Healthcare, Heal Thyself! How the Industry Can and Should Play the Trust Card
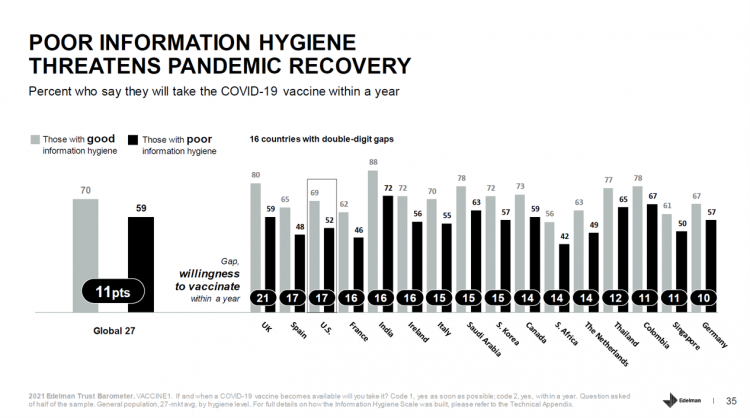
The emergence of the COVID-19 vaccine “infodemic” has slowed the ability for nations around the world to emerge out of the public health crisis. Growing cynicism among some health citizens facing the politicization of public health tactics like vaccines and facial masks is what we’re talking about. At the root is peoples’ lack of trust across a range of information providers, including government, media, business, and even peers. The 2021 Edelman Trust Barometer spotlighted the infodemic and eroding trust in the U.S. in the voices of public health, the public sector, and media. This is a global challenge as well,
Trust in Healthcare is Under Stress in the US and Globally, Edelman Finds
You’re stressed, I’m stressed; most of us have felt stress in the COVID-19 era which began in the U.S. in the first quarter of 2020. Nearly eighteen months later, a 2021 Edelman Trust Barometer update finds that consumers’ trust in the health care industry is under stress, too — in the U.S. and around the world. The first chart from the Edelman health care update demonstrates that in most countries polled, health citizens’ trust in health care was buoyed in the first five months of 2020 (January through May): up 18 points in the U.S., 14 points in Canada and
Health and Getting Outside – What the 2021 Axios Harris Poll 100 Brands Mean for Health/Care

We want to go outside, drive our cars, shop for groceries, stay and get healthy. These are the key themes coming out of the 2021 Axios Harris Poll 100 on the most visible brands with high (and low) reputations among U.S. consumers. In the top-ranked “excellent” and “very good” brands numbered 1 through 50, we find five core health care brands that were most visible to U.S. consumers: Moderna ranked #3, Pfizer #7, CVS Health #24, Walgreens #46, and Kaiser Permanente #47. The only pure healthcare brand in the bottom 50 was Johnson & Johnson at #72, between Dollar General
And the Oscar Goes To….Power to the Patients!
Health care has increased its role in popular culture over the years. In movies in particular, we’ve seen health care costs and hassles play featured in plotlines in As Good as it Gets [theme: health insurance coverage], M*A*S*H [war and its medical impacts are hell], and Philadelphia [HIV/AIDS in the era of The Band Played On], among dozens of others. And this year’s Oscar winner for leading actor, Anthony Hopkins, played The Father, who with his family is dealing with dementia. [The film, by the way, garnered six nominations and won two]. When I say “Oscar” here on the Health
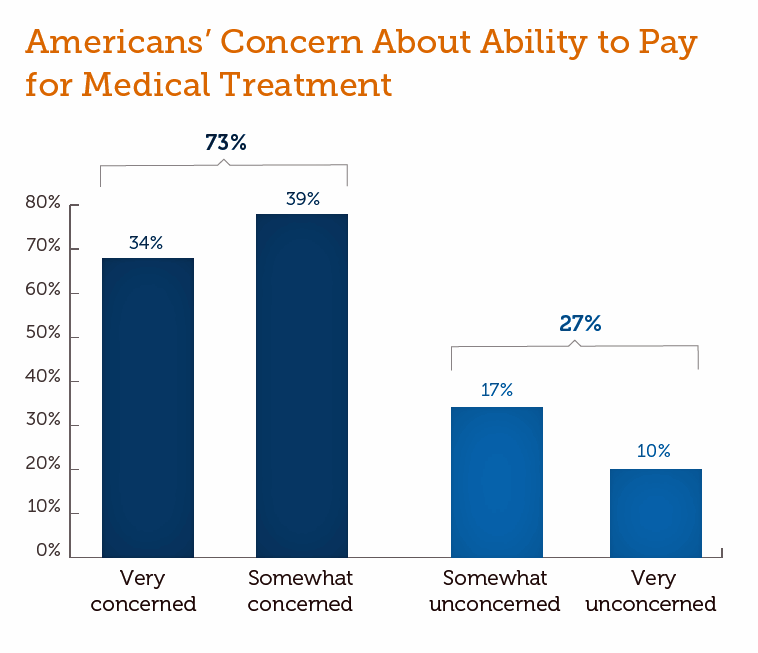
The Cost of Healthcare Can Drive Medical Rationing and Crowd Out Other Household Spending
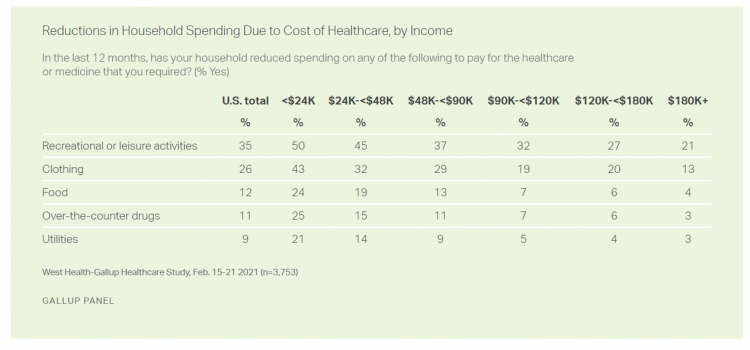
One in five people in the U.S. cannot afford to pay for quality health care — an especially acute challenge for Black and Hispanic Americans, according to a West Health-Gallup poll conducted in March 2021, a year into the COVID-19 pandemic. “The cost of healthcare and its potential ramifications continues to serve as a burdensome part of day-to-day life for millions of Americans,” the study summary observed. Furthermore, “These realities can spill over into other health issues, such as delays in diagnoses of new cancer and associated treatments that are due to forgoing needed care,” the researchers expected. The first table
The Continued Erosion of Trust in the Age of COVID
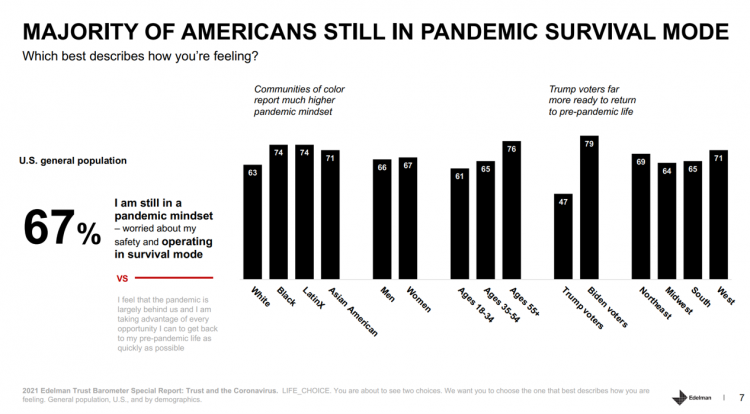
A year into the COVID-19 pandemic, most Americans are still in “survival mode,” according to an update of the 2021 Edelman Trust Barometer, Trust and the Coronavirus in the U.S. Updating the company’s annual Trust Barometer, Edelman conducted a new round of interviews in the U.S. among 2,500 people in early March. [For context, you can read my take on the 2021 Edelman Trust Barometer published during the World Economic Forum in January 2021 here in Health Populi]. The first chart shows that two in three people in the U.S. are still in a pandemic mindset, worried about safety and
The Ongoing Reality of COVID-19 – My Conversation with Dr. Michael Osterholm at SXSW
“So close and yet so far” feels like the right phrase to use a year after the World Health Organization used the “P-word,” “pandemic,” to describe the coronavirus’s impact on public health, globally. One year and over 550,000 COVID-related deaths in the U.S. later, we face a New Reality that Dr. Michael Osterholm and I are brainstorming today at the 2021 South-by-Southwest Festival. Usually held live and very up-close-and-personally crowded in Austin, Texas, this year we are all virtual — including the film, music, and interactive festivals alike. While I regret to not be in the same room as Dr.
How to Restore Americans’ Confidence in U.S. Health Care: Deal With Access and Cost
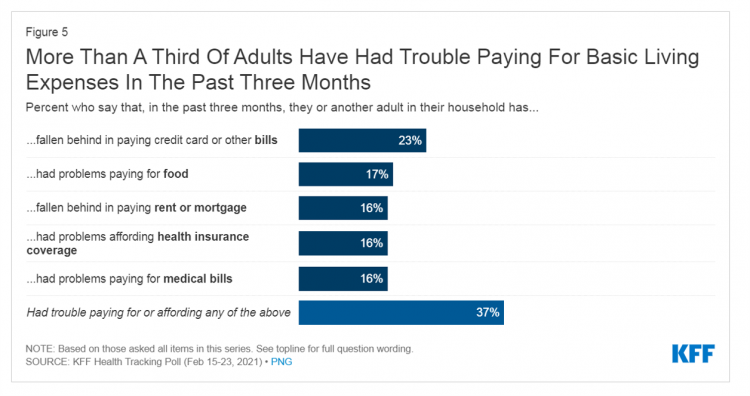
With a vaccine supply proliferating in the U.S. and more health citizens getting their first jabs, there’s growing optimism in America looking to the next-normal by, perhaps, July 4th holiday weekend as President Biden reads the pandemic tea leaves. But that won’t mean Americans will be ready to return to pre-pandemic health care visits to hospital and doctor’s offices. Now that hygiene protocols are well-established in health care providers’ settings, at least two other major consumer barriers to seeking care must be addressed: cost and access. The latest (March 2021) Kaiser Family Foundation Tracking Poll learned that at least one
“Hope Springs Eternal” With the COVID Vaccine for Both Joe Biden and Most People in the U.S.
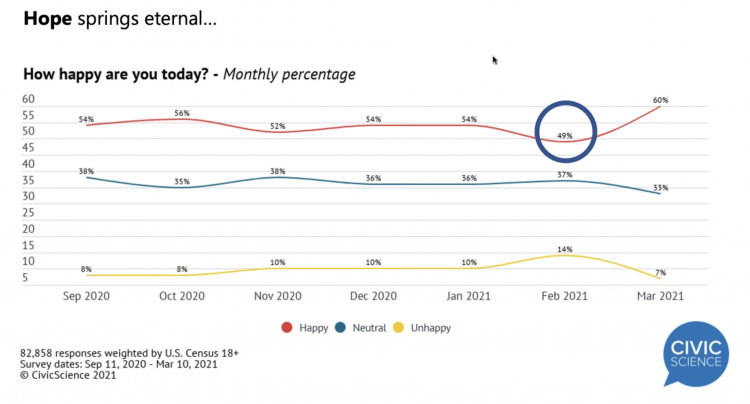
More Americans are happier in March 2021 than they’ve been for a year, based on consumer research from Civic Science polling U.S. adults in early March 2021. For the first time, a larger percent of Americans said they were better off financially since the start of the pandemic. This week, Civic Science shared their latest data on what they’re seeing beyond the coronavirus quarantine era to forecast trends that will shape a post-COVID America. Buoying peoples’ growing optimism was the expectation of the passage of the American Cares Act, which President Biden signed into effect yesterday. The HPA-CS Economic Sentiment Index
Value-Based Health Care Needs All Stakeholders at the Table – Especially the Patient

