Pay for Doctors, . Insurance executives are also overpaid, according to 73% of Americans — an even higher percent of people than the 68% saying hospital execs make too much money. In addition to nurses being underpaid, 6 in 10
Pondering Prescription Drugs: Pricing Rx and Going Direct-to-Consumer
There is one health care public policy issue that unites U.S. voters across political party: that is the consumer-facing costs of prescription drugs. With the price of medicines in politicians’ and health citizens’ cross-hairs, the pharmaceutical and biotech industries have responded in many ways to the Rx pricing critiques from consumers (via, for example, Consumer Reports/Consumers Union and AARP), hospitals (through the American Hospital Association), and insurance companies (from AHIP, America’s Health Insurance Plans). The latest poll from the University of Chicago/Harris Public Policy and the Associate Press-NORC Center for Public Affairs Research quantifies the issue cross-party, finding that 74%
Our Pandemic Lessons: Listening to Michael Dowling – a #HIMSS21 Wrap-Up

“We don’t un-learn,” Dr. Amy Abernethy asserted as she shared her pandemic perspectives on a panel with 2 other former U.S. health policy and regulatory leaders. The three spoke about navigating compliance (think: regulations and reimbursement) in an uncertain world. An uncertain world is our workplace in the health/care ecosystem, globally, in this moment. So to give us some comfort in our collective foxhole, my last post for this week of immersion in #HIMSS21 is based on the keynote speech of Michael Dowling, CEO of Northwell Health. Dowling keynoted on the theme of “Leading for the Future,” sharing his lessons
Can the U.S. Improve Health System Performance with Digital Health Tools? Pondering A Big Question for #HIMSS21
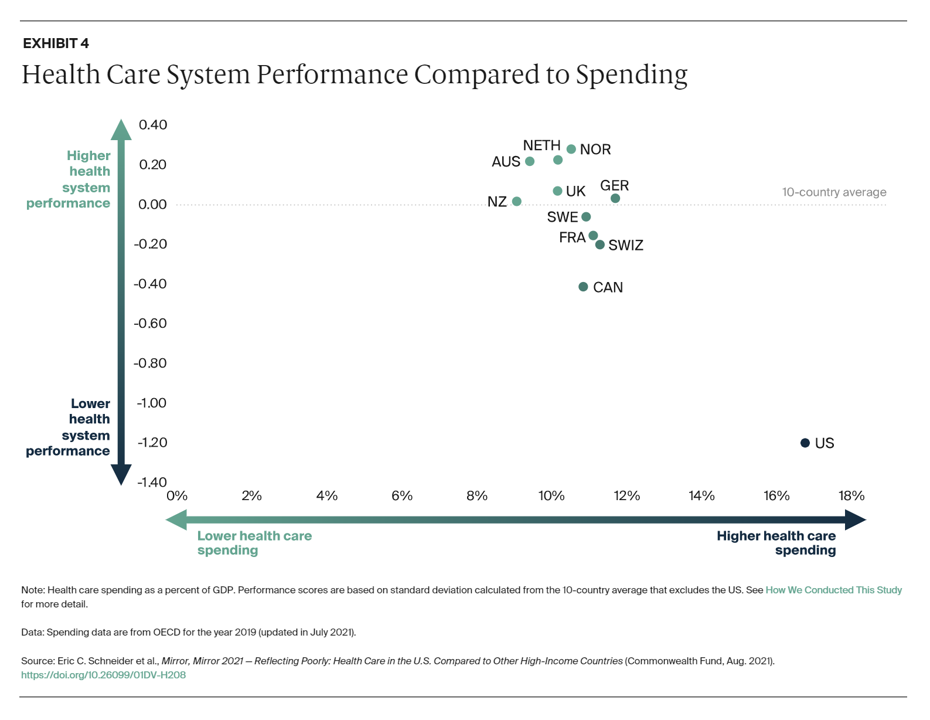
Simply put, is the equation, “Spend more, get less” a sustainable business model? Of course not. But that’s the simple math on U.S. health care spending and what comes from it, according to Mirror, Mirror 2021: Reflecting Poorly, a perennial report from The Commonwealth Fund that compares health system performance across eleven developed countries. The first table details the metrics that the Fund compares across the eleven peer nations, which included Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the United Kingdom, and the United States. The metrics compared were access to care, care process, administrative efficiency, equity,
Digital Inclusion As Upstream Health Investment
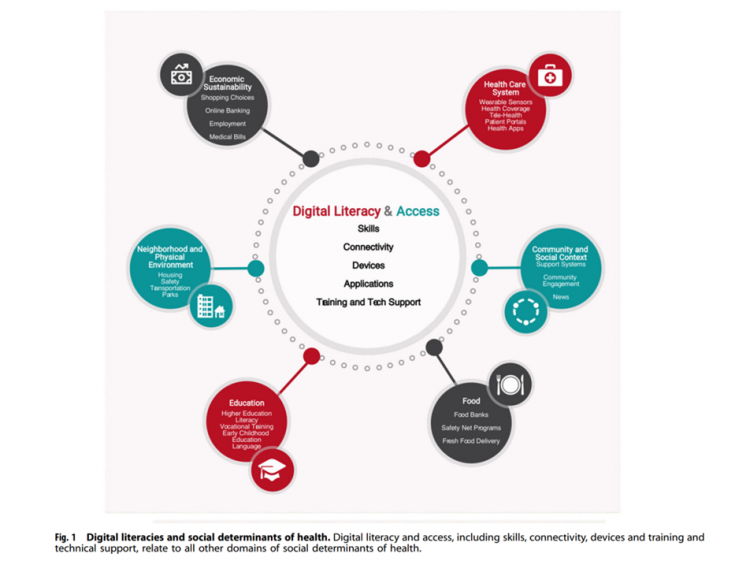
Without access to connectivity during the pandemic, too many people could not work for their living, attend school and learn, connect with loved ones, or get health care. The COVID-19 era has shined a bright light on what some of us have been saying since the advent of the Internet’s emergence in health care: that digital literacies and connectivity are “super social determinants of health” because they underpin other social determinants of health, discussed in Digital inclusion as a social determinant of health, published in Nature’s npj Digital Medicine. On the downside, lack of access to digital tools and literacies
The Healthcare and Macro-Economic Impacts of Living with Endemic COVID – Listening to Fitch
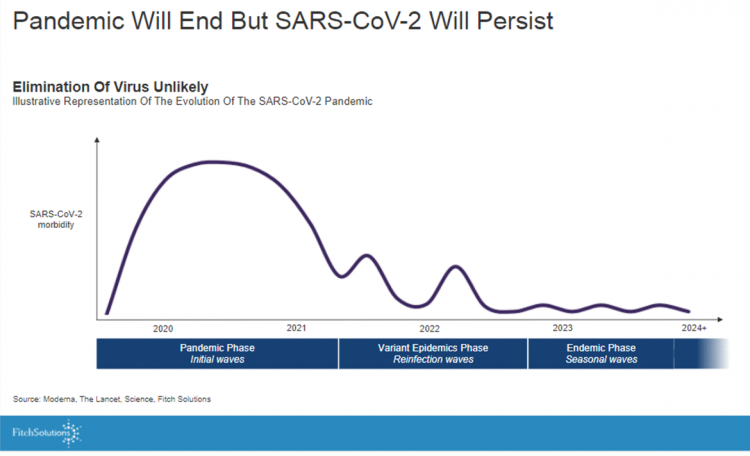
Getting totally rid of the coronavirus isn’t likely, so we humans must accept the fact that SARS-CoV-2 will be endemic. The economic and healthcare system impacts of this were explored in the Post-Covid Healthcare Landscape, delivered by Fitch Solutions’ Jamie Davies and Beau Noafshar, leaders in the Pharmaceuticals, Healthcare, and Medical Devices groups. I welcomed the opportunity to learn from this team’s approach in weaving together the dynamic issues that help us to plan for the long-tail of COVID-19 and its impact on the economy and prospects for the health care industry and health citizens. The first graph illustrates the
What Do Democrats and Republicans Agree On? Allowing Negotiations to Lower Rx Prices
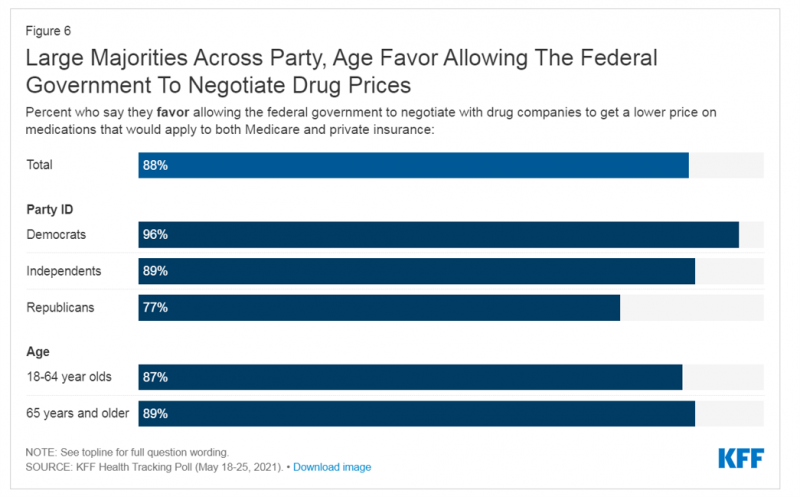
People living in the U.S. have weathered over fifteen months of life-shifts for work, school, prayer, fitness, and social lives. So you might think that the most important public priority for Congress might have something to do with COVID-19, vaccines, or health insurance coverage. But across all priorities, it turns out that prescription drug costs rank higher in Americans’ minds than any other issue in the Kaiser Family Foundation Health Tracking Poll for May 2021. Two-thirds of U.S. adults said that allowing the federal government and private insurance plans to negotiate for lower prices on Rx drugs was their top
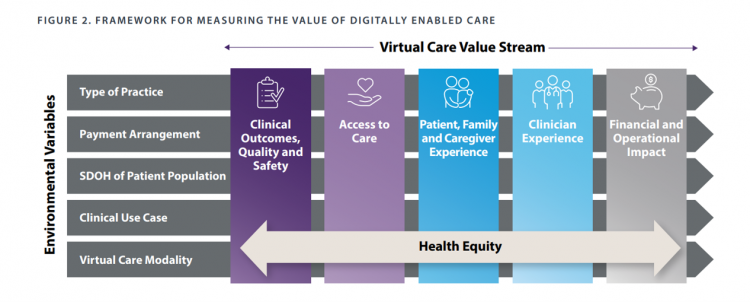
The ROI on Virtual Care – Thinking About Value and Future Prospects With the AMA
When a new technology or product starts to get used in a market, it follows a diffusion curve whose slope depends on the pace of adoption in that market. For telehealth, that S-curve has had a very long and fairly flat front-end of the “S” followed by a hockey stick trajectory in March and April 2020 as the COVID-19 pandemic was an exogenous shock to in-person health care delivery. The first chart from the CDC illustrates that dramatic growth in the use of telehealth ratcheting up since the first case of COVID-19 was diagnosed in the U.S. Virtual care has
And the Oscar Goes To….Power to the Patients!