2021 is the 20th anniversary of the University of Michigan Center for Value-Based Insurance Design (V-BID). On March 10th, V-BID held its annual Summit, celebrating the Center’s 20 years of innovation and scholarship. The Center is led by Dr. Mark Fendrick, and has an active and innovative advisory board. [Note: I may be biased as a University of Michigan graduate of both the School of Public Health and Rackham School of Graduate Studies in Economics]. Some of the most important areas of the Center’s impact include initiatives addressing low-value care, waste in U.S. health care, patient assistance programs, Medicare
The Remarkable Rise of Pharma’s Reputation in the Pandemic
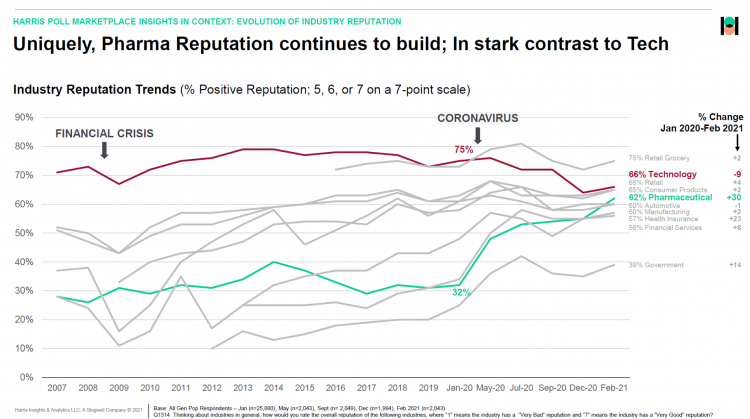
The reputation of the pharmaceutical industry gained a “whopping” 30 points between January 2020 and February 2021, based on the latest Harris Poll in their research into industries’ reputations. The study was written up by Beth Snyder Bulik in FiercePharma. Beth writes that, “a whopping two-thirds of Americans now offer a thumbs-up on pharma” as the title of her article, calling out the 30-point gain from 32% in January 2020 to 62% in February 2021. Thanks to Rob Jekielek, Managing Director of the Harris Poll, for sharing this graph with me for us to understand the details comparing pharma’s to
Americans Lost Future Life-Years in 2020: How Much Life Was Lost Depends on the Color of One’s Skin
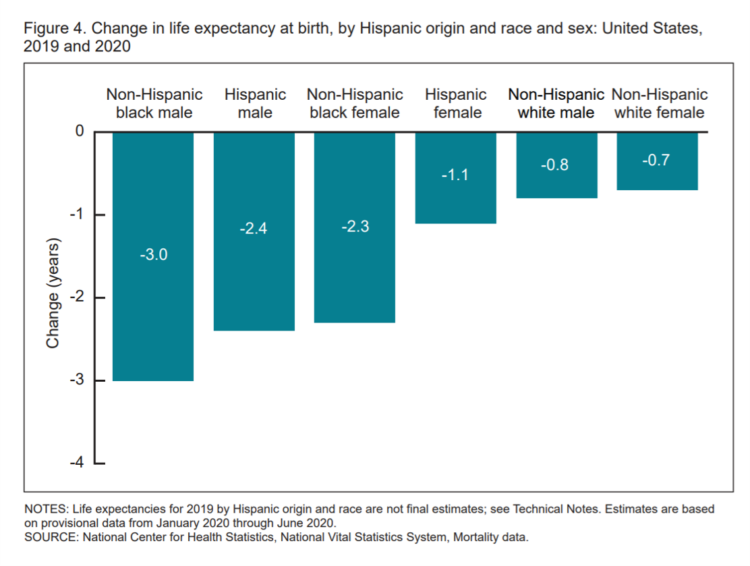
Some people remark about 2020 being a “lost year” in the wake of the coronavirus pandemic. That happens to be a true statement, sadly not in jest: in the U.S., life expectancy at birth fell by one full year over the first half of 2020 compared with 2019, to 77.8 years. In 2019, life expectancy at birth was 78.8 years, according to data shared by the National Center for Health Statistics (NCHS), part of the Centers for Disease Control and Prevention (CDC). Life expectancy at birth declined for both females and males, shown in the first chart. The differences between
Most Americans Want a Vaccine, Dissatisfied with the Rollout
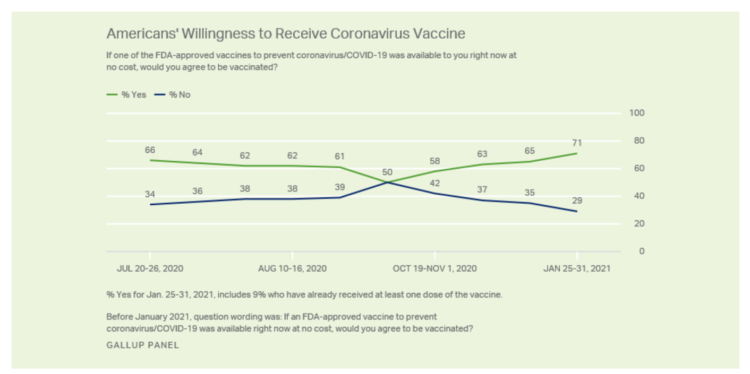
Seven in 10 U.S. adults are willing to be vaccinated, and they’re not happy about the process in getting their jab, according to Gallup’s poll taken in the last week of January 2021. The proportion of Americans willing to receive a COVID-19 vaccine has steadily grown since October 2020, which fell to a mere 50% of folks keen to get the shot. That percentage has risen to 71% as of February 1 2021, as the first line chart shows the reversal in public embrace for vaccination against the coronavirus. Now that most people in the U.S. welcome the opportunity to
Americans A Year Into the Pandemic – A View from Pew
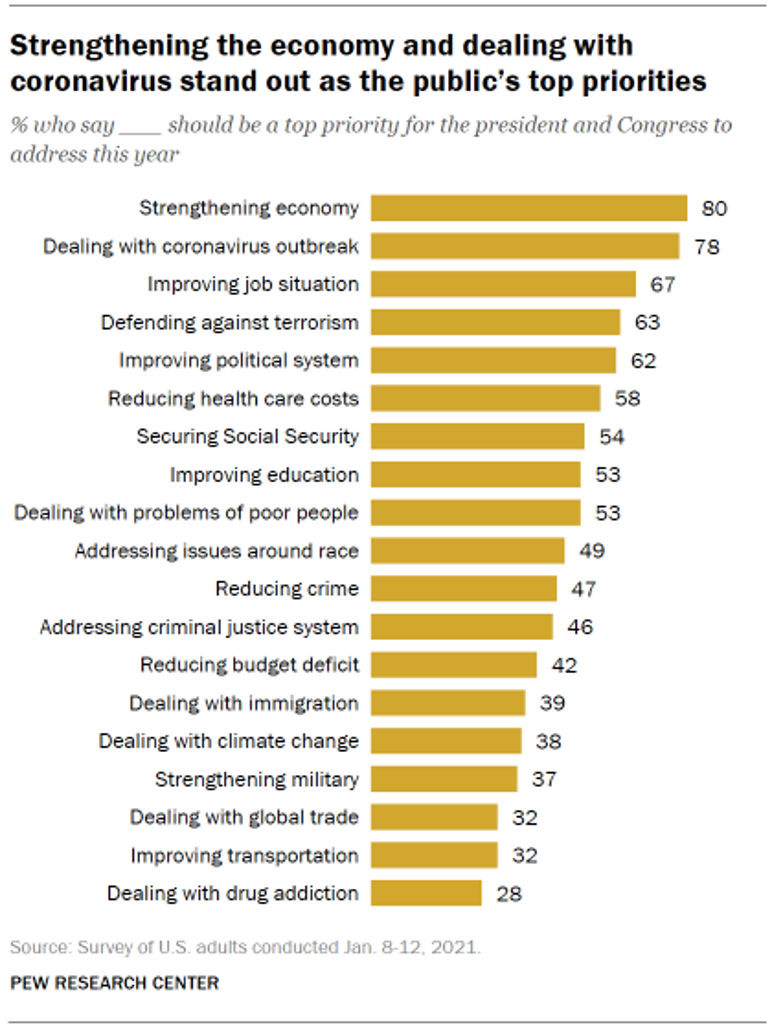
Nearly a year into the COVID-19 pandemic, the same percent of Americans say strengthening the U.S. economy and dealing with the coronavirus outbreak should be a top priority for President Biden and Congress to address this year, according to data from the Pew Research Center collected during the second week of January 2021. Two-thirds of people in the U.S. also want government leaders to prioritize improving the employment situation, defending against terrorism, and improving the political system, the study learned. At Americans’ low end of the priority list for the President and Congress are dealing with global trade, improving transportation,
Can Telemedicine Increase Health Equity? A Conversation with Antoinette Thomas, Dave Ryan, and Me with the ATA

“Yes,” we concurred on our session convened by the American Telemedicine Association (ATA) EDGE session today. “We” was a trio including Antoinette Thomas (@NurseTechExec1), Chief Patient Experience Officer with Microsoft, David Ryan (@DavidPRyan), former long-time Global Head of Intel’s Health/Life Science business; and, me. Antoinette posed three questions for all of us to brainstorm, addressing various aspects of health equity. We covered, The theory that telemedicine should increase health equity — where are we and what are the barriers to getting there? The role of social determinants of health in creating equitable opportunities for health citizens; and, Entering a post-pandemic world,
Dr. Burnout – The 2021 Medscape Physician Burnout & Suicide Report
Physicians in the U.S. are experiencing “death by 1,000 cuts,” according to the 2021 Medscape Physician Burnout & Suicide Report. Medscape polled 12,339 physicians representing over 29 specialties between late August and early November 2020 to gauge their feelings about work and life in the midst of the coronavirus pandemic. Medscape researched its first Physician Lifestyle Report in 2012. That research focused on physician “happiness” and work-life satisfaction. In 2013, the issue of burnout was called out on the cover of the report, shown here with the question, “does burnout affect lifestyle?” In 2015, the Physician Lifestyle Report was titled,
Addressing Lives and Livelihoods with a Whole-of-Government Approach – The First Wave of Biden Health Policy
President Biden’s first few days on the job gave us a very clear view on how he sees conquering COVID: through a whole-of-government approach to public policies that bolster directly addressing the virus, along with the many forces shaping how we got here and how to come out of the pandemic era stronger. I cover this first wave of Biden health policy in my latest post for the Medecision Liberation blog titled, “Top Priorities for President Biden: COVID-19, Then Everything Else.” The plotline goes… On the day of inauguration, January 20, 2021, Joseph R. Biden was installed as the 46th
The Biden Administration’s Whole-of-Government Approach to Equity – in Health and Beyond
In the U.S., the COVID-19 pandemic has revealed disparities in housing, food, and job security, and the role that one’s ZIP code and social determinants play in health outcomes. Overall, America has done poorly in light of being 4% of the world’s population but having one-fifth of the planet’s deaths due to the coronavirus. But these have disproportionately hit non-white people, who are nearly three times as likely to die from COVID-19 than white Americans. I’ve been head-down reviewing the first two days of President Biden’s signing Executive Orders, reading the National Strategy for COVID-19 Response, and inventorying line items
Our Homes Are Health Delivery Platforms – The New Home Health/Care at CES 2021

The coronavirus pandemic disrupted and re-shaped the annual CES across so many respects — the meeting of thousands making up the global consumer tech community “met” virtually, both keynote and education sessions were pre-recorded, and the lovely serendipity of learning and meeting new concepts and contacts wasn’t so straightforward. But for those of us working with and innovating solutions for health and health care, #CES2021 was baked with health goodness, in and beyond “digital health” categories. In my consumer-facing health care work, I’ve adopted the mantra that our homes are our health hubs. Reflecting on my many conversations during CES
Trust Plummets Around the World: The 2021 Edelman Trust Barometer in #CES2021 and Microsoft Context
Citizens around the world unite around the concept that Trust is Dead. This is no truer than in the U.S., where trust in every type of organization and expert has plummeted in the wake of the COVID-19 pandemic, political and social strife, and an economic downturn. Welcome to the sobering 2021 Edelman Trust Barometer, released this week as the world’s technology innovators and analysts are convening at CES 2021, and the annual JP Morgan Healthcare meetup virtually convened. As the World Economic Forum succinctly put the situation, “2020 was the year of two equally destructive viruses: the pandemic and the
The 2021 Shkreli Awards: Lown Institute Counts Down the Top 10 Healthcare Industry Abuses in the Coronavirus Pandemic

The first year of the coronavirus pandemic in America was a kind of stress test on the U.S. health care system, revealing weak links and opportunities for bad behavior. “These are not just about individual instances or bad apples,” Dr. Vikas Saini, President of The Lown Institute, explained, referring to them as “cautionary tales” of the current state of U.S. health care. Dr. Saini and his colleague Shannon Brownlee released the annual Lown Institute 2020 Shkreli Awards this week, highlighting their ten most egregious examples of the worst events in U.S. health care that happened in the past year —
Vaccine Enthusiasm, from Warp-Speed to Right-Speed
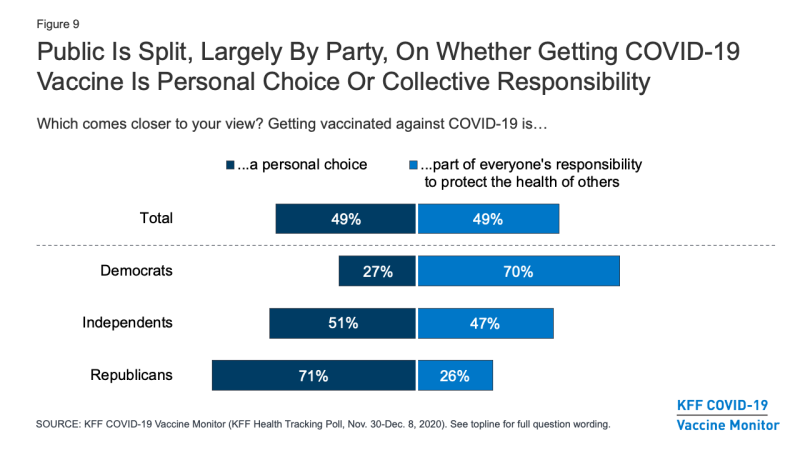
Since the spike in hospitalizations and deaths topping 300,000 in the U.S., one day and week at a time, it appears that more Americans are moving on a continuum from being vaccine-hesitant toward vaccine-enthusiasm. The latest Kaiser Family Foundation COVID-19 Vaccine Monitor for December 2020 quantifies this moving sentiment across several perspectives: Most Americans across political party believe the COVID-19 vaccine development process is moving at the right speed The number of Americans who would get a coronavirus vaccine if it were free and seen as safe grew since September, from 34% of people who would “definitely get it” to
Vaccine Hesitancy Is Greatest Among Those at Highest Risk of Dying from COVID-19: Black People
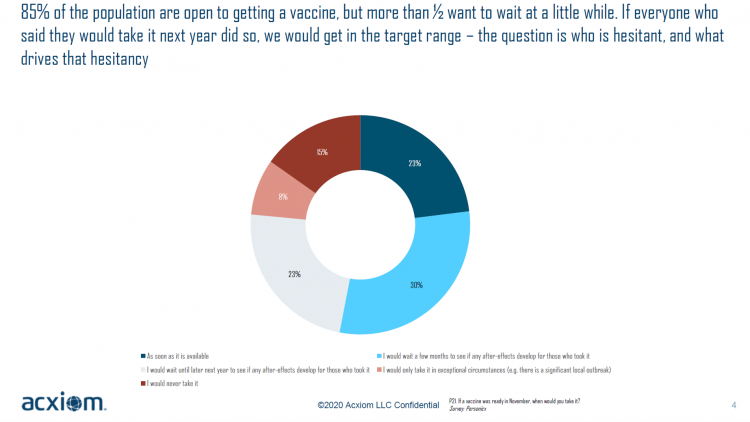
While 85% of people are open to receiving a COVID-19 vaccine, over one-half of them would want to wait some time to observe if after-effects developed in people who took the jab, according to a new study from Acxiom, the data analytics-marketing company. Not all people are as enthused about getting a coronavirus vaccine at all, Acxiom discovered: in fact, those hardest hit by the virus — Black people — would be the least-likely to want to get a COVID-19 vaccine, discussed in in Vaccine Hesitancy in the U.S., a survey the company conducted among 10,000 people in the U.S.
The COVID Healthcare Consumer – 5 Trends Via The Medecision Liberation Blog
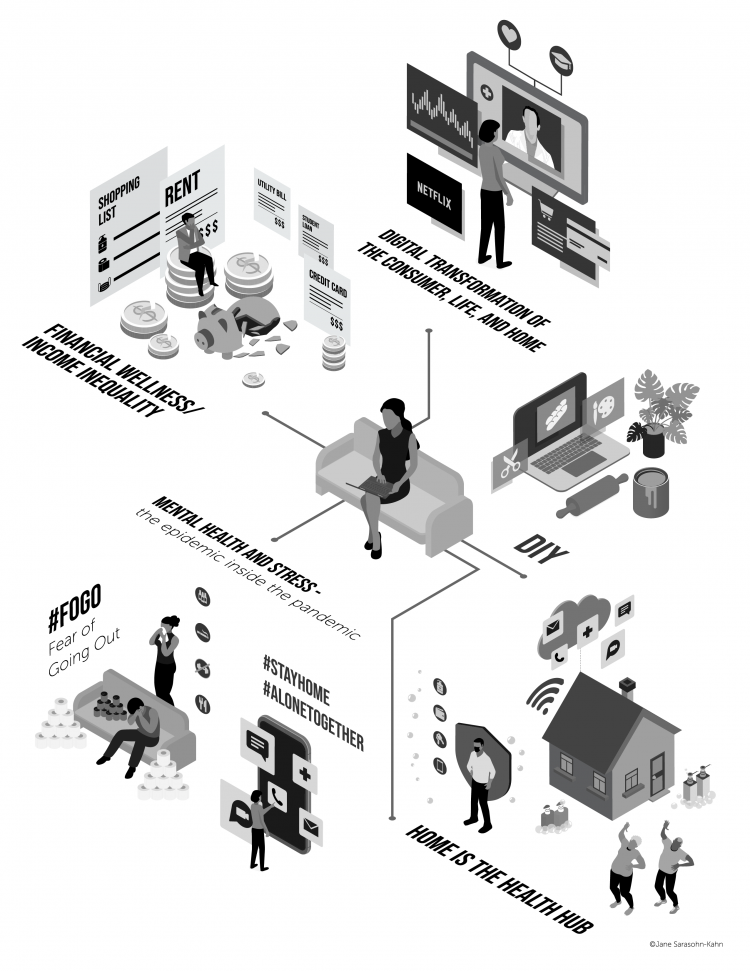
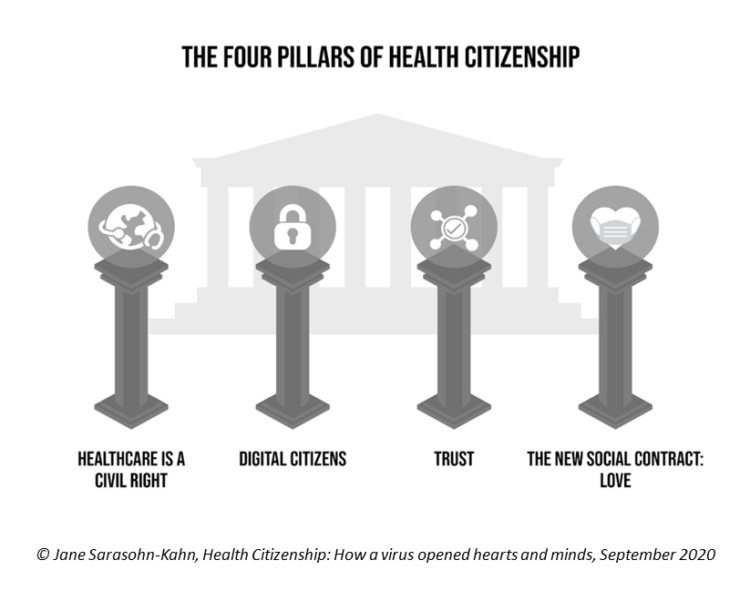
The first six months into the coronavirus pandemic shocked the collective system of U.S. consumers for living, learning, laboring, and loving. I absorbed all kinds of data about consumers in the wake of COVID-19 between March and mid-August 2020, culminating in my book, Health Citizenship: How a virus opened hearts and minds, published in September on Kindle and in print in October. In this little primer, I covered the five trends I woven based on all that data-immersion, following up the question I asked at the end of my previous book, HealthConsuming: when and how would Americans claim their health
Will We See A Field of Dreams for the COVID-19 Vaccine in the U.S.?
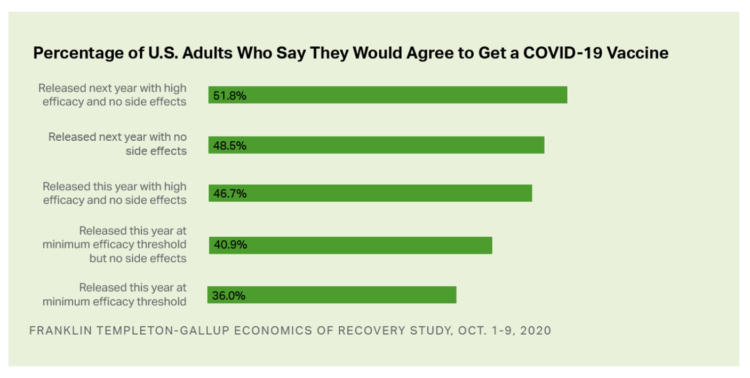
“If you build it, he will come,” the voice of James Earl Jones echoes in our minds when we recall the plotline of the film, Field of Dreams. A quick summary if you don’t know the movie: the “it” was a baseball field to be built in a rural cornfield. The “he” was a baseball player, ultimately joined by a dream-team of ball players who would convene on that dreamy field to play an amazing game. Today, the day after Pfizer announced a 90% benefit for its coronavirus vaccine, bolstering Wall Street returns on 9th November 2020, two new consumer
Keep Calm and Carry On With Counting the Votes: How CNN Allied With A Tele-Mental Health App

Yesterday, the 4th of November 2020, the cable network CNN published a story titled, “Survive election uncertainty with these expert tips on how to cope.” That morning-after-the-Election-night-before followed CNN’s allying on #2020Elections night with the Calm app — a marketing alliance meant to address the real phenomenon of political stress that has been ramping up in the U.S. for several years. I liked Teen Vogue‘s coverage of the story best, and linked it here, but you can also view lenses on the event in: Adweek, Meditation App Calm Was the Most 2020 Brand Partner for CNN’s Election Coverage, whose key
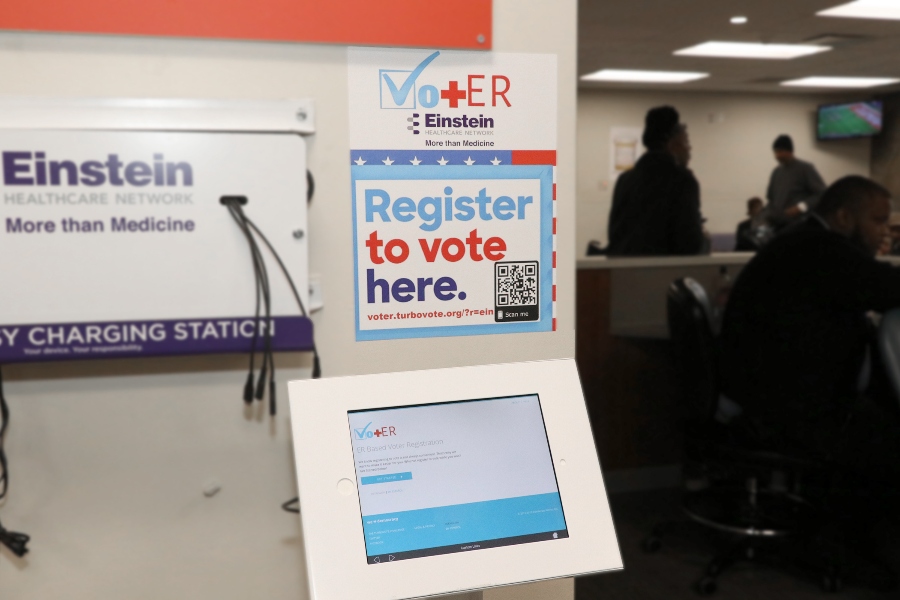
Voting for Health in 2020

In the 2018 mid-term elections, U.S. voters were driven to polls with health care on their minds. The key issues for health care voters were costs (for care and prescription drugs) and access (read: protecting pre-existing conditions and expanding Medicaid). Issue #2 for 2018 voters was the economy. In 2020, as voting commences in-person tomorrow on 3rd November, U.S. voters have lives and livelihoods on their minds. It’s the pandemic – our physical lives looming largest in the polls – coupled with our fiscal and financial lives. Health is translating across all definitions for U.S. voters in November 2020: for
Masks Work. A Picture From Kansas That Tells A Story in Two Words.
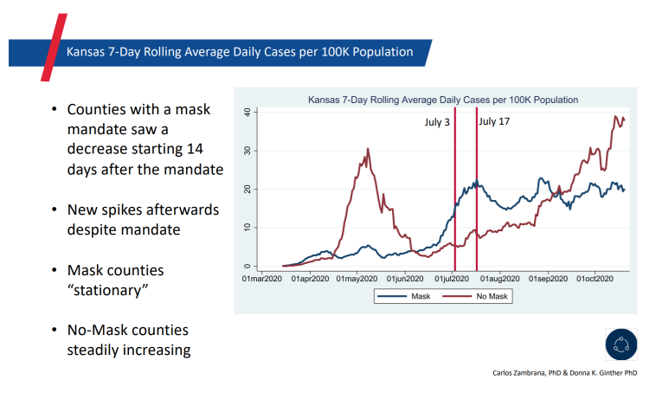
It is said that a picture tells a thousand words. This picture tells an even quicker story that can save lives: “Masks work.” The backstory: Kansas Governor Laura Kelly issued a mask mandate on July 2, 2020. The rationale: That was two days before Independence Day, the holiday weekend when she and state public health officials anticipated health citizens would abandon their personal efforts to physically distance and cover faces to avoid contracting or spreading the coronavirus. This was the message directly communicated to U.S. residents by the White House Coronavirus Task Force that week before Independence Day. The backlash:
Health Care Providers Are More Politically Engaged in the 2020 Elections
Until 2016, physicians’ voting rates in U.S. elections had not changed since the late 1970s. Then in 2018, two years into President Donald Trump’s four-year term, the mid-term elections drove U.S. voters to the election polls…including health care providers. Based on the volume and intensity of medical professional societies’ editorials on the 2020 Presidential Election, we may be in an inflection-curve moment for greater clinician engagement in politics as doctors and nurses take claim of their health citizenship. A good current example of this is an essay published in the AMA’s website asserting, “Why it’s okay for doctors to ask
Stress in America, Like COVID-19, Impacts All Americans
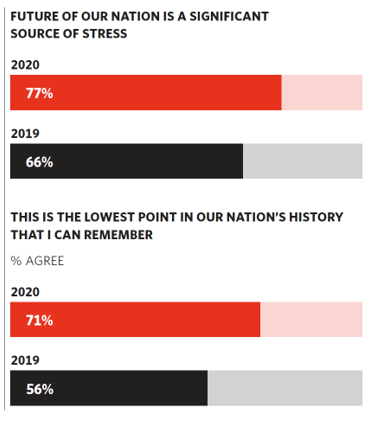
With thirteen days to go until the U.S. #2020Elections day, 3rd November, three in four Americans say the future of America is a significant source of stress, according to the latest Stress in America 2020 study from the American Psychological Association. Furthermore, seven in 10 U.S. adults believe that “now” is the lowest point in the nation’s history that they can remember. “We are facing a national mental health crisis that could yield serious health and social consequences for years to come,” APA introduces their latest read into stressed-out America. Two in three people in the U.S. say that the
Two in Three Americans Cite the U.S. Presidential Election is a Significant Source of Stress, Even More than the 2016 Race
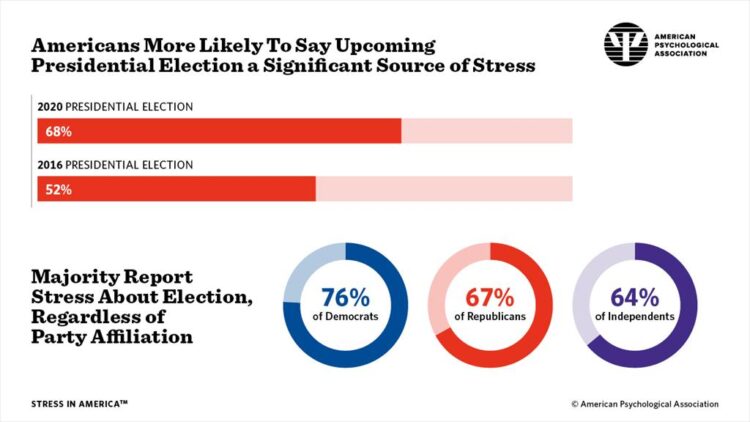
If you perceive you are more stressed in the COVID-19 pandemic than you were in 2019, you are one in many millions feeling so. If you felt stressed during the 2016 Presidential election season, you were also one in a million. Now, as the 2020 Election converges with the coronavirus crisis, even more Americans are feeling significant stress in a double-whammy impact. Our friends at the American Psychological Association have assessed Stress in America for many years of studies. The latest, published 7 October, finds that the 2020 Presidential election is a source of significant stress for more Americans than
The Coronavirus Pandemic Turbocharged Digital Health Investment in 2020
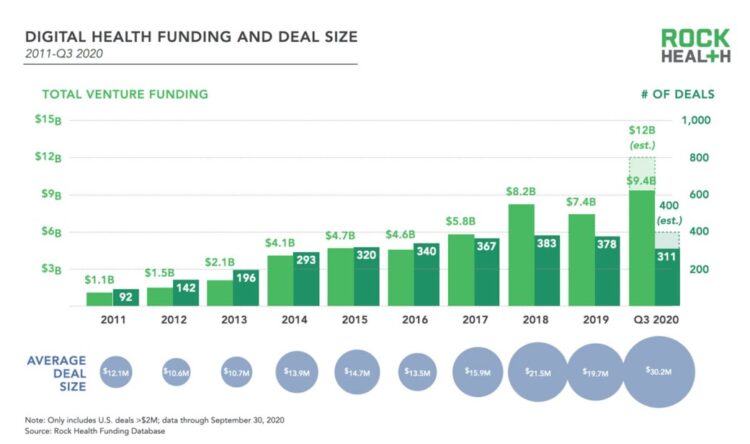
2020 will be remembered for disruption and dislocation on many fronts; among the major blips in the year will be it remembered as the largest funding year for digital health recorded, according to Rock Health’s report on the 3Q2020 digital health funding. This funding record (“already” before year-end, tallied by the third quarter as Rock Health notes) was driven by “mega”-deals accelerated during the public health crisis of COVID-19. In the third quarter of 2020, some $4 billion was invested in U.S. based digital health start-ups adding up $9.4 billion in 2020….so far. This is $1.2 billion more than two
Financial Health Is On Americans’ Minds Just Weeks Before the 2020 Elections
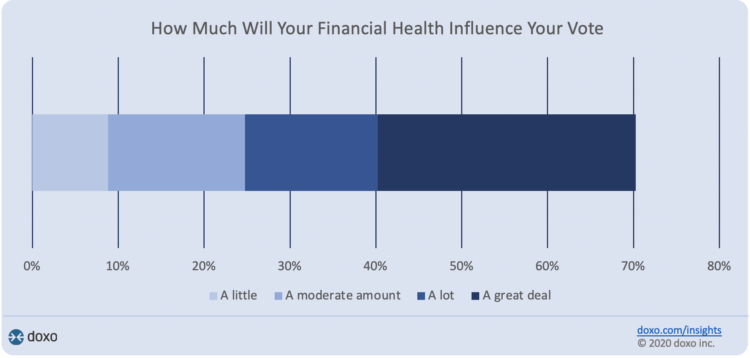
Financial health is part of peoples’ overall health. As Americans approach November 3, 2020, the day of the real-time U.S. Presidential and down-ballot elections, personal home economics are front-of-mind. Twenty-seven days before the 2020 elections, 7 in 10 Americans say their financial health will influence their votes this year, according to the doxoINSIGHTS survey which shows personal financial health as a key voter consideration in the Presidential election. Doxo, a consumer payments company, conducted a survey among 1,568 U.S. bill-paying households in late September 2020. The study has a 2% margin of error. U.S. voters facing this year’s election are
The Emergence of Health Citizens – Part of Liberating Health, on the Medecision Blog
I have always appreciated Medecision’s mission as expressed in the company’s tagline: “Liberating,” as in “liberate healthcare.” I began collaborating with Medecision as a client several years ago, a couple of years after I heard Todd Park, then Chief Technology Officer in the White House, joyfully assert the phrase, “Data Liberación!” at an early Health 2.0 Conference. Medecision published my blog about health citizenship this week on the company’s Liberate.Health site. The emergence of health citizens in the U.S. — people re-claiming their health, health care, and control of data — is part of liberating health in America. Please check
Health Citizenship in America. If Not Now, When?
On February 4th, 2020, in a hospital in northern California, the first known inpatient diagnosed with COVID-19 died. On March 11th, the World Health Organization called the growing prevalence of the coronavirus a “pandemic.” On May 25th, George Floyd, a 46-year-old Black man, died at the hands of police in Minneapolis. This summer, the Dixie Chicks dropped the “Dixie” from their name, and NASCAR cancelled the confederate flag from their tracks. Today, nearly 200,000 Americans have died due to the novel coronavirus. My new book, Health Citizenship: How a virus opened hearts and minds, launched this week. In it, I
Only in America: The Loss of Health Insurance as a Toxic Financial Side Effect of the COVID-19 Pandemic