Health care has increased its role in popular culture over the years. In movies in particular, we’ve seen health care costs and hassles play featured in plotlines in As Good as it Gets [theme: health insurance coverage], M*A*S*H [war and its medical impacts are hell], and Philadelphia [HIV/AIDS in the era of The Band Played On], among dozens of others. And this year’s Oscar winner for leading actor, Anthony Hopkins, played The Father, who with his family is dealing with dementia. [The film, by the way, garnered six nominations and won two]. When I say “Oscar” here on the Health
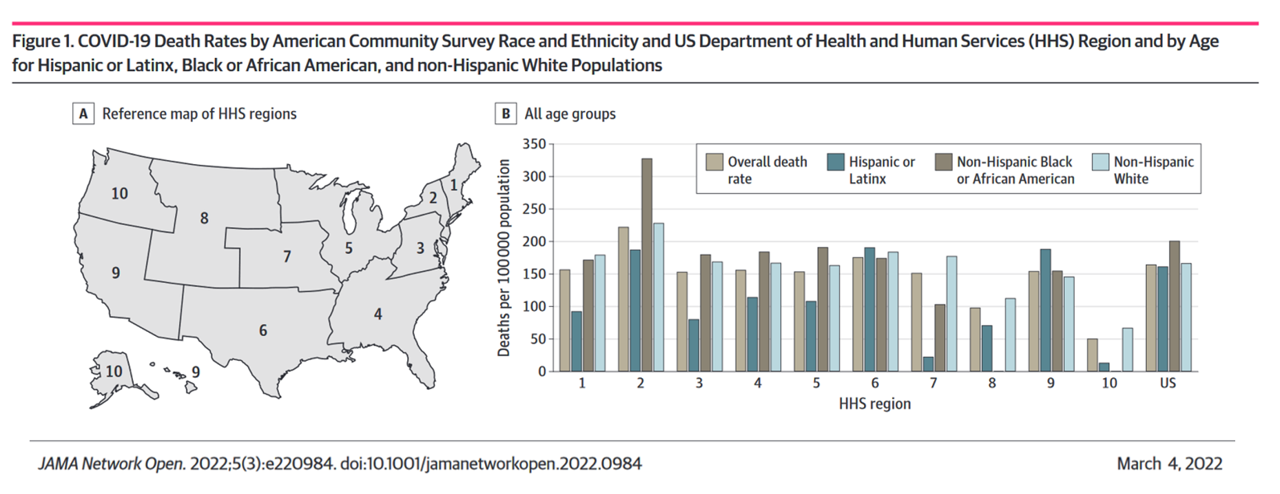
Health Disparities and the Risks of Social Determinants for COVID-19 – 14 Months of Evidence
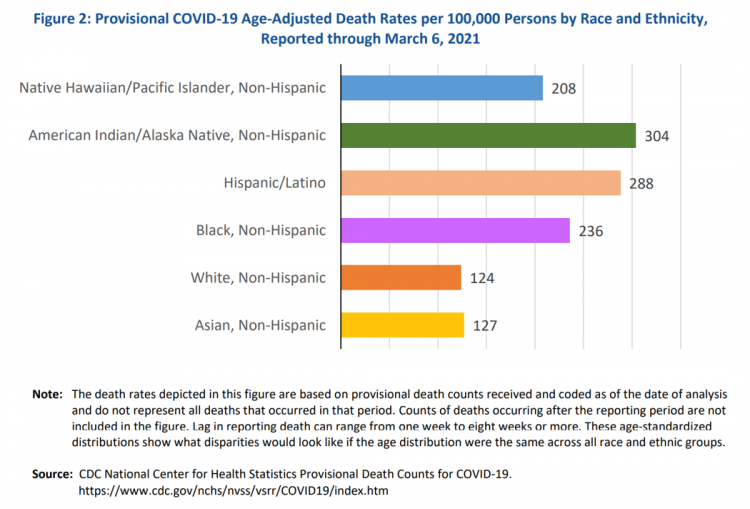
In April 2020, the U.S. Centers for Disease Control issued a report featuring evidence that in the month of March 2020, the coronavirus pandemic was not an equal-opportunity killer. Within just a couple of months of COVID-19 emerging in America, it became clear that health disparities were evident in outcomes due to complications from the coronavirus. An update from that early look at differences in COVID-19 diagnoses and mortality rates was published in Health Disparities by Race and Ethnicity During the COVID-19 Pandemic: Current Evidence and Policy Approaches, In this report, the Assistant Secretary for Planning and Evaluation, part of
Virtual Health Tech Enables the Continuum of Health from Hospital to Home

In the COVID-19 pandemic, as peoples’ daily lives shifted closer and closer to home, and for some weeks and months home-all-the-time, health care, too, moved beyond brick-and-mortar hospitals and doctors’ offices. The public health crisis accelerated “what’s next” for health care delivery, detailed in A New Era of Virtual Health, a report published by TripleTree. TripleTree is an investment bank that has advised health care transactions since 1997. As such, the team has been involved in digital health financing and innovation for 24 years, well before the kind of platforms, APIs, and cloud computing now enabling telehealth and care, everywhere. The
Emerging with A Stronger Healthcare System Post-COVID: NAM’s Lessons Learned
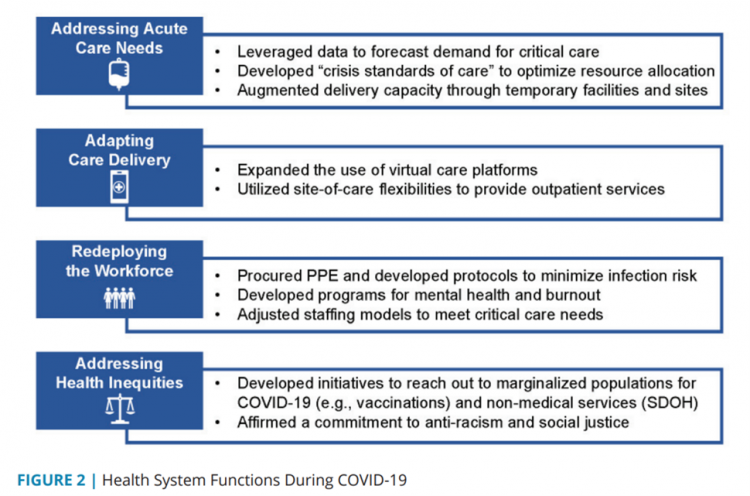
The coronavirus pandemic exposed weaknesses in the U.S. health care system that existed before the public health crisis. What lessons can be learned from the COVID-19 stress-test to build American health care back better? The National Academy of Medicine is publishing nine reports addressing health stakeholder segments impacted and re-shaped by COVID-19 — for public health, quality and safety, health care payers, clinicians, research, patients-families-communities, health product manufacturers, digital health, and care systems. The report on health care systems and providers was released this week: COVID-19 Impact Assessment: Lessons Learned and Compelling Needs was authored by experts on the front-line
The Cost of Healthcare Can Drive Medical Rationing and Crowd Out Other Household Spending
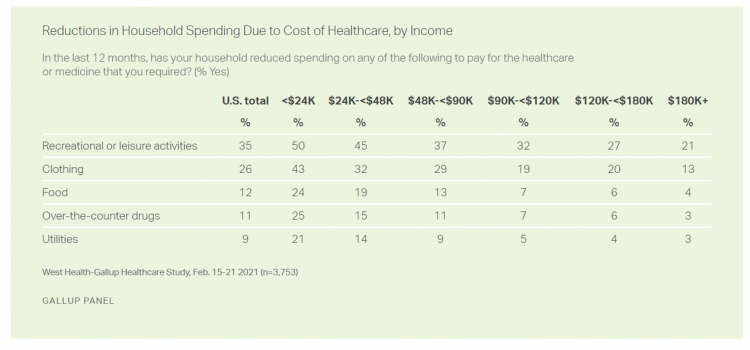
One in five people in the U.S. cannot afford to pay for quality health care — an especially acute challenge for Black and Hispanic Americans, according to a West Health-Gallup poll conducted in March 2021, a year into the COVID-19 pandemic. “The cost of healthcare and its potential ramifications continues to serve as a burdensome part of day-to-day life for millions of Americans,” the study summary observed. Furthermore, “These realities can spill over into other health issues, such as delays in diagnoses of new cancer and associated treatments that are due to forgoing needed care,” the researchers expected. The first table
How Fruits and Veg Can Make Health and Lower Costs – Calling Chef José Andrés to the White House
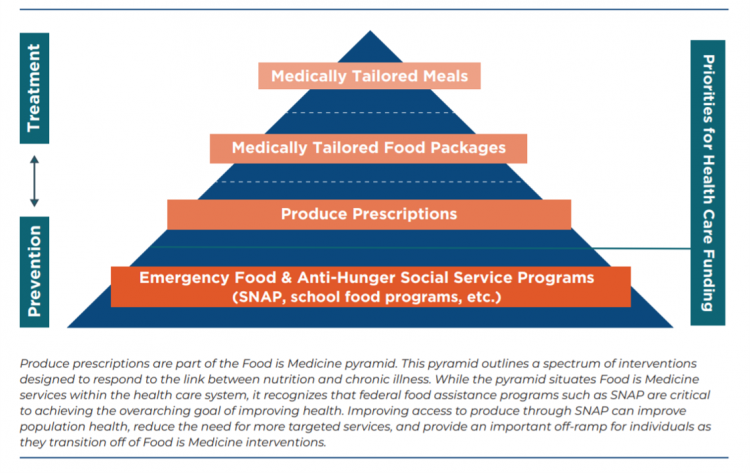
Springtime is finally emerging on the east coast of the U.S. and my local CSA farm is on my mind. It’s timely, then, to re-visit a research paper on subsidizing fruits and vegetables from a March 2019 issue of PLOS as an introduction to a new initiative growing out of The Center for Health Law and Policy Innovation of Harvard Law School (CHLPI) on produce prescriptions. Timely, too, that Chef José Andrés has been called to President Biden’s White House to help address food security in America. First, let’s look at the research in PLOS: Cost-effectiveness of financial incentives for
A BA Degree as Prescription for a Longer Life – Update on Deaths of Despair from Deaton and Case
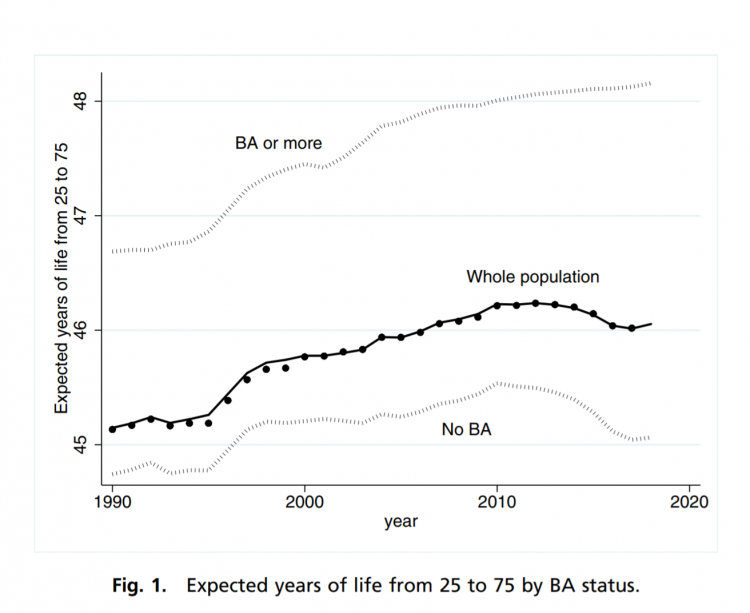