In terms of income, U.S. households entered 2020 in the best financial shape they’d been in years, based on new Census data released earlier this week. However, the U.S. Census Bureau found that the level of health insurance enrollment fell by 1 million people in 2019, with about 30 million Americans not covered by health insurance. In fact, the number of uninsured Americans rose by 2 million people in 2018, and by 1.9 million people in 2017. The coronavirus pandemic has only exacerbated the erosion of the health insured population. What havoc a pandemic can do to minds, bodies, souls, and wallets. By September 2020,
50 Days Before the U.S. Elections, Voters Say Health Care Costs and Access Top Their Health Concerns — More than COVID-19
The coronavirus pandemic has revealed deep cracks and inequities in U.S. health care in terms of exposure to COVID-19 and subsequent outcomes, with access to medical care and mortality rates negatively impacting people of color to a greater extent than White Americans. The pandemic has also led to economic decline that, seven weeks before the 2020 elections in America, is top-of-mind for health citizens with the virus-crisis itself receding to second place, according to the Kaiser Family Foundation September 2020 Health Tracking Poll. KFF polled 1,199 U.S. adults 18 years of age and older between August 28 and September 3,
Americans Worry About Medical Bankruptcy, As Prescription Drug Costs Play Into Voters’ Concerns
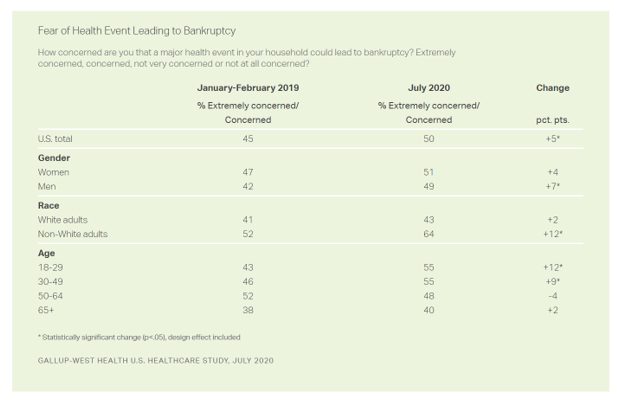
One in two people in the U.S. are concerned that a major health event in their family would lead to bankruptcy, up 5 percent points over the past eighteen months. In a poll conducted with West Health, Gallup found that more younger people are concerned about medical debt risks, along with more non-white adults, published in their study report, 50% in U.S. Fear Bankruptcy Due to Major Health Event. The survey was fielded in July 2020 among 1,007 U.S. adults 18 and older. One of the basic questions in studies like these is whether a consumer could cover a $500
Behavioral Health Side-Effects in the COVID Era
“This surge of people experiencing acute behavioral health problems…has the potential to further impact the healthcare system for years to come,” a report from McKinsey expects looking at the hidden costs of COVID-19’s impact on U.S. health care. The coronavirus pandemic has taken a toll on Americans’ mental health, with anxiety and depression growing as a side-effect to worries about the virus itself, the long Great Lockdown in much of the country, and the economic recession that has particularly impacted women and people of color. I covered depression impacts due to COVID-19 here in Health Populi yesterday, and wanted to
The Next-Normal Health Care Consumer After the Pandemic
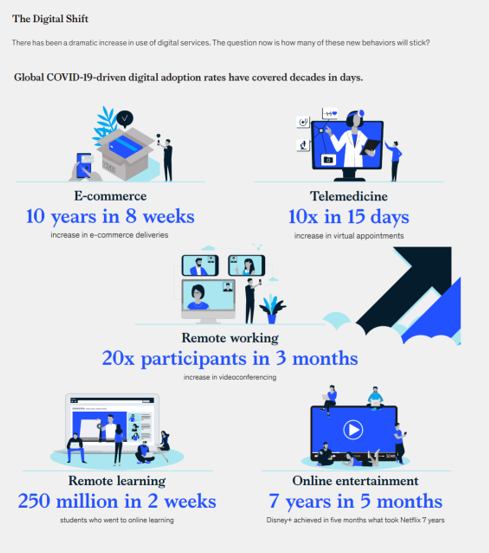
McKinsey invites us to Meet the next-normal consumer in a recently-published research report describing changing consumer behavior responding to the COVID-19 lockdown and aftermath. The report gives us insights into the next-normal health consumer, which I’ll discuss in today’s post. Note the massive digital shift every person living in a country touched by the coronavirus has experienced, illustrated in the first graphic from the report. Tele-work, tele-education, ecommerce, and streaming entertainment all grew so fast within a matter of a few weeks. And telemedicine, McKinsey points out, was adopted at a rate of ten times growth over 15 days, the
How COVID-19 Is Reshaping Cities and Inspiring Healthcare Innovation
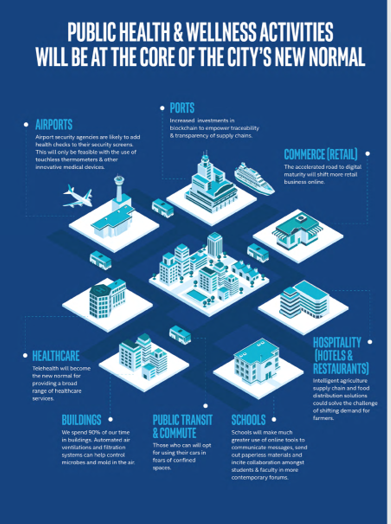
The coronavirus pandemic added a new concept to our collective, popular lexicon: “social distancing” and “physical distancing.” This was one pillar for the public health prescription we were given to help mitigate the spread of a very tricky, contagious virus. A major negative impact of our sheltering in place, working from home, and staying indoors has been a sort of clearing out of cities where people congregate for work, for culture, for entertainment, for education, for travel and tourism…for living out our full and interesting lives and livelihoods. Intel gave Harbor Research a mandate to “re-imagine life in a post-pandemic
Data Well-Being: A Pillar of Health Citizenship for US Consumers
In the COVID-19 era, most U.S. consumers believe they have an obligation to share personal health information to stop the spread of the coronavirus. However, only 44% would be willing to share their personal data with a national database, a MITRE study learned. Only one-third of Americans would be willing to share their temperature, 29% their location, and one-fourth information about their chronic conditions. The Harris Poll conducted the study among 2,065 U.S. adults 18 and over in mid-June 2020 to gauge peoples’ perspectives on health data and privacy. Three-quarters of people in the U.S. believe that data privacy “is a
My ABCovid-19 Journal – Day 4 of 5, Letters “P” through “T”
While I’m on holiday this week, restoring and re-setting, I’ve been sharing pages from my ABCovid-19 Journal with readers of Health Populi. I created this journal during the early phase of the pandemic in the U.S., as a form of art therapy, creative outlet, and learning. Today is Day 4 of sharing: we consider the letters “P” through “T,” and what I saw in the early coronavirus era. P is for pandemic This “P” was self-evidence in our collective early COVID-19 lexicon. The “P” word was uttered by the Secretary General of the World Health Organization on March 11, confirming
My ABCovid-19 Journal – Day 3 of 5, Letters “K” through “O”
Welcome back to my ABCovid-19 Journal, which I created/curated in the early weeks of the coronavirus pandemic. This week, I’m sharing all the letters of the alphabet with you which reminded me keywords and themes emerging as we were learning about this dastardly public health threat beginning early in 2020. In today’s Health Populi blog I bring you letters “K” through “O,” continuing through the rest of the alphabet tomorrow and Friday while I’m on a lake-side holiday that’s good for mind, body, and spirit. K is for Kirkland, Washington state In the U.S., one of the earliest hotspots for
My ABCovid-19 Journal, Day 2 of 5 – Letters “F” through “J”
Welcome to Day 2 of my #COVID19 holiday break, welcome to my ABCovid Journal, letters “F” through “J. If you hadn’t tuned into the Health Populi blog yesterday, 10th August 2020, you missed the first five letters of my Age of Corona alphabet, curated in my art journal created in the early weeks of the pandemic. Click the link to back-track and catch up with us… I should explain why I’m sharing this project in the Health Populi blog this week. Last month, long-time colleague and friend Colin Hung interviewed me on the #HITMC broadcast to discuss a lovely recognition
My ABCovid-19 Journal – Day 1 of 5, “A” through “E”
My friends… It’s time in this pandemic journey that I take a full week to re-charge and bask in the midst of nature, a lake, farm-to-table food, wine-making, and the love of and therapeutic time with my wonderful husband. My gift to you all this week, 10th – 14th August, is to share with you pages from my “ABCovid-19 Journal” that I created/curated in the first weeks of the coronavirus pandemic. We all have our hacks for managing stress and discomfort, and in the first weeks of COVID-19, this was my life-saver. Journaling is one of my self-care strategies; think
Return-To-School Is Stressing Out U.S. Parents Across Income, Race and Political Party
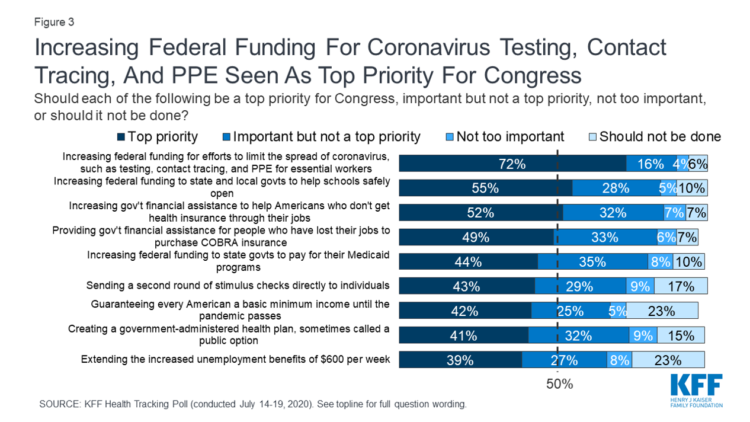
The worse of the coronavirus pandemic is yet to come, most Americans felt in July 2020. That foreboding feeling is shaping U.S. parents’ concerns about their children returning to school, with the calendar just weeks away from educators opening their classrooms to students, from kindergarten to the oldest cohort entering senior year of high school. The Kaiser Family Foundation’s July 2020 Health Tracking Poll focuses on the COVID-19 pandemic, return-to-school, and the governments’ response. KFF polled 1,313 U.S. adults 18 and older between July 14 to 19, 2020. The first line chart illustrates Americans’ growing concerns about the coronavirus, shifting
More Americans Pivot to Distancing and Mask-Wearing in the Hot Summer of 2020
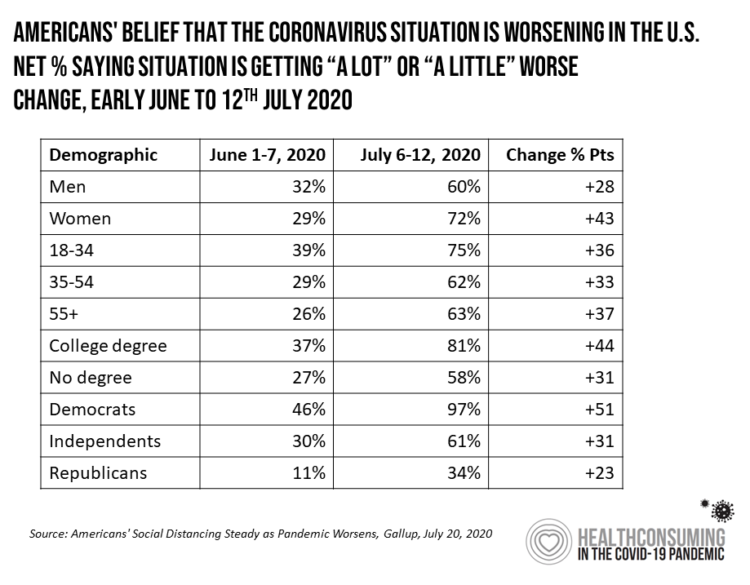
With growing coronavirus case hotspots in southern and western states, more Americans perceive the pandemic is worsening this summer, shown by a Gallup poll published 20 July 2020. Gallup titles the analysis, Americans’ social distancing steady as pandemic worsens. The first table organizes Gallup’s data by demographics, illustrating a significant gap between how women perceive the exacerbating pandemic compared with men. In early June, roughly one-third of both men and women saw COVID-19 was getting “worse”; five weeks later, in the second week of July, men and women’s perceptions were 12 points apart with more women concerned about the situation
Stressed Out By COVID and Civil Unrest – the APA’s Stress in America Survey, Part 2
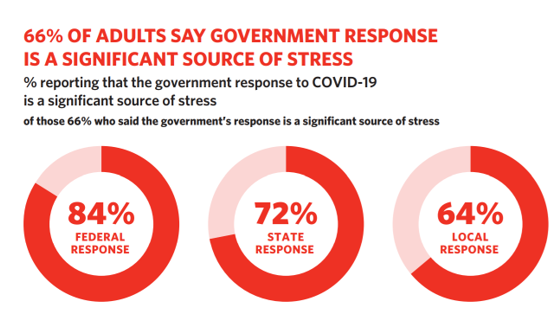
“Now” is the lowest point in history that most Americans can remember: 7 in 10 people in the U.S. feel this way, up from 56% in 2018 and 2019. Furthermore, 4 in 5 people in the U.S. say the future of America is a significant source of stress, as discussed in Stress in the Time of COVID-19, Volume Two, a report covering a poll of U.S. adults sponsored by the American Psychological Association. APA’s Stress in America research has been one of my annual go-to’s for better understanding U.S. residents through the lens of health consumers and, especially this year
Health Insurance and Demand for Masking, Testing and Contact Tracing – New Data from The Commonwealth Fund
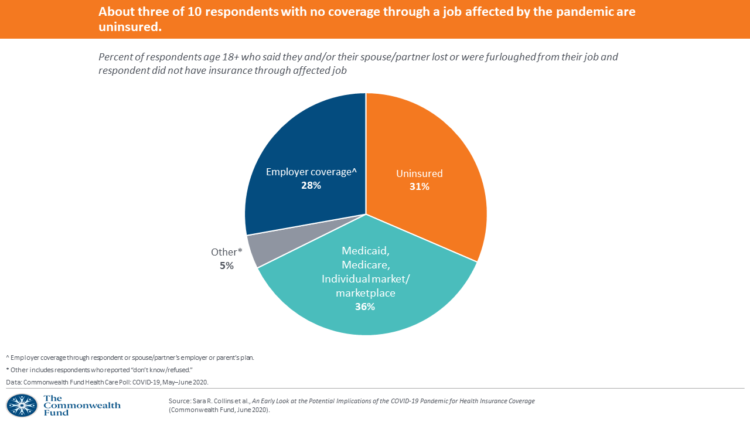
The coronavirus pandemic occasioned the Great Lockdown for people to shelter-at-home, tele-work if possible, and shut down large parts of the U.S. economy considered “non-essential.” As health insurance for working-age people is tied to employment, COVID-19 led to disproportionate loss of health plan coverage especially among people earning lower incomes, as well as non-white workers, explained in the Commonwealth Fund Health Care Poll: COVID-19, May-June 2020. The Commonwealth Fund commissioned interviews with 2,271 U.S. adults 18 and over between 13 May and 2nd June 2020 for this study. The survey has two lenses: first, on health insurance coverage among working
Juneteenth 2020: Inequality and Injustice in Health Care in America
“Of all the forms of inequality, injustice in health is the most shocking and the most inhuman because it often results in physical death,” Martin Luther King, Jr., asserted at the second meeting of the Medical Committee for Human Rights in Chicago on March 25, 1966. This quote has been shortened over the five+ decades since Dr. King told this truth, to the short-hand, “Of all the forms of inequality, injustice in health care is the most shocking and inhumane.” Professor Charlene Galarneau recently enlightened me on Dr. King’s original statement in her seminal essay, “Getting King’s Words Right.” Among
Americans Across Political Party Worry About Prescription Drug Prices – Especially to Deal with COVID-19
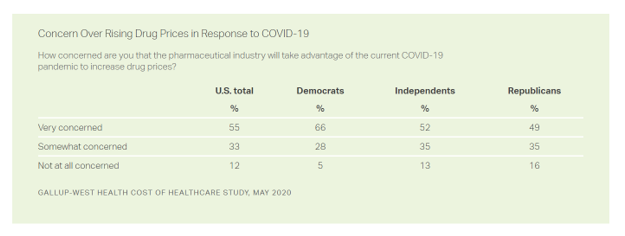
Nine in ten Americans is concerned about the price of prescription drugs in the wake of the coronavirus pandemic, Gallup and West Health found in their survey on the cost of healthcare, published today. A majority of people across political party share this concern: overall, 88% of U.S. adults are concerned about rising drug prices in response to COVID19, split across party ID with: 94% of Democrats, 86% of Independents, and 84% of Republicans. By demographics, more women than men are concerned about rising costs for the three health care spending categories the survey studied: drug prices, insurance premiums, and
Economic Anxieties Rise, Medical and Vacation Plans Delayed: the COVID-19 Consumer in June 2020
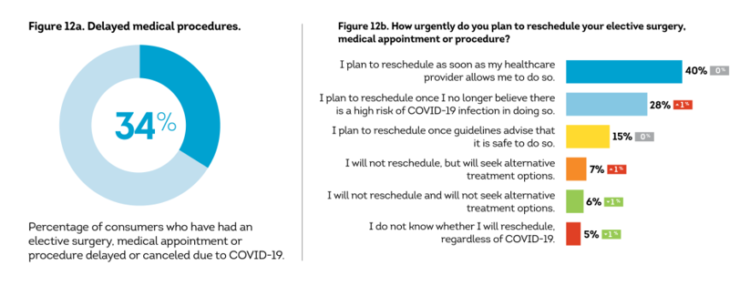
Some 6 in 10 people in the U.S. have been financially impacted by COVID-19. Those most negatively affected by the pandemic tend to be younger, Gen Z age group and African-American, 63% of whom felt financial pressure directly due from the virus and the national economic lockdown. By late May 2020, 34% of black Americans had lost their jobs compared with 21% in late April, compared with 18% of white consumers, reported in The COVID-19 Pandemic’s Financial Impact on U.S. Consumers, survey research from TransUnion. This post describes data from TransUnion’s Wave 9 report, which polled 2,086 U.S. adults 18
Americans’ Concerns About the US Healthcare System Loom Larger Than Worries About Their Own Care
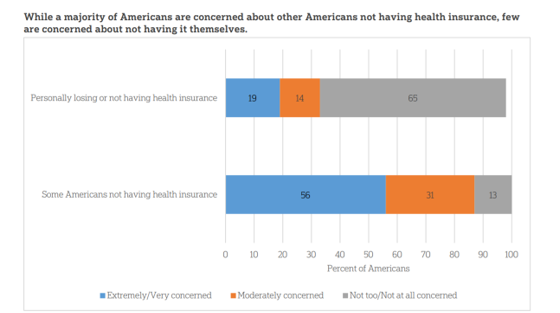
The coronavirus pandemic has further opened the kimono of the U.S. healthcare system to Americans: four months into the COVID-19 outbreak, most consumers (62%) of people in the U.S. are more concerned about other people not having access to high quality health care versus themselves. This is a 16 point increase in concern in May 2020 compared with the response to the same question asked in February in a poll conducted by the University of Chicago Harris School of Public Policy and The Associated Press-NORC Center for Public Affairs Research (the AP-NORC Center). The AP-NORC Poll found more of this
Stress in America – COVID-19 Takes Toll on Finances, Education, Basic Needs and Parenting