“Without a four-year college diploma, it is increasingly difficult to build a meaningful and successful life in the United States,” according to an essay in PNAS, Life expectancy in adulthood is falling for those without a BA degree, but as educational gaps have widened, racial gaps have narrowed by Anne Case and Angus Deaton. Case and Deaton have done extensive research on the phenomenon of Deaths of Despair, the growing epidemic of mortality among people due to accidents, drug overdoses, and suicide. Case and Deaton wrote the book on Deaths of Despair (detailed here in Health Populi), Case and Deaton
How to Restore Americans’ Confidence in U.S. Health Care: Deal With Access and Cost
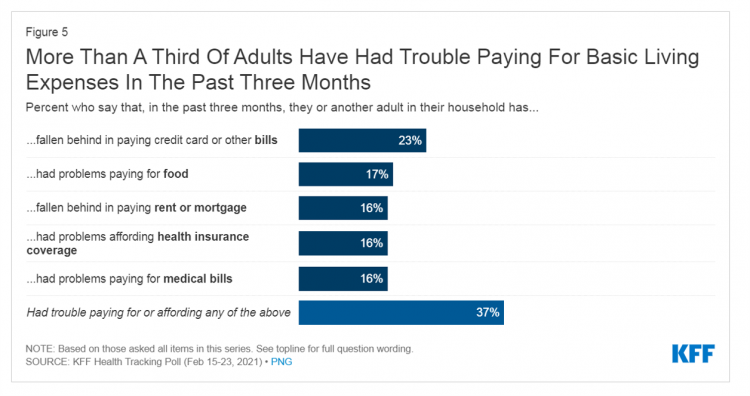
With a vaccine supply proliferating in the U.S. and more health citizens getting their first jabs, there’s growing optimism in America looking to the next-normal by, perhaps, July 4th holiday weekend as President Biden reads the pandemic tea leaves. But that won’t mean Americans will be ready to return to pre-pandemic health care visits to hospital and doctor’s offices. Now that hygiene protocols are well-established in health care providers’ settings, at least two other major consumer barriers to seeking care must be addressed: cost and access. The latest (March 2021) Kaiser Family Foundation Tracking Poll learned that at least one
“Hope Springs Eternal” With the COVID Vaccine for Both Joe Biden and Most People in the U.S.
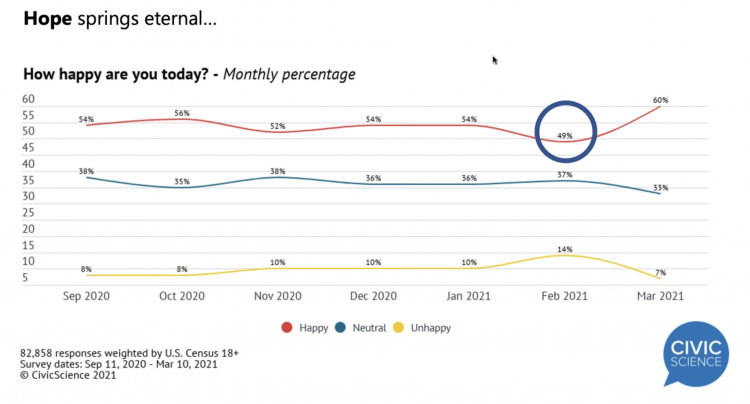
More Americans are happier in March 2021 than they’ve been for a year, based on consumer research from Civic Science polling U.S. adults in early March 2021. For the first time, a larger percent of Americans said they were better off financially since the start of the pandemic. This week, Civic Science shared their latest data on what they’re seeing beyond the coronavirus quarantine era to forecast trends that will shape a post-COVID America. Buoying peoples’ growing optimism was the expectation of the passage of the American Cares Act, which President Biden signed into effect yesterday. The HPA-CS Economic Sentiment Index
Value-Based Health Care Needs All Stakeholders at the Table – Especially the Patient

2021 is the 20th anniversary of the University of Michigan Center for Value-Based Insurance Design (V-BID). On March 10th, V-BID held its annual Summit, celebrating the Center’s 20 years of innovation and scholarship. The Center is led by Dr. Mark Fendrick, and has an active and innovative advisory board. [Note: I may be biased as a University of Michigan graduate of both the School of Public Health and Rackham School of Graduate Studies in Economics]. Some of the most important areas of the Center’s impact include initiatives addressing low-value care, waste in U.S. health care, patient assistance programs, Medicare
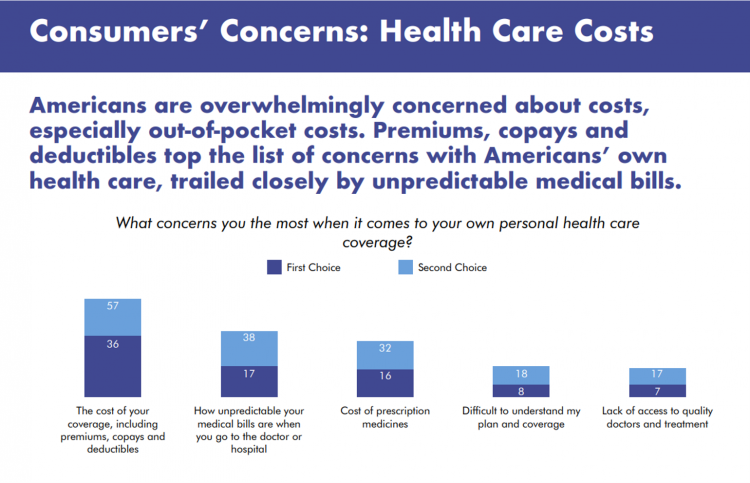
The Economics of the Pandemic Put Costs at the Top of Americans’ Health Reform Priorities
A major side-effect of the coronavirus pandemic in 2020 was its impact on the national U.S. economy, jobs, and peoples’ household finances — in particular, medical spending. In 2021, patients-as-health-consumers seek lower health care and prescription drug costs coupled with higher quality care, discovered by the patient advocacy coalition, Consumers for Quality Care. This broad-spanning patient coalition includes the AIMED Alliance, Autism Speaks, the Black AIDS Institute, Black Women’s Health Initiative, Center Forward, Consumer Action. Fair Foundation, First Focus, Global Liver Institute, Hydrocephalus Association, LULAC, MANA (a Latina advocacy organization), Myositis Association, National Consumers League, National Health IT Collaborative, National Hispanic
The Most Relevant Companies in Health Care – Learning from the W2O Group
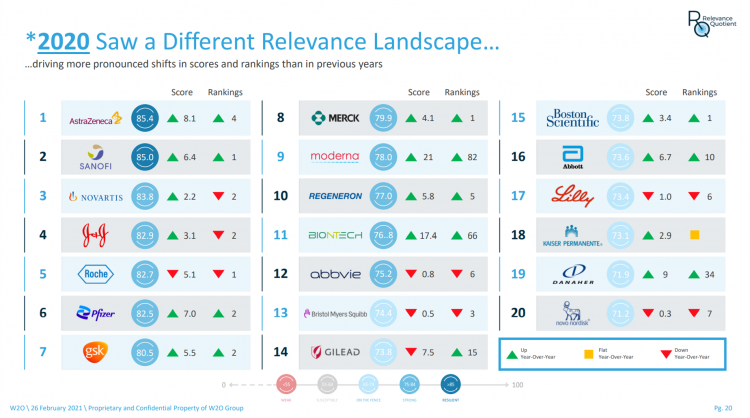
Five years ago, in 2016, the W2O Group said that, “Relevance is reputation.” That year the firm began to study the relevance of, well, relevance for organizations especially operating in the health/care ecosystem. 2020 changed everything, the W2O team asserts, now issuing its latest look into the issue through the Relevance Quotient. Relevance is built on recognizing, meeting and exceeding stakeholder expectations of organizations. In the Relevance Quotient methodology, W2O Group defines key stakeholders as employees, patients (including the sick and the well, caregivers, consumers, et al), health care providers, advocacy groups, analysts and investors, policy makers, journalists and media outlets.
The Remarkable Rise of Pharma’s Reputation in the Pandemic
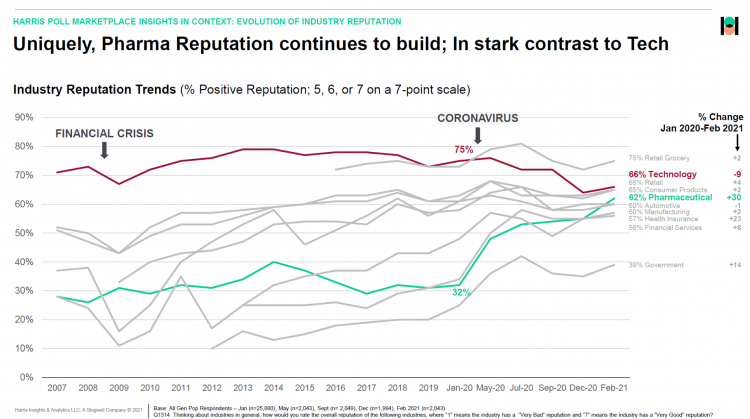
The reputation of the pharmaceutical industry gained a “whopping” 30 points between January 2020 and February 2021, based on the latest Harris Poll in their research into industries’ reputations. The study was written up by Beth Snyder Bulik in FiercePharma. Beth writes that, “a whopping two-thirds of Americans now offer a thumbs-up on pharma” as the title of her article, calling out the 30-point gain from 32% in January 2020 to 62% in February 2021. Thanks to Rob Jekielek, Managing Director of the Harris Poll, for sharing this graph with me for us to understand the details comparing pharma’s to
Americans Lost Future Life-Years in 2020: How Much Life Was Lost Depends on the Color of One’s Skin
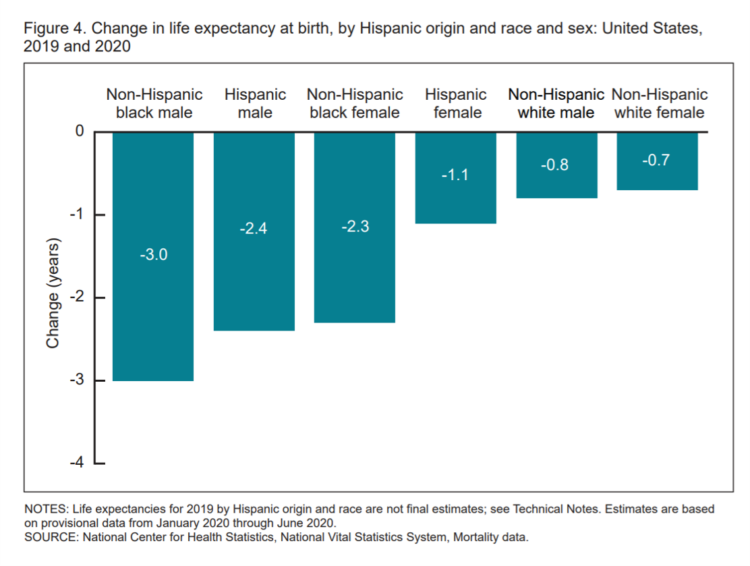
Some people remark about 2020 being a “lost year” in the wake of the coronavirus pandemic. That happens to be a true statement, sadly not in jest: in the U.S., life expectancy at birth fell by one full year over the first half of 2020 compared with 2019, to 77.8 years. In 2019, life expectancy at birth was 78.8 years, according to data shared by the National Center for Health Statistics (NCHS), part of the Centers for Disease Control and Prevention (CDC). Life expectancy at birth declined for both females and males, shown in the first chart. The differences between
Most Americans Want a Vaccine, Dissatisfied with the Rollout
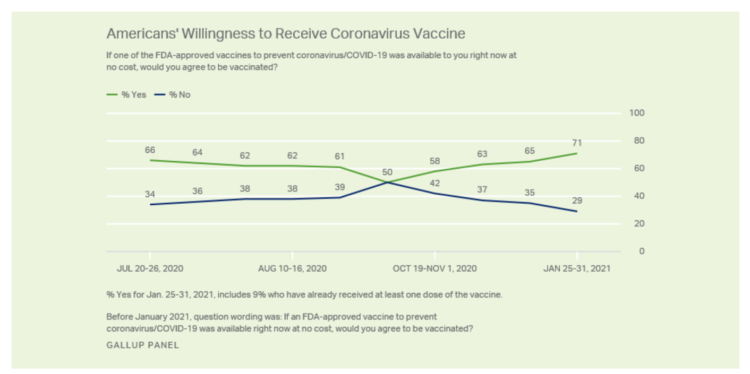
Seven in 10 U.S. adults are willing to be vaccinated, and they’re not happy about the process in getting their jab, according to Gallup’s poll taken in the last week of January 2021. The proportion of Americans willing to receive a COVID-19 vaccine has steadily grown since October 2020, which fell to a mere 50% of folks keen to get the shot. That percentage has risen to 71% as of February 1 2021, as the first line chart shows the reversal in public embrace for vaccination against the coronavirus. Now that most people in the U.S. welcome the opportunity to
The Health Care Cost Curve is Bending Down – A New View from Deloitte
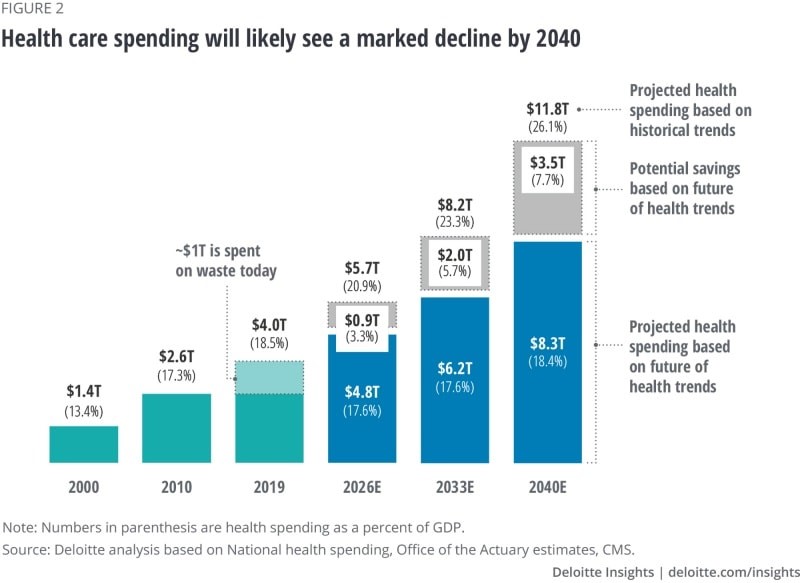
Over the next 20 years, health care spending in the U.S. will migrate toward well-being and the early detection of disease, away from the funding of America’s sick-care system, according to Breaking the cost curve, a forecast of U.S. health economics in the year 2040 from Deloitte. Current spending on health care in America is roughly $4 trillion (with a “t”) dollars, approaching 20% of the nation’s economy. By 2040, spending is projected to be $8.3 trillion based on future health trends — not historic workflows and delivery mechanisms which would consume an additional $3.5 trillion — close to what we
Ten In Ten: Manatt’s Healthcare Priorities to 2031

The coronavirus pandemic has exposed major weaknesses in the U.S. health care system, especially laying bare inequities and inertia in American health care, explained in The Progress We Need: Ten Health Care Imperatives for the Decade Ahead from Manatt Health. The report details the ten objectives that are central to Manatt’s health care practice, a sort of team manifesto call-to-action and North Star for the next decade. Their ten must-do’s for bending the cost curve while driving constructive change for a better health care system are to: Ensure access Achieve health equity Stability the safety net and rebuild public health
Americans A Year Into the Pandemic – A View from Pew
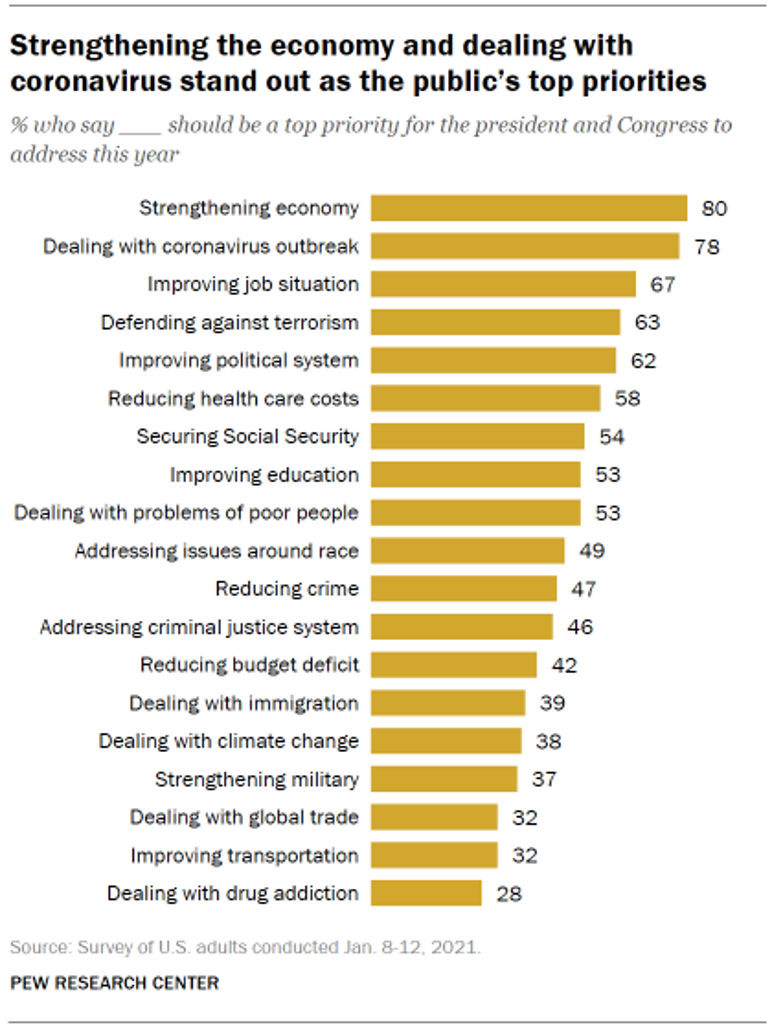
Nearly a year into the COVID-19 pandemic, the same percent of Americans say strengthening the U.S. economy and dealing with the coronavirus outbreak should be a top priority for President Biden and Congress to address this year, according to data from the Pew Research Center collected during the second week of January 2021. Two-thirds of people in the U.S. also want government leaders to prioritize improving the employment situation, defending against terrorism, and improving the political system, the study learned. At Americans’ low end of the priority list for the President and Congress are dealing with global trade, improving transportation,
Call It Deferring Services or Self-Rationing, U.S. Consumers Are Still Avoiding Medical Care
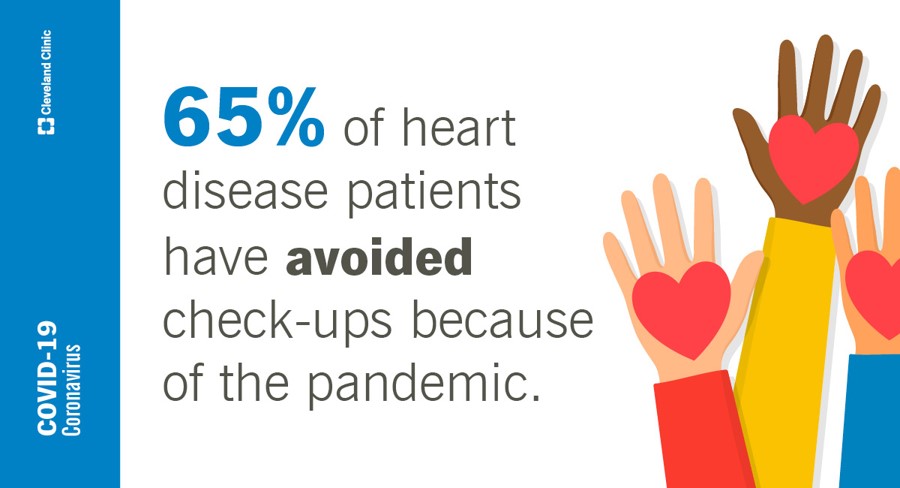
Patients in the U.S. have been self-rationing medical care for many years, well before any of us knew what “PPE” meant or how to spell “coronavirus.” Nearly a decade ago, I cited the Kaiser Family Foundation Health Security Watch of May 2012 here in Health Populi. The first chart here shows that one in four U.S. adults had problems paying medical bills, largely delaying care due to cost for a visit or for prescription drugs. Fast-forward to 2020, a few months into the pandemic in the U.S.: PwC found consumers were delaying treatment for chronic conditions. In October 2020, The American Cancer
Can Telemedicine Increase Health Equity? A Conversation with Antoinette Thomas, Dave Ryan, and Me with the ATA

“Yes,” we concurred on our session convened by the American Telemedicine Association (ATA) EDGE session today. “We” was a trio including Antoinette Thomas (@NurseTechExec1), Chief Patient Experience Officer with Microsoft, David Ryan (@DavidPRyan), former long-time Global Head of Intel’s Health/Life Science business; and, me. Antoinette posed three questions for all of us to brainstorm, addressing various aspects of health equity. We covered, The theory that telemedicine should increase health equity — where are we and what are the barriers to getting there? The role of social determinants of health in creating equitable opportunities for health citizens; and, Entering a post-pandemic world,
Food Trends and Hunger in the Pandemic – the Importance of Food Security in Health and Economic Security
In 2020, the COVID-19 pandemic changed all kinds of aspects of our daily lives, not the least of which were our food habits — how we shopped for food, how we bought food, how we cooked and baked from scratch, and how our tastes and nutritional choices changed with our #StayHome and #WorkFromHome lifestyles. People who could keep their jobs and work from home connected by broadband learned how to build up pandemic pantries, shop online, and stay well-fed. But for people in the U.S. who lost employment, had hours cut, or were compelled to stay home to teach kids
Addressing Lives and Livelihoods with a Whole-of-Government Approach – The First Wave of Biden Health Policy
President Biden’s first few days on the job gave us a very clear view on how he sees conquering COVID: through a whole-of-government approach to public policies that bolster directly addressing the virus, along with the many forces shaping how we got here and how to come out of the pandemic era stronger. I cover this first wave of Biden health policy in my latest post for the Medecision Liberation blog titled, “Top Priorities for President Biden: COVID-19, Then Everything Else.” The plotline goes… On the day of inauguration, January 20, 2021, Joseph R. Biden was installed as the 46th