“The COVID-19 pandemic has altered every aspect of American life, from health and work to education and exercise,” the new Stress in America 2020 study from the American Psychological Association begins. The APA summarizes the impact of these mass changes on the nation: “The negative mental health effects of the coronavirus may be as serious as the physical health implications,” with COVID-19 stressors hitting all health citizens in the U.S. in different ways. Beyond the risk of contracting the virus, the Great Lockdown of the U.S. economy has stressed the U.S. worker and the national economy, with 7 in 10
Health, Wealth & COVID-19 – My Conversation with Jeanne Pinder & Carium, in Charts
The coronavirus pandemic is dramatically impacting and re-shaping our health and wealth, simultaneously. Today, I’ll be brainstorming this convergence in a “collaborative health conversation” hosted by Carium’s Health IRL series. Here’s a link to the event. Jeanne founded ClearHealthCosts nearly ten years ago, having worked as a journalist with the New York Times and other media. She began to build a network of other journalists, each a node in a network to crowdsource readers’-patients’ medical bills in local markets. Jeanne started in the NYC metro and expanded, one node at a time and through many sources of funding from not-for-profits/foundations,
Americans’ Sense of Well-Being Falls to Great Recession Levels, Gallup Finds
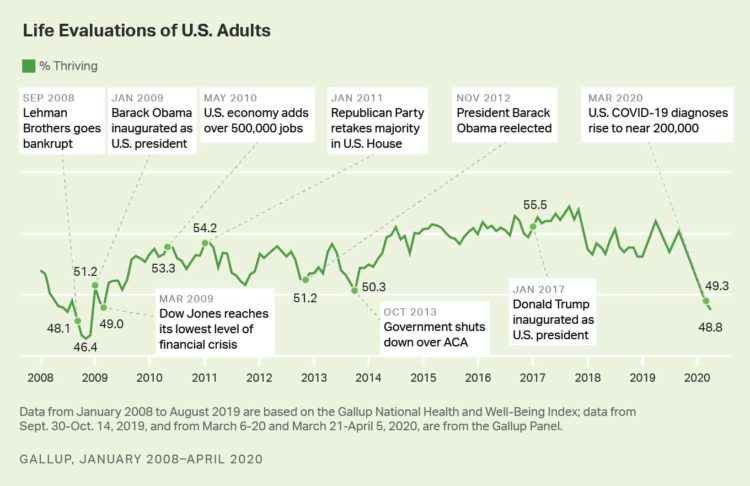
It’s déjà vu all over again for Americans’ well-being: we haven’t felt this low since the advent of the Great Recession that hit our well-well-being hard in December 2008. As COVID-19 diagnoses reached 200,000 in the U.S. in April 2020, Gallup gauged that barely 1 in 2 people felt they were thriving. In the past 12 years, the percent of Americans feeling they were thriving hit a peak in 2018, as the life evaluations line graph illustrates. Gallup polled over 20,000 U.S. adults in late March into early April 2020 to explore Americans’ self-evaluations of their well-being. FYI, Gallup asks consumers
The Coronavirus Impact on American Life, Part 2 – Our Mental Health
As the coronavirus pandemic’s curve of infected Americans ratchets up in the U.S., people are seeking comfort from listening to Dolly Parton’s bedtime stories, crushing on Dr. Anthony Fauci’s science-wrapped-with-empathy, and streaming the Tiger King on Netflix. These and other self-care tactics are taking hold in the U.S. as most people are “social distancing” or sheltering in place, based on numbers from the early April 2020 Kaiser Family Foundation health tracking poll on the impact of the coronavirus on American life. While the collective practice of #StayHome to #FlattenTheCurve is the best-practice advice from the science leaders at CDC, the NIAID
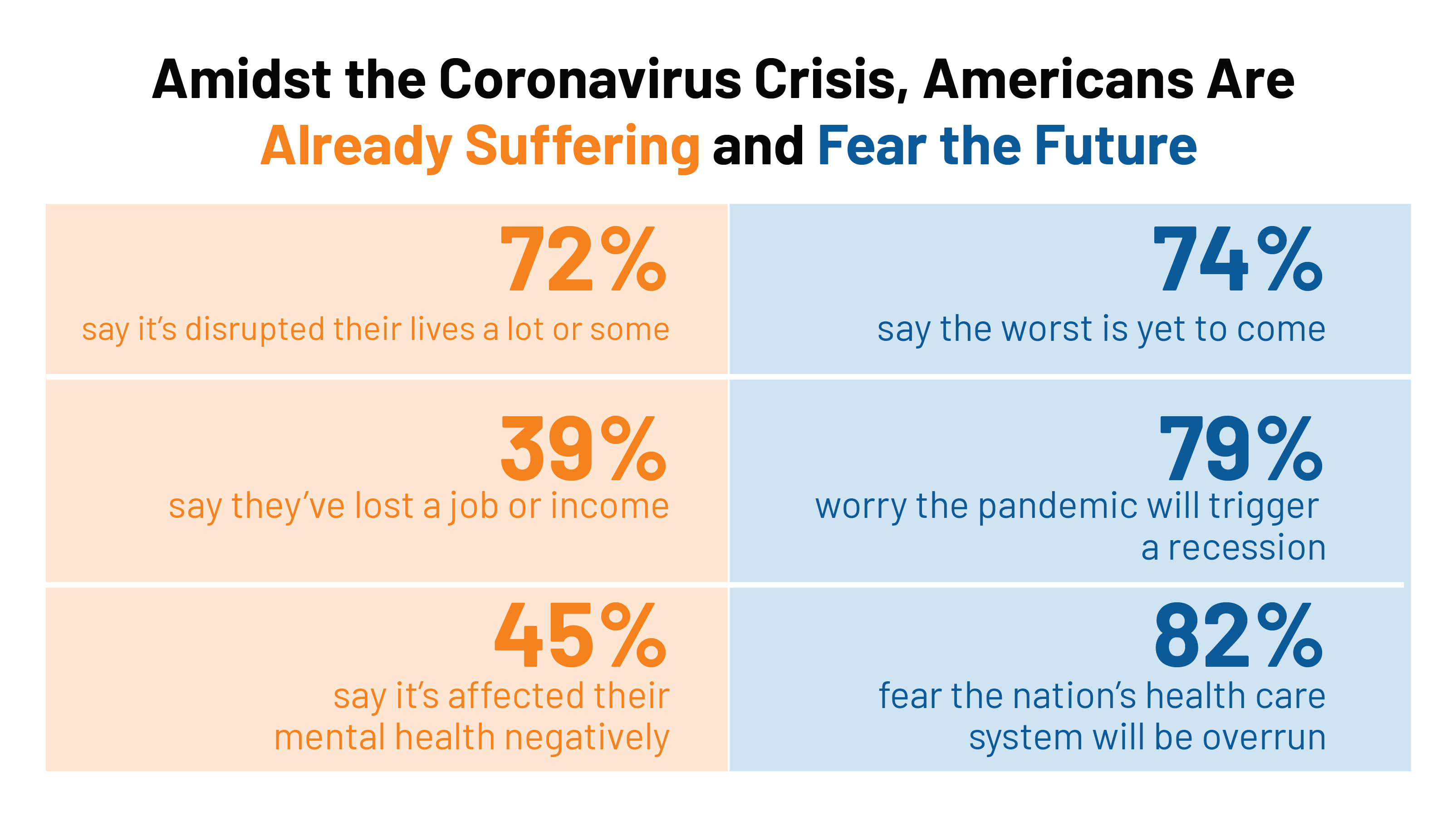
The Coronavirus Impact on American Life, Part 1 – Life Disrupted, and Money Concerns
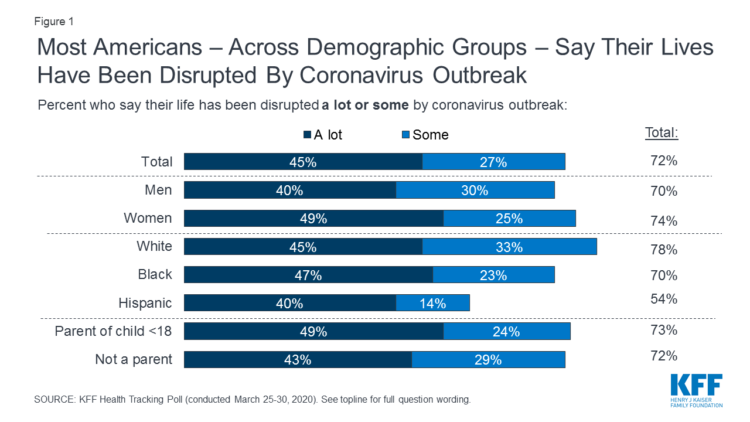
Nearly 3 in 4 Americans see their lives disrupted by the coronavirus pandemic, according to the early April Kaiser Family Foundation Health Tracking Poll. This feeling holds true across most demographic factors: among both parents and people without children; men and women alike; white folks as well as people of color (although fewer people identifying as Hispanic, still a majority). There are partisan differences, however, in terms of who perceives a life-disruption due to COVID-19: 76% of Democrats believe this, 72% of Independents, and 70% of Republicans. Interestingly, only 30% of Republicans felt this way in March 2020, more than
West Virginia Was the Last State to ID a COVID-19 Positive Patient; The States’ Residents Are At Highest Risk for Severe Reaction to C19
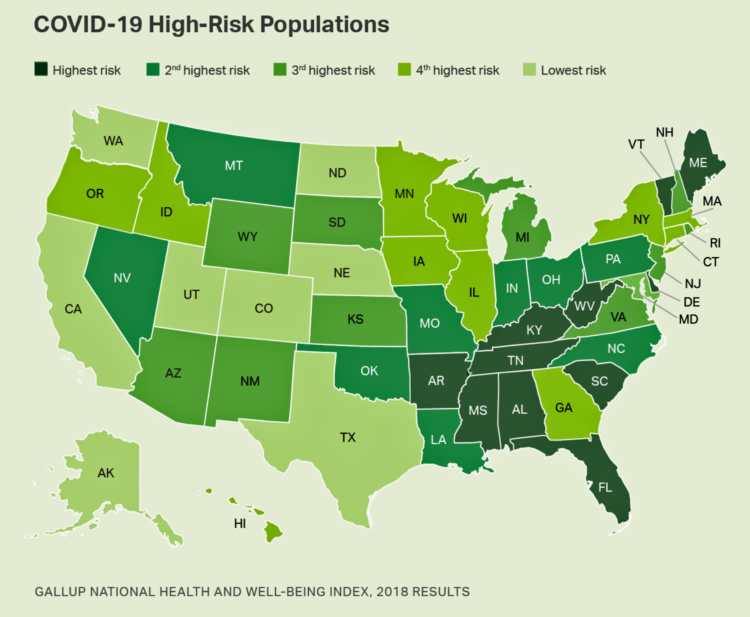
Gallup has estimated 11 Million in U.S. at Severe Risk If Infected With COVID-19 in research published today. And the health citizens of West Virginia would be at greatest risk for having a severe reaction to the coronavirus. A “severe reaction” here means being critically ill or dying. The forecast doesn’t focus on the whole number of people in the US. who would be at-risk of contracting the coronavirus; the 11 million is the total number of Americans who have a “very high chance of becoming critically ill or dying” if 100% of the country were infected with C19. This
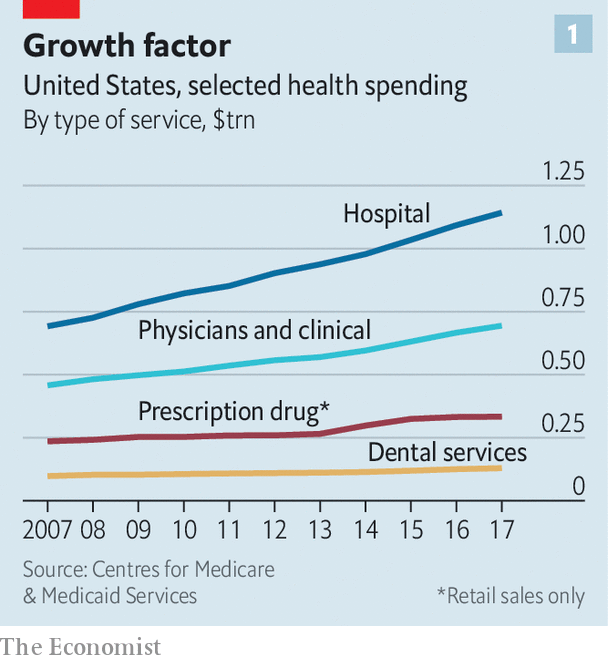
Wistful Thinking: The National Health Spending Forecast In a Land Without COVID-19
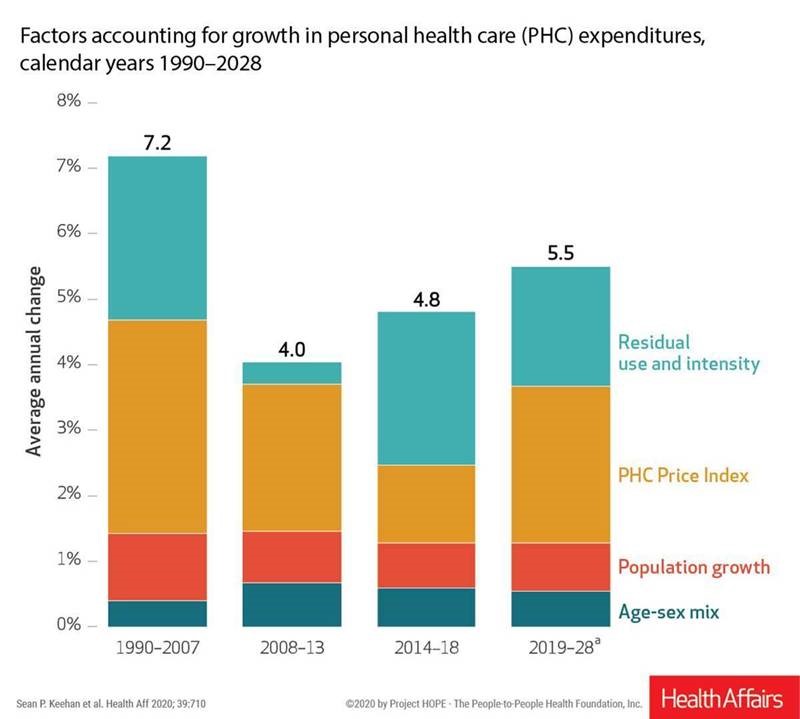
U.S. health care spending will grow to 20% of the national economy by 2028, forecasted in projections pre-published in the April 2020 issue of Health Affairs, National Health Expenditure (NHE) Projections. 2019-28: Expected Rebound in Prices Drives Rising Spending Growth. NHE will grow 5.4% in the decade, the model expects. But…what a difference a pandemic could make on this forecast. This year, NHE will be $3.8 trillion, growing to $6.2 trillion in 2028. Hospital care spending, the largest single component in national health spending, is estimated at $1.3 trillion in 2020. These projections are based on “current law,” the team
In the US COVID-19 Pandemic, A Tension Between the Fiscal and the Physical