The Biden Administration’s Whole-of-Government Approach to Equity – in Health and Beyond
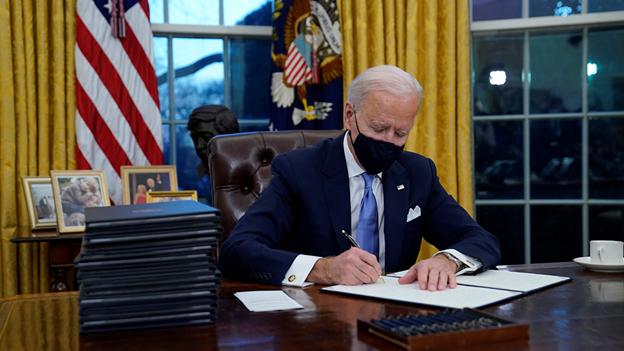
In the U.S., the COVID-19 pandemic has revealed disparities in housing, food, and job security, and the role that one’s ZIP code and social determinants play in health outcomes. Overall, America has done poorly in light of being 4% of the world’s population but having one-fifth of the planet’s deaths due to the coronavirus. But these have disproportionately hit non-white people, who are nearly three times as likely to die from COVID-19 than white Americans. I’ve been head-down reviewing the first two days of President Biden’s signing Executive Orders, reading the National Strategy for COVID-19 Response, and inventorying line items
Our Homes Are Health Delivery Platforms – The New Home Health/Care at CES 2021

The coronavirus pandemic disrupted and re-shaped the annual CES across so many respects — the meeting of thousands making up the global consumer tech community “met” virtually, both keynote and education sessions were pre-recorded, and the lovely serendipity of learning and meeting new concepts and contacts wasn’t so straightforward. But for those of us working with and innovating solutions for health and health care, #CES2021 was baked with health goodness, in and beyond “digital health” categories. In my consumer-facing health care work, I’ve adopted the mantra that our homes are our health hubs. Reflecting on my many conversations during CES
Trust Plummets Around the World: The 2021 Edelman Trust Barometer in #CES2021 and Microsoft Context
Citizens around the world unite around the concept that Trust is Dead. This is no truer than in the U.S., where trust in every type of organization and expert has plummeted in the wake of the COVID-19 pandemic, political and social strife, and an economic downturn. Welcome to the sobering 2021 Edelman Trust Barometer, released this week as the world’s technology innovators and analysts are convening at CES 2021, and the annual JP Morgan Healthcare meetup virtually convened. As the World Economic Forum succinctly put the situation, “2020 was the year of two equally destructive viruses: the pandemic and the
The Digital Consumer, Increasingly Connected to Health Devices; Parks Associates Kicking Off #CES2021

In 2020, the COVID-19 pandemic drove U.S. consumers to increase spending on electronics, notably laptops, smartphones, and desktop computers. But the coronavirus era also saw broadband households spending more on connecting health devices, with 42% of U.S. consumers owning digital health tech compared with 33% in 2015, according to research discussed in Supporting Today’s Connected Consumer from Parks Associates. developed for Sutherland, the digital transformation company. Consumer electronics purchase growth was, “likely driven by new social distancing guidelines brought on by COVID-19, which requires many individuals to work and attend school from home. Among the 26% of US broadband households
“The virus is the boss” — U.S. lives and livelihoods at the beginning of 2021
“The virus is the boss,” Austan Goolsbee, former Chair of the Council of Economic Advisers under President Obama, told Stephanie Ruhle this morning on MSNBC. Goolsbee and Jason Furman, former Chair of Obama’s Council of Economic Advisers, tag-teamed the U.S. economic outlook following today’s news that the U.S. economy lost 140,000 jobs — the greatest job loss since April 2020 in the second month of the pandemic. The 2020-21 economic recession is the first time in U.S. history that a downturn had nothing to do with the economy per se. As Uwe Reinhardt, health economist guru, is whispering in my
The 2021 Shkreli Awards: Lown Institute Counts Down the Top 10 Healthcare Industry Abuses in the Coronavirus Pandemic

The first year of the coronavirus pandemic in America was a kind of stress test on the U.S. health care system, revealing weak links and opportunities for bad behavior. “These are not just about individual instances or bad apples,” Dr. Vikas Saini, President of The Lown Institute, explained, referring to them as “cautionary tales” of the current state of U.S. health care. Dr. Saini and his colleague Shannon Brownlee released the annual Lown Institute 2020 Shkreli Awards this week, highlighting their ten most egregious examples of the worst events in U.S. health care that happened in the past year —
Nurses, doctors, pharmacists join with teachers in Gallup’s 2021 honest and ethics poll
Each year, Americans rank nurses as the most honest and ethical professionals along, generally followed by doctors and pharmacists. In the middle of the coronavirus pandemic in the U.S., grade school teachers join the three medical professions in the annual Gallup Poll on the top-ranked professions for honest and ethical behavior in America as we enter 2021 with many U.S. hospitals’ intensive care units at full capacity….and schools largely emptied of students. The three health care professions scored their highest marks ever achieved in this Gallup Poll, which has been assessing honesty and ethics in America since 1999. Nurses are
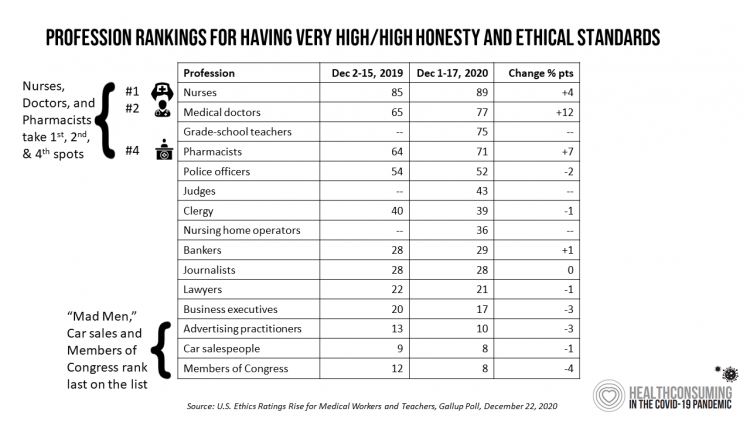
The Comforts of Home Drive Demand for Healthcare There
Two in three U.S. consumers skipped or delayed getting in-person medical care in 2020. One in 2 people had a telehealth visit int he last year. Most would use virtual care again. The coronavirus pandemic has mind-shifted how patients envision a health care visit. Today, most consumers prefer the idea of getting health care at home compared with going to a doctor’s office. Most Americans also like the idea of recovering at home instead of at a medical facility after a major medical event, according to the report, Health-at-Home 2020: The New Standard of Care Delivery from CareCentrix. COVID-19 has
Vaccine Hesitancy Is Greatest Among Those at Highest Risk of Dying from COVID-19: Black People
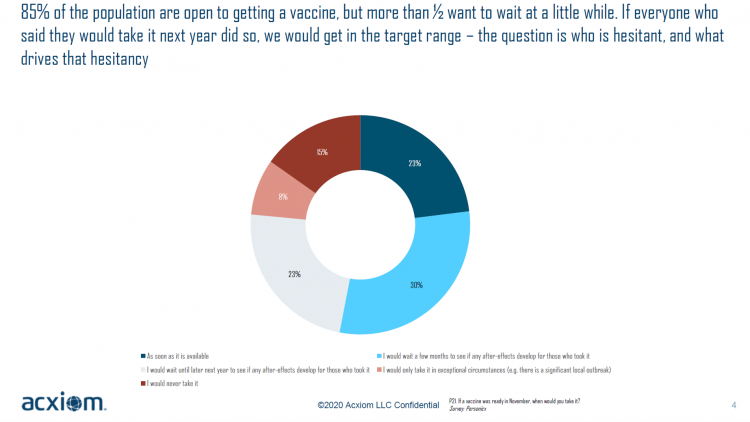
While 85% of people are open to receiving a COVID-19 vaccine, over one-half of them would want to wait some time to observe if after-effects developed in people who took the jab, according to a new study from Acxiom, the data analytics-marketing company. Not all people are as enthused about getting a coronavirus vaccine at all, Acxiom discovered: in fact, those hardest hit by the virus — Black people — would be the least-likely to want to get a COVID-19 vaccine, discussed in in Vaccine Hesitancy in the U.S., a survey the company conducted among 10,000 people in the U.S.