“Act fast and do whatever it takes,” insists the second half of the title of a new eBook with contributions from forty leading economists from around the world. The first half of the title is, Mitigating the COVID Economic Crisis. The book is discussed in a World Economic Forum essay discussing the economists’ consensus to “act fast.” As the U.S. curve adds new American patients testing positive for the coronavirus, the book and essay illustrate the tension between health consumer versus the health citizen in the U.S. For clinical context, as I write this post on 24th March 2020, today’s U.S.
In A Nation “At War” with the C19 Virus, Partisan Healthcare Differences Persist
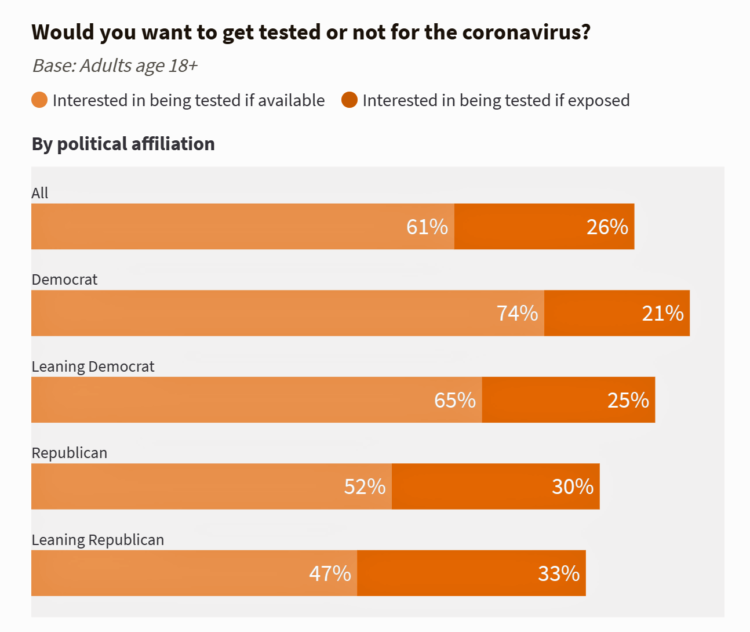
More Democrats would want to get tested for the coronavirus (C19) than would Republicans. And, more women than men believe that a vaccine to address the COVID-19 pandemic believe that treatment would be offered at no-or-low-cost under a Democratic president versus President Trump. These are two key insights gleaned from a look into U.S. adults’ perspectives on the C19 virus in the second week of March 2020. What Are Americans’ Views on the Coronavirus Pandemic? asks and answers an NBC News/Commonwealth Fund Health Care Poll published on 20th March 2020. NBC News and the Commonwealth Fund polled 1,006 people 18
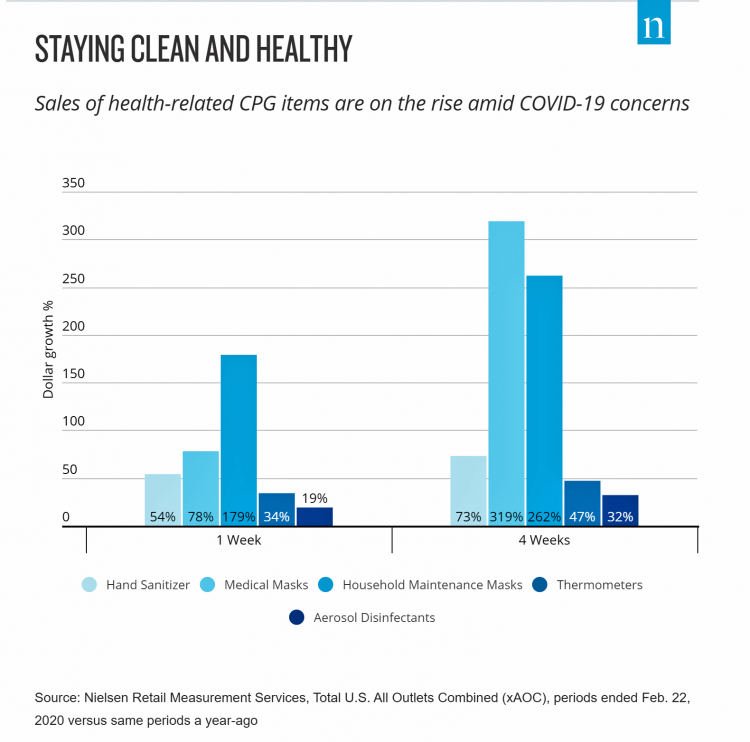
The COVID19 Consumer: #AloneTogether and More Health Aware
The number of diagnoses of people testing positive with the coronavirus topped 14,000 today in the U.S., Johns Hopkins COVID-19 interactive map told us this morning. As tests have begun to come on stream from California on the west coast to New York state on the east, the U.S. COVID-19 positives will continue to ratchet up for weeks to come, based on the latest perspectives shared by the most-trusted expert in America, Dr. Anthony Fauci. This report from the U.S. Department of Health and Human Services on the nation’s response to the coronavirus pandemic, published March 13, 2020, forecasts a
Shaky Trust in the Age of the Coronavirus – Who Do Americans Trust for COVID-19 Facts?
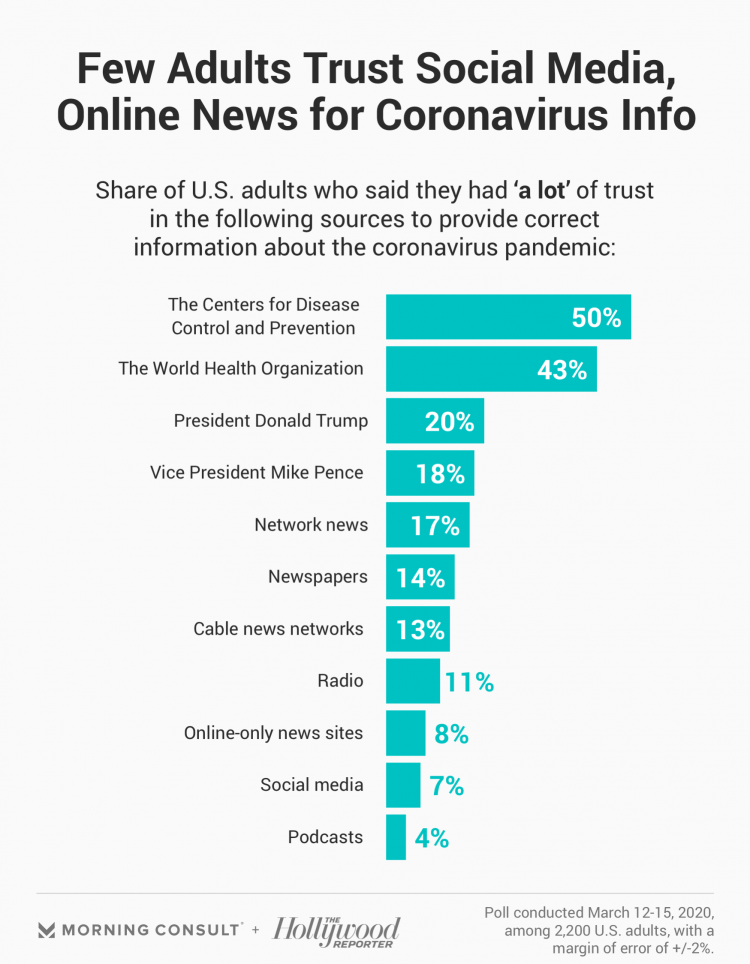
One in two Americans trust the Centers for Disease Control for the facts on the coronavirus pandemic, and 43% trust the World Health Organization. But there’s a huge trust deficit when it comes to trusting President Donald Trump on the facts about COVID-19, a poll from Morning Consult and The Hollywood Reporter found. 2,200 U.S. adults were surveyed between 12 and 15 March 2020 on the coronavirus pandemic and their perspectives on the media and political leaders’ information credibility. For news on the pandemic, only one in five Americans believed the President and 18%, the Vice President, Mike Pence, followed
Estimates of COVID-19 Medical Costs in the US: $20K for inpatient stay, $1300 OOP costs
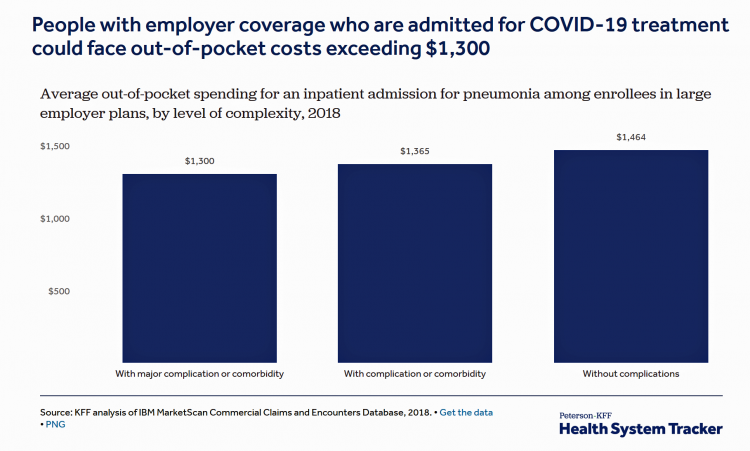
In the midst of growing inpatient admissions and test results for COVID-19, Congress is working as I write this post to finalize a round of legislation to help Americans with the costs-of-living and (hopefully) health care in a national, mandated, clarifying way. Right now in the real world, real patients are already being treated for COVID-19 in American hospitals. Patients are facing health care costs that may result in multi-thousand dollar bills at discharge (or death) that will decimate households’ financial health, particularly among people who don’t have health insurance coverage, covered by skinny or under-benefited plans, and/or lack banked
Lockdown Economics for U.S. Health Consumers

The hashtag #StayHome was ushered onto Twitter by 15 U.S. national healthcare leaders in a USA Today editorial yesterday. The op-ed co-authors included Dr. Eric Topol, Dr. Leana Wen, Dr. Zeke Emanuel, Dr. Jordan Shlain, Dr. Vivek Murthy, Andy Slavitt, and other key healthcare opinion leaders. Some states and regions have already mandated that people stay home; at midnight last night, counties in the Bay Area in California instituted this, and there are tightening rules in my area of greater Philadelphia. UBS economist Paul Donovan talked about “Lockdown Economics” in his audio commentary today. Paul’s observations resonated with me as
Telehealth and COVID-19 in the U.S.: A Conversation with Ann Mond Johnson, ATA CEO
Will the coronavirus inspire greater adoption of telehealth in the U.S.? Let’s travel to Shanghai, China where, “the covid-19 epidemic has brought millions of new patients online. They are likely to stay there,” asserts “The smartphone will see you now,” an article in the March 7th 2020 issue of The Economist. The article returns to the advent of the SARS epidemic in China in 2003, which ushered in a series of events: people stayed home, and Chinese social media and e-commerce proliferated. The coronavirus spawned another kind of gift to China and the nation’s health citizens: telemedicine, the essay explains. A
Waking Up a Health Consumer in the COVID-19 Era
With President Trump’s somber speech from the Oval Office last night, we wake up on 12th March 2020 to a ban on most travel from Europe to the U.S., recommendations for hygiene, and call to come together in America. His remarks focused largely on an immigration and travel policy versus science, triaging, testing and treatment of the virus itself. Here is a link to the President’s full remarks from the White House website, presented at about 9 pm on 11 March 2020. Over the past week, I’ve culled several studies and resources to divine a profile of the U.S. consumer
The Book on Deaths of Despair – Deaton & Case On Education, Pain, Work and the Future of Capitalism
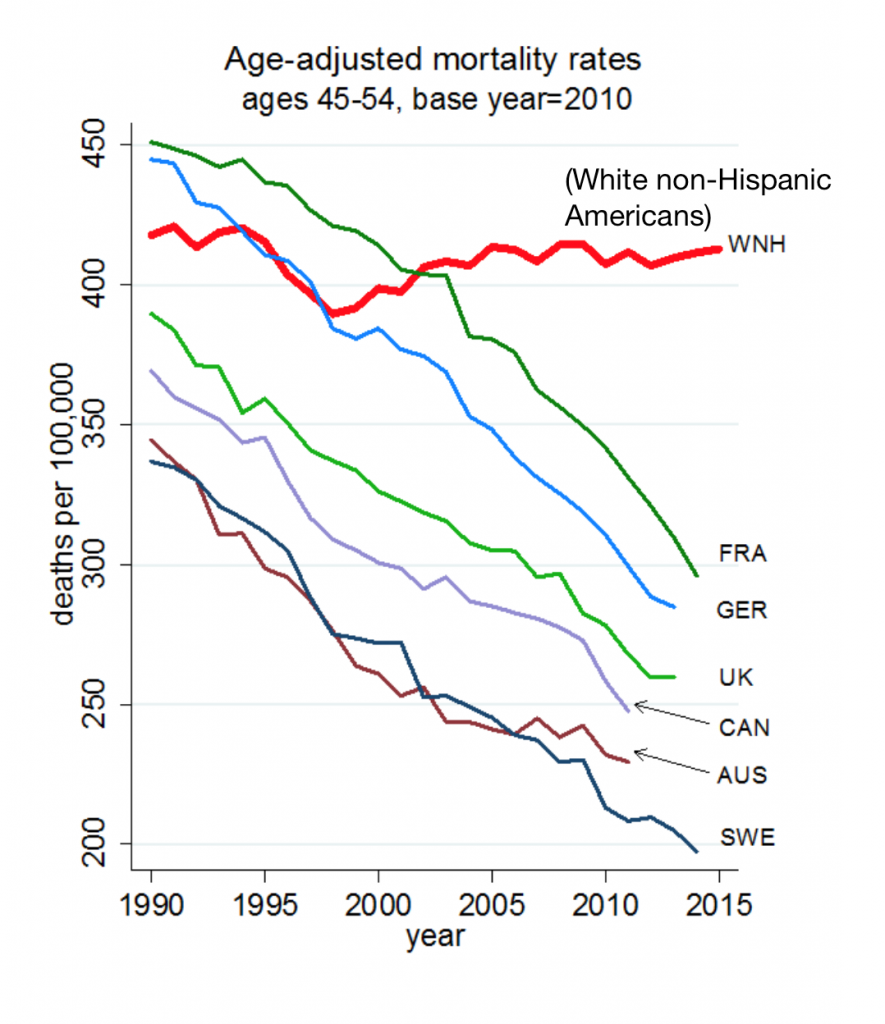
Anne Case and Angus Deaton were working in a cabin in Montana the summer of 2014. Upon analyzing mortality data from the U.S. Centers for Disease Control, they noticed that death rates were rising among middle-aged white people. “We must have hit a wrong key,” they note in the introduction of their book, Deaths of Despair and the Future of Capitalism. This reversal of life span in America ran counter to a decades-long trend of lower mortality in the U.S., a 20th century accomplishment, Case and Deaton recount. In the 300 pages that follow, the researchers deeply dive into and
Most Americans Concerned About Coronavirus Impact on Economy & Families, and Not a “Hoax”

Seven in 10 Americans are concerned about the coronavirus outbreak’s impact on the economy, and 6 in 10 people worried about someone they love getting sick from COVID-19. But most Americans also get the politicized nature of the coronavirus and say they’re less likely to vote for President Trump in November based on his handling of the public health threat, according to a just-released survey from Protect Our Care fielded by Public Policy Polling. Some of the data points which demonstrate that Americans are taking the emerging coronavirus pandemic quite seriously are that: 53% disagree that President Trump and his
How Coronavirus Is Re-Shaping Consumer Behavior, From the Amusement Park to the Voting Booth