The COVID Healthcare Consumer – 5 Trends Via The Medecision Liberation Blog
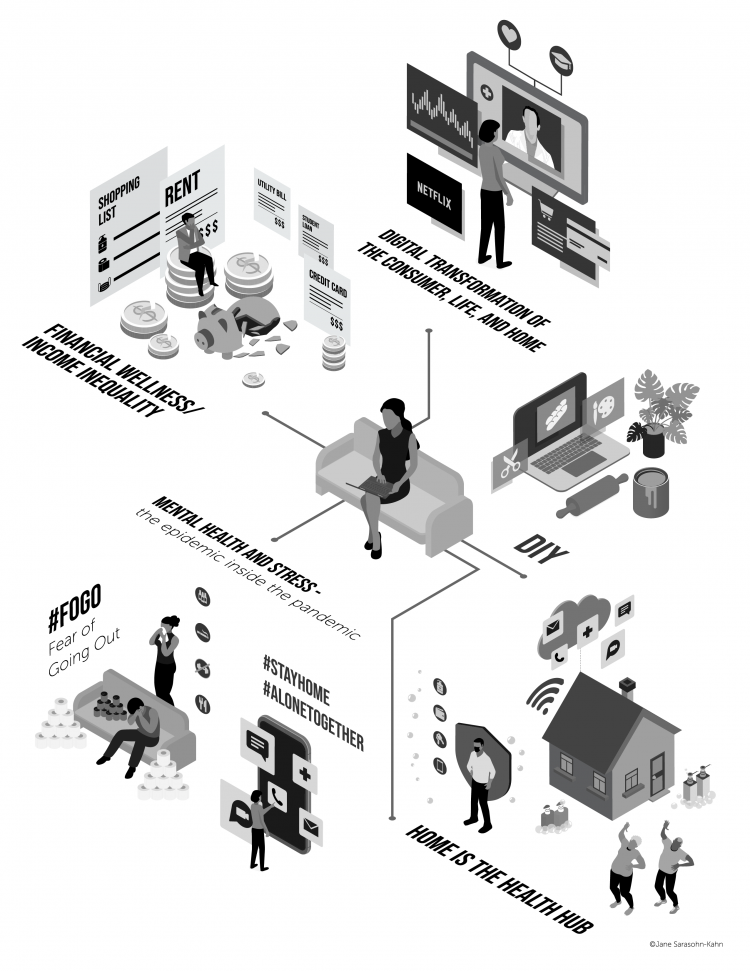
The first six months into the coronavirus pandemic shocked the collective system of U.S. consumers for living, learning, laboring, and loving. I absorbed all kinds of data about consumers in the wake of COVID-19 between March and mid-August 2020, culminating in my book, Health Citizenship: How a virus opened hearts and minds, published in September on Kindle and in print in October. In this little primer, I covered the five trends I woven based on all that data-immersion, following up the question I asked at the end of my previous book, HealthConsuming: when and how would Americans claim their health
Rebuilding Resilience, Trust, and Health – Deloitte’s Latest on Health Care and Sustainability
The COVID-19 pandemic has accelerated health care providers’ and plans’ investment in digital technologies while reducing capital spending on new physical assets, we learn in Building resilience during the COVID-19 pandemic and beyond from the Deloitte Center for Health Solutions. What must be built (or truly re-built), health care leaders believe, is first and foremost trust, followed by financial viability to ensure long-term resilience and sustainability — for the workforce, the organization, the community, and leaders themselves. For this report, Deloitte interviewed 60 health care chief financial officers to gauge their perspectives during the pandemic looking at the future of
Will We See A Field of Dreams for the COVID-19 Vaccine in the U.S.?
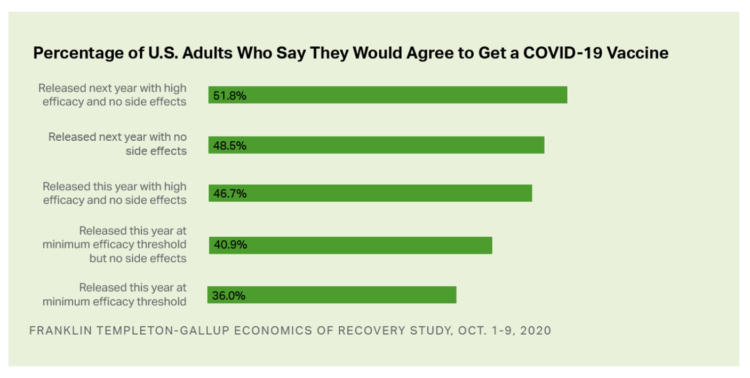
“If you build it, he will come,” the voice of James Earl Jones echoes in our minds when we recall the plotline of the film, Field of Dreams. A quick summary if you don’t know the movie: the “it” was a baseball field to be built in a rural cornfield. The “he” was a baseball player, ultimately joined by a dream-team of ball players who would convene on that dreamy field to play an amazing game. Today, the day after Pfizer announced a 90% benefit for its coronavirus vaccine, bolstering Wall Street returns on 9th November 2020, two new consumer
Voting for Health in 2020

In the 2018 mid-term elections, U.S. voters were driven to polls with health care on their minds. The key issues for health care voters were costs (for care and prescription drugs) and access (read: protecting pre-existing conditions and expanding Medicaid). Issue #2 for 2018 voters was the economy. In 2020, as voting commences in-person tomorrow on 3rd November, U.S. voters have lives and livelihoods on their minds. It’s the pandemic – our physical lives looming largest in the polls – coupled with our fiscal and financial lives. Health is translating across all definitions for U.S. voters in November 2020: for
Masks Work. A Picture From Kansas That Tells A Story in Two Words.
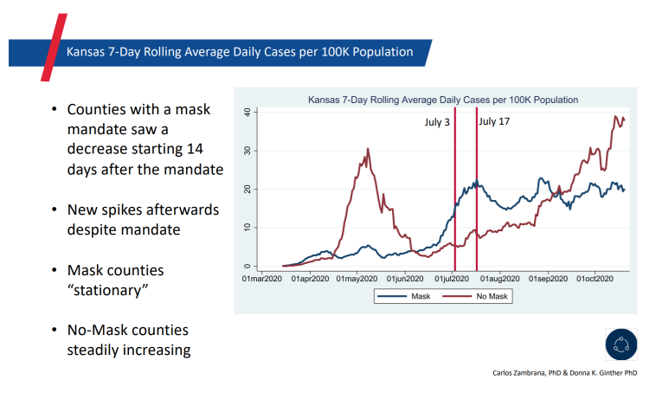
It is said that a picture tells a thousand words. This picture tells an even quicker story that can save lives: “Masks work.” The backstory: Kansas Governor Laura Kelly issued a mask mandate on July 2, 2020. The rationale: That was two days before Independence Day, the holiday weekend when she and state public health officials anticipated health citizens would abandon their personal efforts to physically distance and cover faces to avoid contracting or spreading the coronavirus. This was the message directly communicated to U.S. residents by the White House Coronavirus Task Force that week before Independence Day. The backlash:
Health Care Providers Are More Politically Engaged in the 2020 Elections
Until 2016, physicians’ voting rates in U.S. elections had not changed since the late 1970s. Then in 2018, two years into President Donald Trump’s four-year term, the mid-term elections drove U.S. voters to the election polls…including health care providers. Based on the volume and intensity of medical professional societies’ editorials on the 2020 Presidential Election, we may be in an inflection-curve moment for greater clinician engagement in politics as doctors and nurses take claim of their health citizenship. A good current example of this is an essay published in the AMA’s website asserting, “Why it’s okay for doctors to ask
Stress in America, Like COVID-19, Impacts All Americans
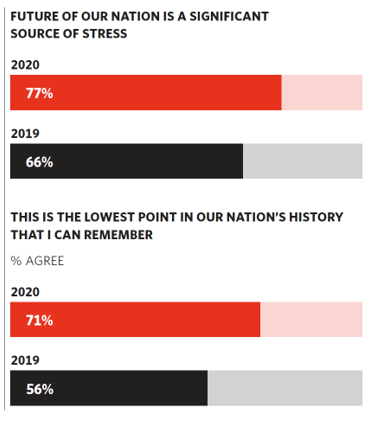
With thirteen days to go until the U.S. #2020Elections day, 3rd November, three in four Americans say the future of America is a significant source of stress, according to the latest Stress in America 2020 study from the American Psychological Association. Furthermore, seven in 10 U.S. adults believe that “now” is the lowest point in the nation’s history that they can remember. “We are facing a national mental health crisis that could yield serious health and social consequences for years to come,” APA introduces their latest read into stressed-out America. Two in three people in the U.S. say that the
Women’s Health Policy Advice for the Next Occupant of the White House: Deal With Mental Health, the Pandemic, and Health Care Costs
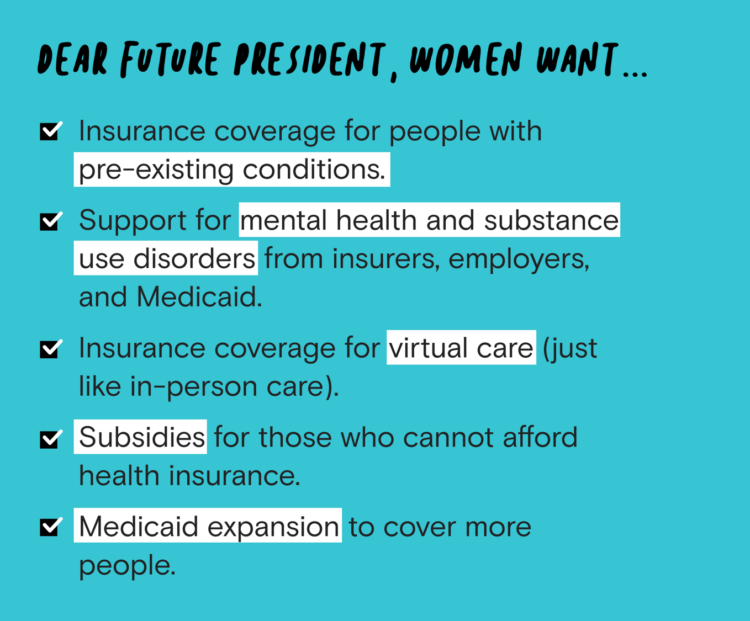
2020 marked the centennial anniversary of the 19th Amendment to the U.S. Constitution, giving women the right to vote. In this auspicious year for women’s voting rights, as COVID-19 emerged in the U.S. in February, women’s labor force participation rate was 58%. Ironic timing indeed: the coronavirus pandemic has been especially harmful to working women’s lives, the Brookings Institution asserted last week in their report in 19A: The Brookings Gender Equality Series. A new study from Tia, the women’s health services platform, looks deeply into COVID-19’s negative impacts on working-age women and how they would advise the next occupant of
Black Health Should Matter More in America: The Undefeated Survey on Race and Health
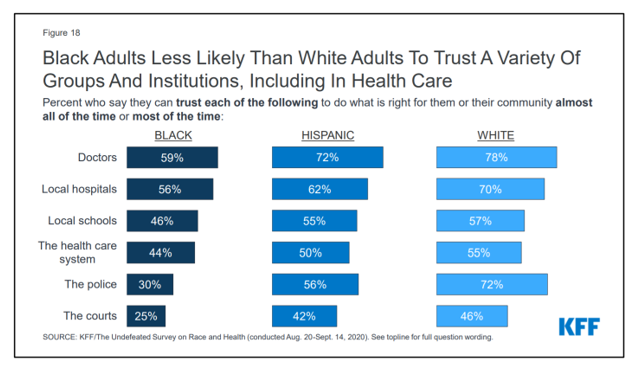
In 2020, most Black people, men and women alike, feel it is a bad time to be Black in America. More than twice as many Black men believed that in 2020 compared with 2006. More than four times as many Black women believed that it’s a bad time to be Black in America in 2020 versus 2011, we learn in The Undefeated Survey on Race and Health from Kaiser Family Foundation (KFF). KFF collaborated with The Undefeated, ESPN’s project that focuses on sports, race, and culture. The Undefeated program was started in May 2016, and has become a thought leader
Two in Three Americans Cite the U.S. Presidential Election is a Significant Source of Stress, Even More than the 2016 Race
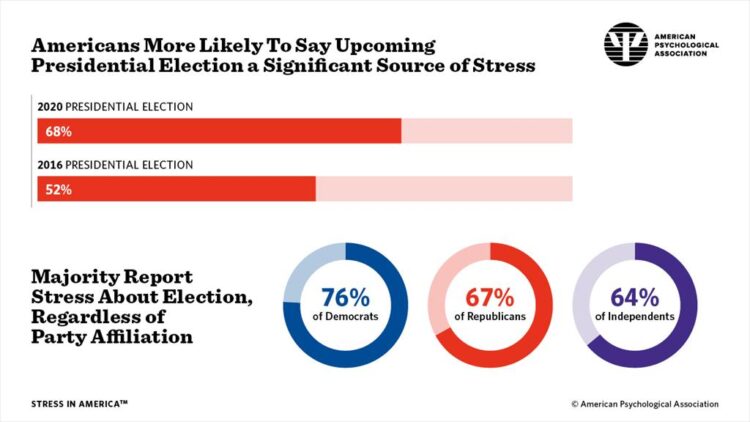
If you perceive you are more stressed in the COVID-19 pandemic than you were in 2019, you are one in many millions feeling so. If you felt stressed during the 2016 Presidential election season, you were also one in a million. Now, as the 2020 Election converges with the coronavirus crisis, even more Americans are feeling significant stress in a double-whammy impact. Our friends at the American Psychological Association have assessed Stress in America for many years of studies. The latest, published 7 October, finds that the 2020 Presidential election is a source of significant stress for more Americans than
In the Past Ten Years, Workers’ Health Insurance Premiums Have Grown Much Faster Than Wages
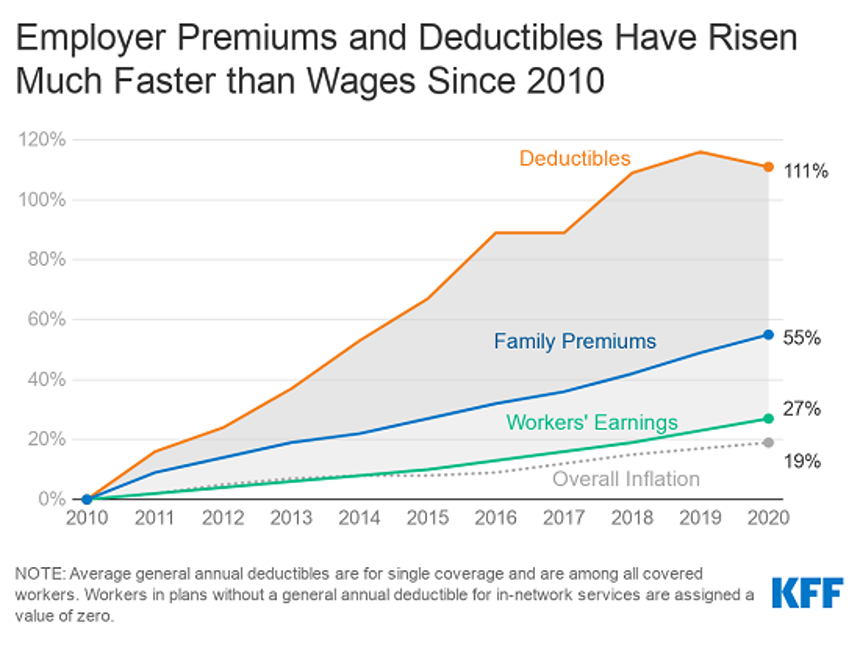
For a worker in the U.S. who benefits from health insurance at the workplace, the annual family premium will average $21,342 this year, according to the 2020 Employer Health Benefits Survey from the Kaiser Family Foundation. The first chart illustrates the growth of the premium shares split by employer and employee contributions. Over ten years, the premium dollars grew from $13,770 in 2010 to $21K in 2020. The worker’s contribution share was 29% in 2010, and 26% in 2020. Single coverage reached $7,470 in 2020 and was $5,049 in 2010. Roughly the same proportion of companies offered health benefits to
Financial Health Is On Americans’ Minds Just Weeks Before the 2020 Elections
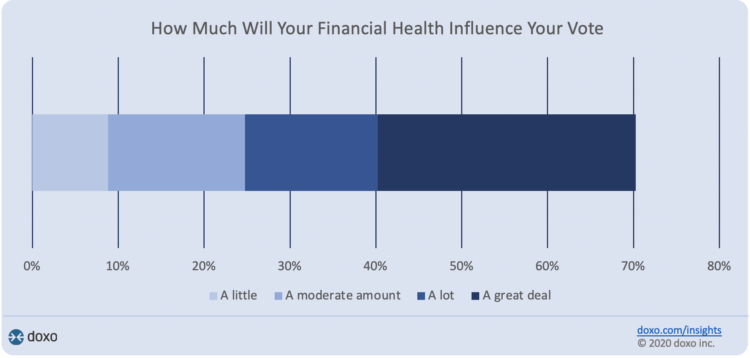
Financial health is part of peoples’ overall health. As Americans approach November 3, 2020, the day of the real-time U.S. Presidential and down-ballot elections, personal home economics are front-of-mind. Twenty-seven days before the 2020 elections, 7 in 10 Americans say their financial health will influence their votes this year, according to the doxoINSIGHTS survey which shows personal financial health as a key voter consideration in the Presidential election. Doxo, a consumer payments company, conducted a survey among 1,568 U.S. bill-paying households in late September 2020. The study has a 2% margin of error. U.S. voters facing this year’s election are
Our Home Is Our Health Hub: CTA and CHI Align to Address Digital and Health Equity

In the pandemic, I’ve been weaving together data to better understand how people as consumers are being re-shaped in daily life across their Maslow Hierarchies of Needs. One of those basic needs has been digital connectivity. People of color have faced many disparities in the wake of the pandemic: the virus itself, exacting greater rates of mortality and morbidity being the most obvious, dramatic inequity. Another has been digital inequity. Black people have had a more difficult time paying for phone and Internet connections during the COVID-19 crisis, we learned in a Morning Consult poll fielded in June 2020. In
The Emergence of Health Citizens – Part of Liberating Health, on the Medecision Blog
I have always appreciated Medecision’s mission as expressed in the company’s tagline: “Liberating,” as in “liberate healthcare.” I began collaborating with Medecision as a client several years ago, a couple of years after I heard Todd Park, then Chief Technology Officer in the White House, joyfully assert the phrase, “Data Liberación!” at an early Health 2.0 Conference. Medecision published my blog about health citizenship this week on the company’s Liberate.Health site. The emergence of health citizens in the U.S. — people re-claiming their health, health care, and control of data — is part of liberating health in America. Please check
Redefining PPE As Primary Care, Public Health, and Health Equity – The Community PPE Index
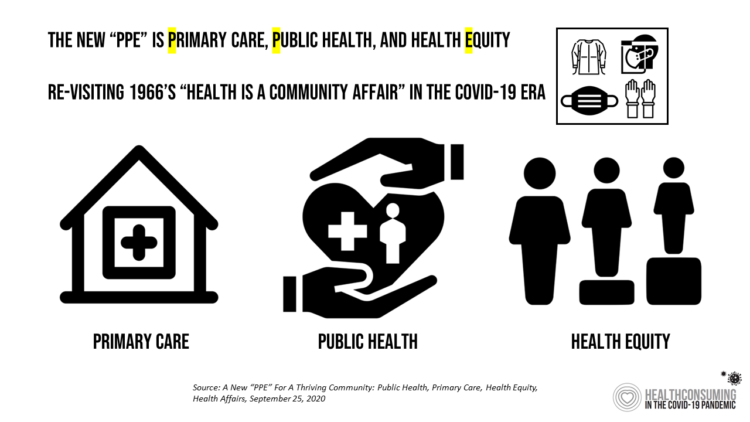
In May 2020, the Oxford English Dictionary (OED) re-visited the acronym, “PPE.” As OED evolves the definition of PPE, the wordsmiths could borrow from OSHA’s website, noting that PPE, “is equipment worn to minimize exposure to hazards that cause serious workplace injuries and illnesses. These injuries and illnesses may result from contact with chemical, radiological, physical, electrical, mechanical, or other workplace hazards. Personal protective equipment may include items such as gloves, safety glasses and shoes, earplugs or muffs, hard hats, respirators, or coveralls, vests and full body suits.” Perhaps Definition 3 in the OED could be updated by a blog
Health Citizenship in America. If Not Now, When?