The coronavirus has shaken U.S. consumer confidence, both in terms of financial markets and personal health risks. COVID-19 is re-shaping peoples’ behavior and daily choices, from using public transit to choosing where to shop, based on Morning Consult’s National Tracking Poll #200276 conducted February 28-March 1, 2020. Morning Consult surveyed 2,200 U.S. adults, finding that 3 in 4 Americans were concerned about the coronavirus outbreak. The first chart from the survey shows various consumer activities by peoples’ likelihood of choosing to do them. Clearly, our daily life-flows outside of our homes have been impacted by our perceived risks of the coronavirus:
Job #1 for Next President: Reduce Health Care Costs – Commonwealth Fund & NBC News Poll

Four in five U.S. adults say lowering the cost of health care in America should be high priority for the next American president, according to a poll from The Commonwealth Fund and NBC News. Health care costs continue to be a top issue on American voters’ minds in this 2020 Presidential election year, this survey confirms. The first chart illustrates that lowering health care costs is a priority that crosses political parties. This is true for all flavors of health care costs, including health insurance deductibles and premiums, out-of-pocket costs for prescription drugs, and the cost of long-term care. While
The High Cost-of-Thriving and the Evolving Social Contract for Health Care
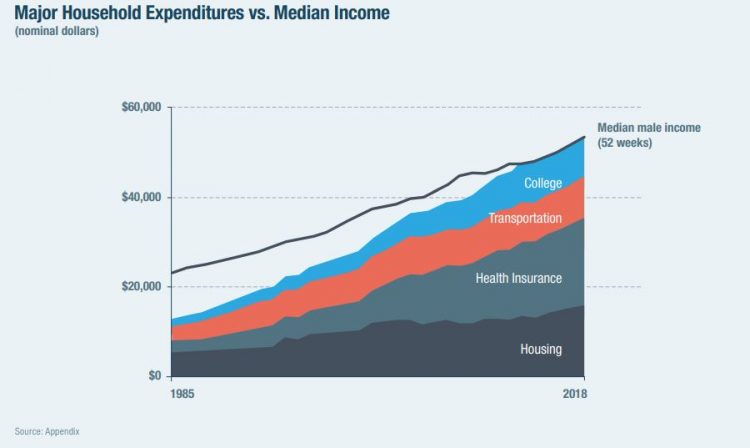
Millions of Americans have to work 53 weeks to cover a year’s worth of household expenses. Most Americans haven’t saved much for their retirement. Furthermore, the bullish macroeconomic outlook for the U.S. in early 2020 hasn’t translated into individual American’s optimism for their own family budgets. (Sidebar and caveat: yesterday was the fourth day in a row of the U.S. financial markets losing as much as 10% of market cap, so the global economic outlook is being revised downward by the likes of Goldman Sachs, Vanguard, and Morningstar, among other financial market prognosticators. MarketWatch called this week the worst market
Americans’ Top 2 Priorities for President Trump and Congress Are To Lower Health Care and Rx Costs
Health care pocketbook issues rank first and second place for Americans in these months leading up to the 2020 Presidential election, according to research from POLITICO and the Harvard Chan School of Public Health published on 19th February 2020. This poll underscores that whether Democrat or Republican, these are the top two domestic priorities among Americans above all other issues polled including immigration, trade agreements, infrastructure and regulations. The point that Robert Blendon, Harvard’s long-time health care pollster, notes is that, “Even among Democrats, the top issues…(are) not the big system reform debates…They’re worried about their own lives, their own
The Ill Health of Rural Hospitals in Four Charts
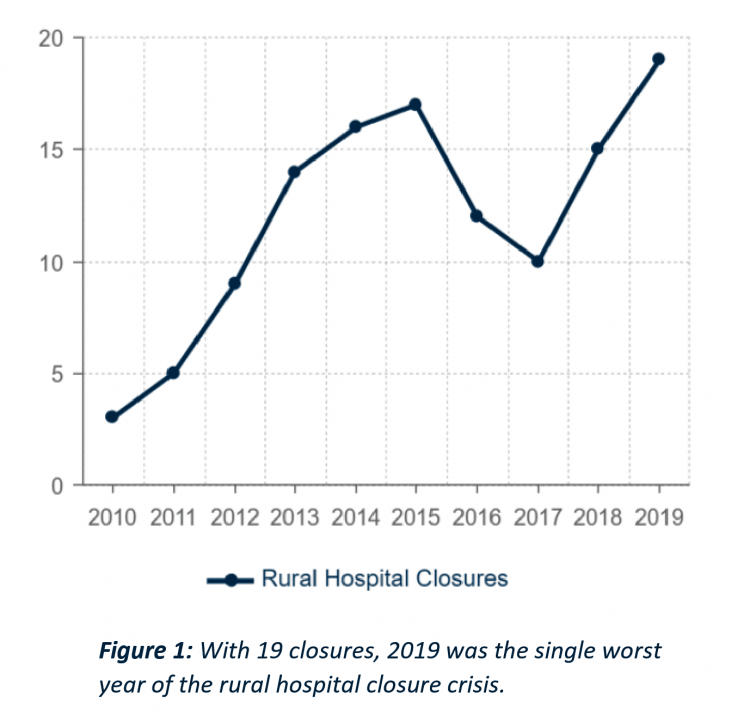
There are 1,844 rural hospitals operating in the U.S. That number is down by 19 in the 2019 calendar year, the worst year of rural hospital closings seen in the past decade. That hockey-stick growth of closures is shown in the first chart, where 34 rural hospitals shut down in the past 2 years. Rural U.S. hospitals are in poor fiscal health. “The accelerated rate at which rural hospitals are closing continues to unsettle the rural healthcare community and demands a more nuanced investigation into rural hospital performance,” threatening the stability of the rural health safety net, according to the
The Federal Reserve Chairman Speaks Out on Health Care Costs: “Spending But Getting Nothing”
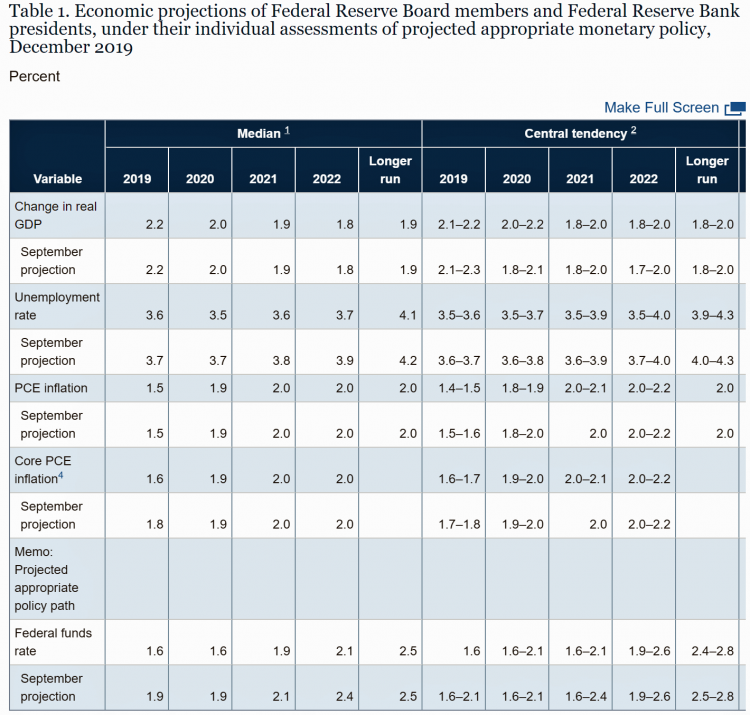
On February 12, 2020, the Chairman of the Federal Reserve Bank of the U.S. submitted the Semiannual Monetary Policy Report to Congress and testified to the Senate Banking Committee. Chairman Jerome Powell detailed the current state of the economy, discussing the state of the macroeconomy, GDP growth, unemployment, inflation, and projections for 2022 and beyond. The top line data points are shown in the first chart. After his prepared remarks, Chairman Powell responded to questions from members of the Senate Banking Committee. Senator Ben Sasse (R-Neb.) asked him about health care costs’ impact on the national U.S. economy. The Chairman
Health Care Costs Concern Americans Approaching Retirement – Especially Women and Sicker People
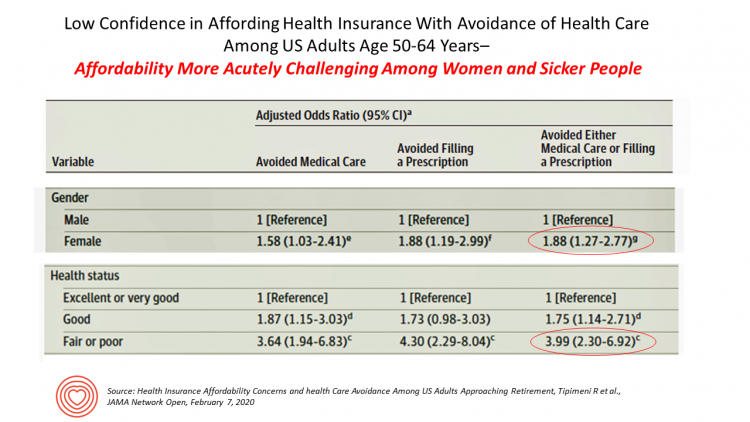
Even with the prospect of enrolling in Medicare sooner in a year or two or three, Americans approaching retirement are growing concerned about health care costs, according to a study in JAMA Network Open. The paper, Health Insurance Affordability Concerns and health Care Avoidance Among US Adults Approaching Retirement, explored the perspectives of 1,028 US adults between 50 and 64 years of age between November 2018 and March 2019. The patient survey asked one question addressing two aspects of “health care confidence:” “Please rate your confidence with the following:” Being able to afford the cost of your health insurance nad
USA Today Finds Hidden Common Ground Among Americans For Health Care
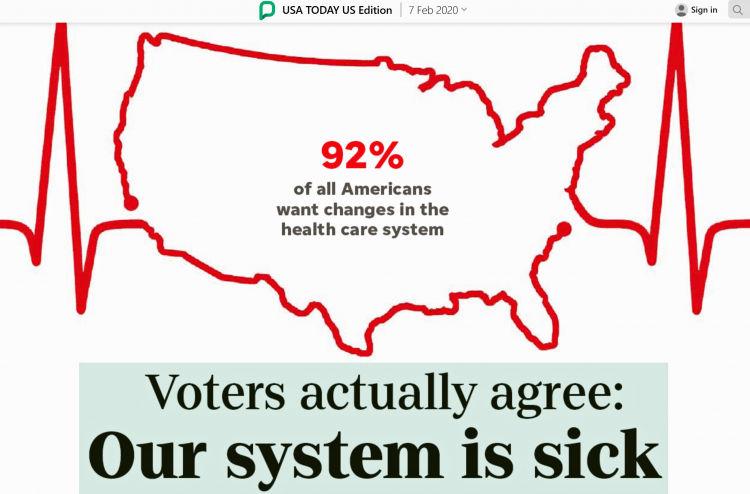
“We need to demand our health citizenship. That means our nation must approach medical treatment and data privacy as civil rights that protect everyone.” This is the start of my column, Americans, let’s claim our health care rights, published by USA Today today. USA Today is publishing a 10-part series called “Hidden Common Ground” addressing key issues where Americans can come together. Thus far, the series has covered climate change, and this month health care. Going forward, we’ll see analyses on jobs, gun rights and violence, and immigration through May’s publishing schedule. In their study conducted in December 2020, USA Today
Come Together – A Health Policy Prescription from the Bipartisan Policy Center
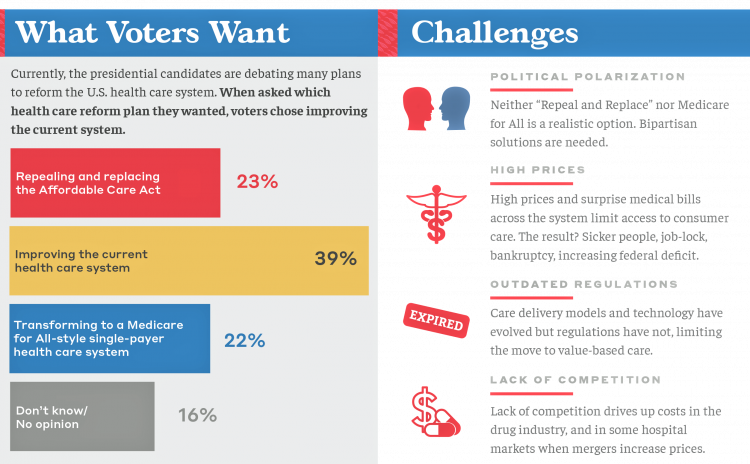
Among all Americans, the most popular approach for improving the health care in the U.S. isn’t repealing or replacing the Affordable Care Act or moving to a Medicare-for-All government-provided plan. It would be to improve the current health care system, according to the Bipartisan Policy Center’s research reported in a Bipartisan Rx for America’s Health Care. The BPC is a truly bipartisan organization, co-founded by Former Democratic Senate Majority Leaders Tom Daschle and George Mitchell, and Former Republican Senate Majority Leaders Howard Baker and Bob Dole. While this political week in America has revealed deep chasms between the Dems and
What’s Causing Fewer Primary Care Visits in the US?
Americans who have commercial health insurance (say, through an employer or union) are rarely thought to face barriers to receiving health care — in particular, primary care, that front line provider and on-ramp to the health care system. But in a new study published in the Annals of Internal Medicine, commercially-insured adults were found to have visited primary care providers (PCPs) less often, and 1 in 2 had no PCP visits in one year. In Declining Use of Primary Care Among Commercially Insured Adults in the United States, 2008-2016, the researchers analyzed data from a national sample of adult health
The State of the Union for Prescription Drug Prices
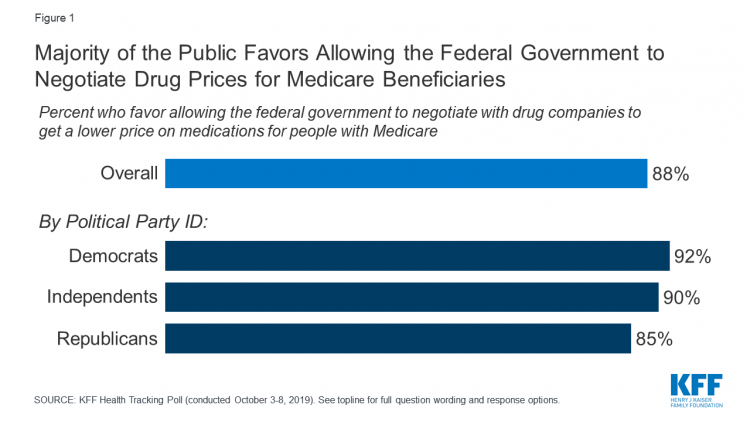
Tonight, President Trump will present his fourth annual State of the Union address. This morning we don’t have a transcript of the speech ahead of the event, but one topic remains high on U.S. voters’ priorities, across political party – prescription drug prices. Few issues unite U.S. voters in 2020 quite like supporting Medicare’s ability to negotiate drug prices with pharmaceutical companies, shown by the October 2019 Kaiser Family Foundation Health Tracking Poll. Whether Democrat, Independent, or Republican, most people living in America favor government intervention in regulating the cost of medicines in some way. In this poll, the top
Most Americans Are Curious and Hopeful About Genetics Research, But Privacy-Concerned
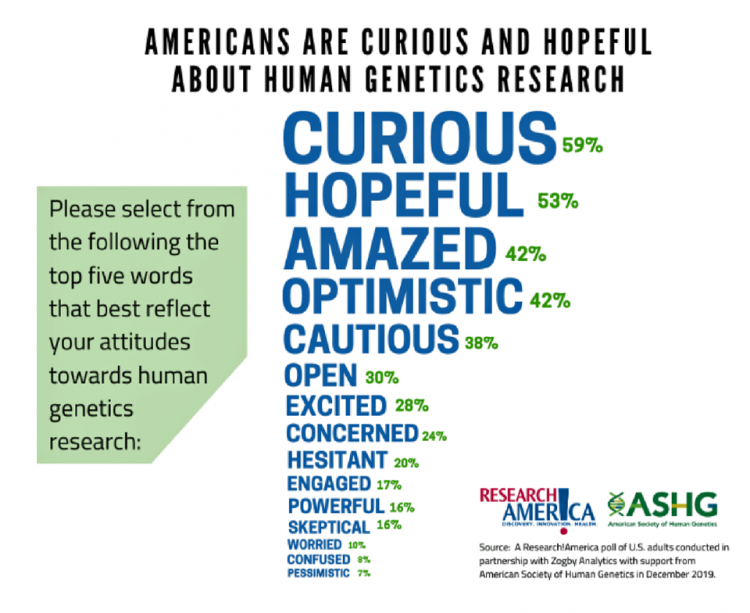
Most Americans associate more optimistic words with human genetics research than they do darker implications: “curious,” “hopeful,” “amazed.” and indeed “optimistic” ranked the top four impressions in peoples’ minds, based on a survey form the American Society of Human Genetics (ASHG). Below these perceptions are a few concerning concepts such as “cautious,” “concerned,” “hesitant, and “skeptical,” the poll found. Based on the relatively positive views on genetics research, most Americans support increasing Federal funding for that research: 74% said it was somewhat or very important to do so, compared with 15% saying it was not important. People value genetics research
A Uniting Issue in the United States is Lowering Prescription Drug Costs
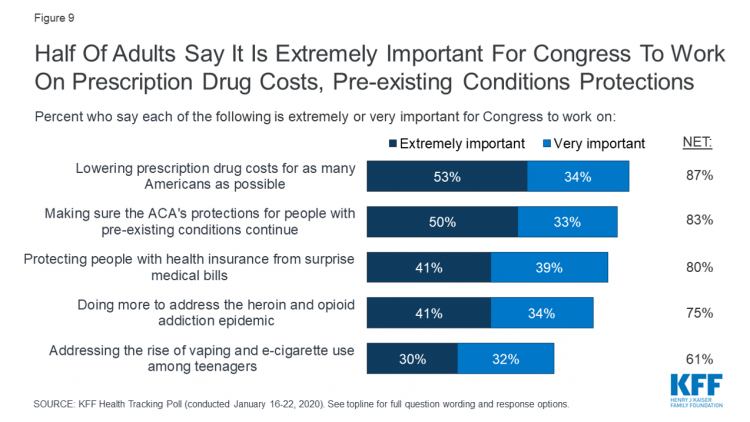
Health care continues to be the top-ranked voting issue in the U.S. looking to the November 2020 Presidential and Congressional elections. The Kaiser Family Foundation conducts the monthly poll which gauges U.S. adults’ perspectives on health care, and this month’s January 2020 Kaiser Health Tracking Poll explores Americans’ views on broad healthcare reform plans and specific medical policy issues. Overall, Americans point to prescription drug costs and the preservation of the Affordable Care Act’s protections for people with pre-existing conditions, the first chart tells us. Third and fourth on voters’ minds are protecting patients from surprise medical bills and better
Most Americans Regardless of Income Say It’s Unfair for Wealthier People to Get Better Health Care
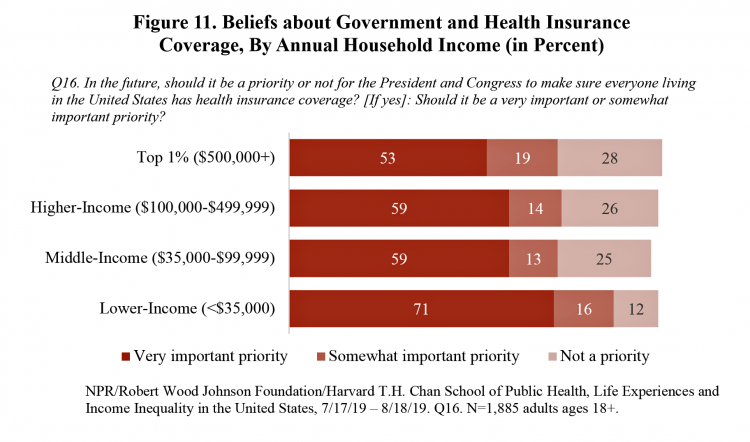
In America, earning lower or middle incomes is a risk factor for having trouble accessing health care and/or paying for it. But most Americans, rich or not, believe that it’s unfair for wealthier people to get better health care, according to a January 2020 poll from NPR, the Robert Wood Johnson Foundation and Harvard Chan School of Public Health, Life Experiences and Income Equality in the United States. The survey was conducted in July and August 2019 among 1,885 U.S. adults 18 or older. Throughout the study, note the four annual household income categories gauged in the research: Top 1%
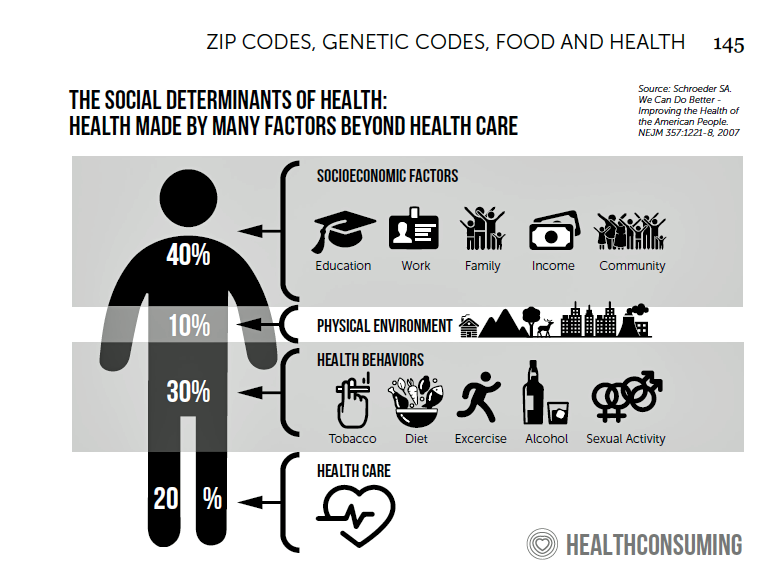
The 2020 Social Determinants of Health: Connectivity, Art, Air and Love
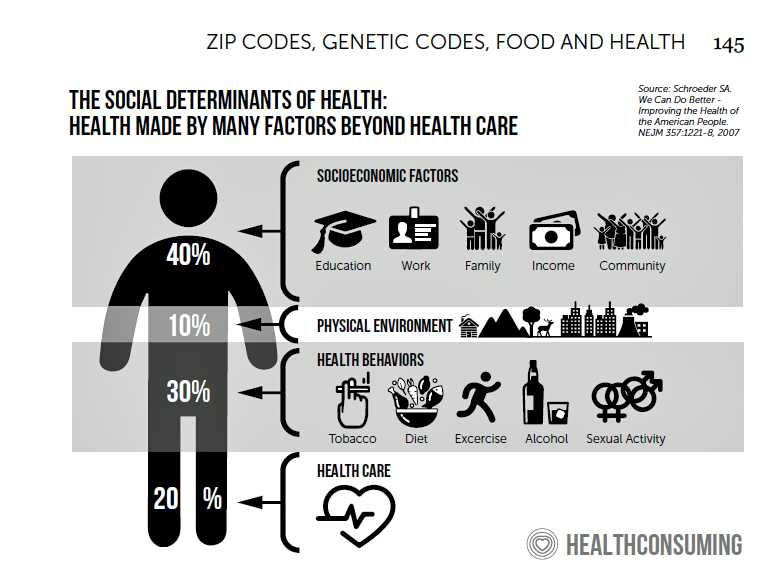
Across the U.S., the health/care ecosystem warmly embraced social determinants of health as a concept in 2019. A few of the mainstreaming-of-SDoH signposts in 2019 were: Cigna studying and focusing in on loneliness as a health and wellness risk factor Humana’s Bold Goal initiative targeting Medicare Advantage enrollees CVS building out an SDOH platform, collaborating with Unite US for the effort UPMC launching a social impact program focusing on SDoH, among other projects investing in social factors that bolster public health. As I pointed out in my 2020 Health Populi trendcast, the private sector is taking on more public health
In 2020, PwC Expects Consumers to Grow DIY Healthcare Muscles As Medical Prices Increase