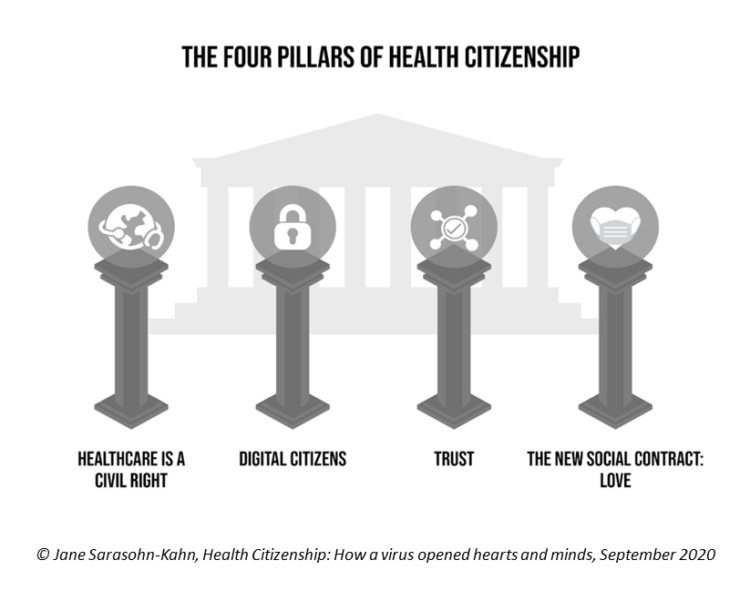
On February 4th, 2020, in a hospital in northern California, the first known inpatient diagnosed with COVID-19 died. On March 11th, the World Health Organization called the growing prevalence of the coronavirus a “pandemic.” On May 25th, George Floyd, a 46-year-old Black man, died at the hands of police in Minneapolis. This summer, the Dixie Chicks dropped the “Dixie” from their name, and NASCAR cancelled the confederate flag from their tracks. Today, nearly 200,000 Americans have died due to the novel coronavirus. My new book, Health Citizenship: How a virus opened hearts and minds, launched this week. In it, I
Only in America: The Loss of Health Insurance as a Toxic Financial Side Effect of the COVID-19 Pandemic

In terms of income, U.S. households entered 2020 in the best financial shape they’d been in years, based on new Census data released earlier this week. However, the U.S. Census Bureau found that the level of health insurance enrollment fell by 1 million people in 2019, with about 30 million Americans not covered by health insurance. In fact, the number of uninsured Americans rose by 2 million people in 2018, and by 1.9 million people in 2017. The coronavirus pandemic has only exacerbated the erosion of the health insured population. What havoc a pandemic can do to minds, bodies, souls, and wallets. By September 2020,
50 Days Before the U.S. Elections, Voters Say Health Care Costs and Access Top Their Health Concerns — More than COVID-19
The coronavirus pandemic has revealed deep cracks and inequities in U.S. health care in terms of exposure to COVID-19 and subsequent outcomes, with access to medical care and mortality rates negatively impacting people of color to a greater extent than White Americans. The pandemic has also led to economic decline that, seven weeks before the 2020 elections in America, is top-of-mind for health citizens with the virus-crisis itself receding to second place, according to the Kaiser Family Foundation September 2020 Health Tracking Poll. KFF polled 1,199 U.S. adults 18 years of age and older between August 28 and September 3,
Behavioral Health Side-Effects in the COVID Era
“This surge of people experiencing acute behavioral health problems…has the potential to further impact the healthcare system for years to come,” a report from McKinsey expects looking at the hidden costs of COVID-19’s impact on U.S. health care. The coronavirus pandemic has taken a toll on Americans’ mental health, with anxiety and depression growing as a side-effect to worries about the virus itself, the long Great Lockdown in much of the country, and the economic recession that has particularly impacted women and people of color. I covered depression impacts due to COVID-19 here in Health Populi yesterday, and wanted to
The Burden of Depression in the Pandemic – Greater Among People With Fewer Resources
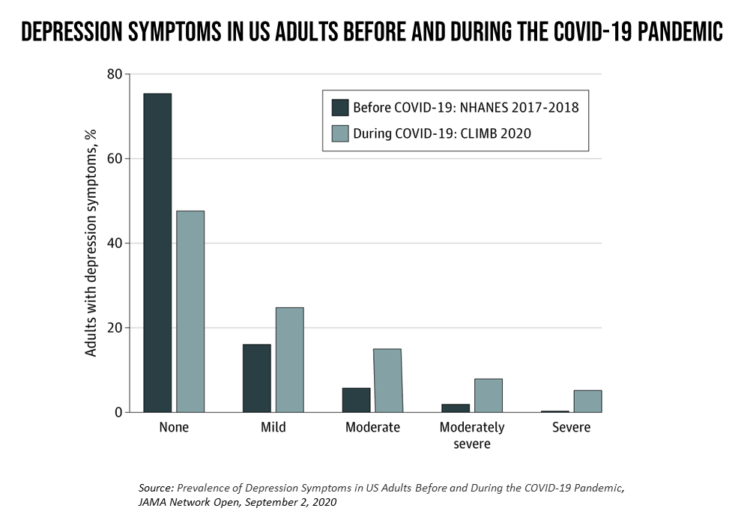
In the U.S., symptoms of depression were three-times greater in April 2020 in the COVID-19 pandemic than in 2017-2018. And rates for depression were even higher among women versus men, along with people earning lower incomes, losing jobs, and having fewer “social resources” — that is, at greater risk of isolation and loneliness. America’s health system should be prepared to deal with a “probable increase” in mental illness after the pandemic, researchers recommend in Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic in JAMA Network Open. A multidisciplinary team knowledgeable in medicine, epidemiology, public health,
The Next-Normal Health Care Consumer After the Pandemic
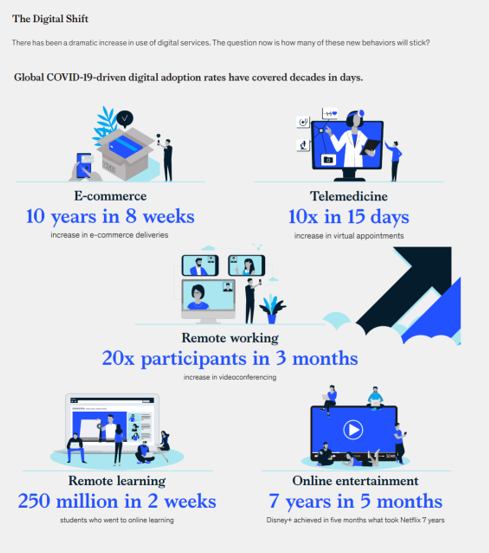
McKinsey invites us to Meet the next-normal consumer in a recently-published research report describing changing consumer behavior responding to the COVID-19 lockdown and aftermath. The report gives us insights into the next-normal health consumer, which I’ll discuss in today’s post. Note the massive digital shift every person living in a country touched by the coronavirus has experienced, illustrated in the first graphic from the report. Tele-work, tele-education, ecommerce, and streaming entertainment all grew so fast within a matter of a few weeks. And telemedicine, McKinsey points out, was adopted at a rate of ten times growth over 15 days, the
Data Well-Being: A Pillar of Health Citizenship for US Consumers
In the COVID-19 era, most U.S. consumers believe they have an obligation to share personal health information to stop the spread of the coronavirus. However, only 44% would be willing to share their personal data with a national database, a MITRE study learned. Only one-third of Americans would be willing to share their temperature, 29% their location, and one-fourth information about their chronic conditions. The Harris Poll conducted the study among 2,065 U.S. adults 18 and over in mid-June 2020 to gauge peoples’ perspectives on health data and privacy. Three-quarters of people in the U.S. believe that data privacy “is a
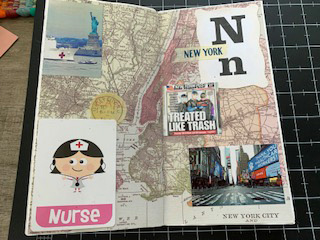
My ABCovid-19 Journal – Day 4 of 5, Letters “P” through “T”
While I’m on holiday this week, restoring and re-setting, I’ve been sharing pages from my ABCovid-19 Journal with readers of Health Populi. I created this journal during the early phase of the pandemic in the U.S., as a form of art therapy, creative outlet, and learning. Today is Day 4 of sharing: we consider the letters “P” through “T,” and what I saw in the early coronavirus era. P is for pandemic This “P” was self-evidence in our collective early COVID-19 lexicon. The “P” word was uttered by the Secretary General of the World Health Organization on March 11, confirming
My ABCovid-19 Journal – Day 3 of 5, Letters “K” through “O”
Welcome back to my ABCovid-19 Journal, which I created/curated in the early weeks of the coronavirus pandemic. This week, I’m sharing all the letters of the alphabet with you which reminded me keywords and themes emerging as we were learning about this dastardly public health threat beginning early in 2020. In today’s Health Populi blog I bring you letters “K” through “O,” continuing through the rest of the alphabet tomorrow and Friday while I’m on a lake-side holiday that’s good for mind, body, and spirit. K is for Kirkland, Washington state In the U.S., one of the earliest hotspots for





 Thank you FeedSpot for
Thank you FeedSpot for