The new year will see a “looming tsunami” of high prices in healthcare, regulation trumping health reform, more business deals reshaping the health/care industry landscape, and patients growing do-it-yourself care muscles, according to Top health industry issues of 2020: Will digital start to show an ROI from the PwC Health Research Institute. I’ve looked forward to reviewing this annual report for the past few years, and always learn something new from PwC’s team of researchers who reach out to experts spanning the industry. In this 14th year of the publication, PwC polled executives from payers, providers, and pharma/life science organizations. Internally,
Food As Medicine: Grocery Stores Expand as Health Destinations While the Federal Government Cuts Food Stamps
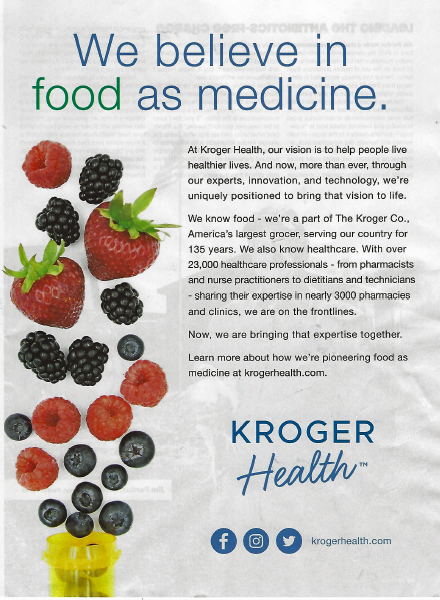
There’s something like cognitive dissonance as I prepare my 2020 Health Populi TrendCast of what to expect in the health/care ecosystem in the new year. One of my key pillars for health-making is food-as-medicine, and that opportunity in this moment resonates in this holiday season with Dickens’ “Best of Times, Worst of Times” context-setting that kicks off Great Expectations. In the “best of times” part of the food+health equation, we recognize the growing role of grocery stores, food-tech and food manufacturers in the health/care landscape. A current example comes from Kroger, partnering with Ascension’s health system in Tennessee, enhancing the organization’s
The Patient As Payor: Workers Covered by Employer Health Insurance Spend 11.5% of Household Incomes on Premiums and Deductibles
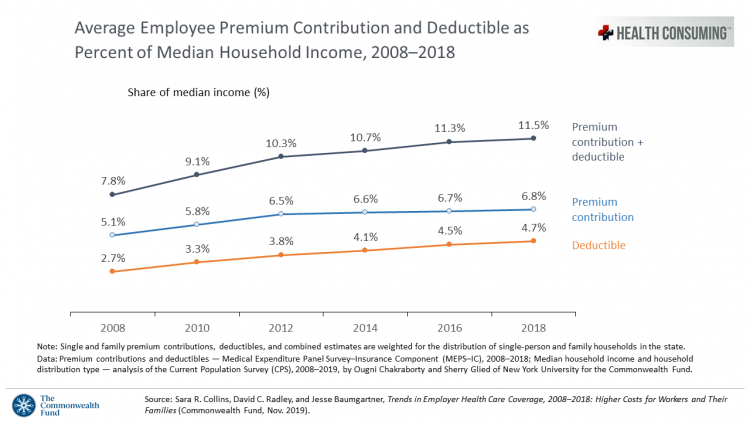
Workers covered by health insurance through their companies spend 11.5% of their household income on health insurance premiums and deductibles based on The Commonwealth Fund’s latest report on employee health care costs, Trends in Employer Health Coverage, 2008-2018: Higher Costs for Workers and Their Families. The topline of this study is that average annual growth in employer premiums rose faster between 2016 and 2017, by about 5% for both single and family plans. The bottom line for families is that workers’ premium payments grew faster than median incomes did over the ten years 2008 to 2018. Average deductibles also outpaced
Being Transparent About Healthcare Transparency – My Post on the Medecision Blog
With new rules emanating from the White House this month focusing on health care price transparency, health care costs are in the spotlight at the Centers for Medicare and Medicaid Services. A hospital transparency mandate will go into effect in January 2021 as a final rule, and a second rule with a focus on health plans and friendly explanations-of-benefits will receive comments in the Federal Register until January 14, 2020. As patients continue to grow muscles as payors and health consumers, transparency is one key to enabling people to “shop” for those health care and medical products and services that
Social Determinants of Health – My Early Childhood Education and Recent Learnings, Shared at the HealthXL Global Gathering
My cousin Arlene got married in Detroit at the classic Book Cadillac Hotel on July 23, 1967, a Sunday afternoon wedding. When Daddy drove us back out to our suburban home about 30 minutes from the fancy hotel, the car radio was tuned to WWJ Newsradio 950, all news all the time. As soon as Daddy switched on the radio, we were shocked by the news of a riot breaking out in the city, fires and looting and gunshots and chaos in the Motor City. Two days later, my father, who did business with Mom-and-Pop retail store owners in the
More Evidence of Self-Rationing as Patients Morph into Healthcare Payors

Several new studies reveal that more patients are feeling and living out their role as health care payors as medical spending vies with other household line items. This role of patient-as-the-payor crosses consumers’ ages and demographics, and is heating up health care as the top political issue for the 2020 elections at both Federal and State levels. In research from HealthPocket, 2 in 5 Americans said they needed to reduce other household expenses to be able to afford their monthly insurance premiums. Four in ten consumers said their monthly health insurance premiums were increasing. One in four people in the
A Tale of Two Americas as Told by the 2019 OECD Report on Health

It was the best of times, It was the worst of times, It was the age of wisdom, it was the age of foolishness, It was the epoch of belief, it was the epoch of incredulity, … starts Dickens’ Tale of Two Cities. That’s what came to my mind when reading the latest global health report from the OECD, Health at a Glance 2019, which compares the United States to other nations’ health care outcomes, risk factors, access metrics, and spending. Some trends are consistent across the wealthiest countries of the world, many sobering, such as: Life expectancy rates fell in 19 of the
The Link Between Wellness & Wealth Is Powerful for Everyone – and Especially Women

In the U.S., the link between wellness and wealth, money and health, is strong and common across people, young and old. But the impacts of money on health, well-being, and life choices varies across the ages, based on a study from Lively, a company that builds platforms for health savings accounts. The first chart illustrates that health care costs challenge people in many ways: the most obvious health care cost problems prevent people from saving more for retirement or paying down debt. Eight in 10 Americans concur that rising health care costs challenge their ability to save for retirement. Beyond the
Great Expectations for Health Care: Patients Look for Consumer Experience and Trust in Salesforce’s Latest Research

On the demand side of U.S. health care economics, patients are now payors as health consumers with more financial skin in paying medical bills. As consumers, people have great expectations from the organizations on the supply side of health care — providers (hospitals and doctors), health insurance plans, pharma and medical device companies. But as payors, health consumers face challenges in getting care, so great expectations are met with frustration and eroding trust with the system, according to the latest Connected Healthcare Consumer report from Salesforce published today as the company announced expansion of their health cloud capabilities. This is
Thinking About Health Care One Year From the 2020 Presidential Election

Today is 4th November 2019, exactly one year to the day that Americans can express their political will and cast their vote for President of the United States. Health care will be a key issue driving people to their local polling places, so it’s an opportune moment to take the temperature on U.S. voters’ perspectives on healthcare reform. This post looks at three current polls to gauge how Americans are feeling about health care reform 365 days before the 2020 election, and one day before tomorrow’s 2019 municipal and state elections. Today’s Financial Times features a poll that found two-thirds
Will Consumers Cross the Cost-and-Trust Chasm Between Prescription Drugs and Hospitals?
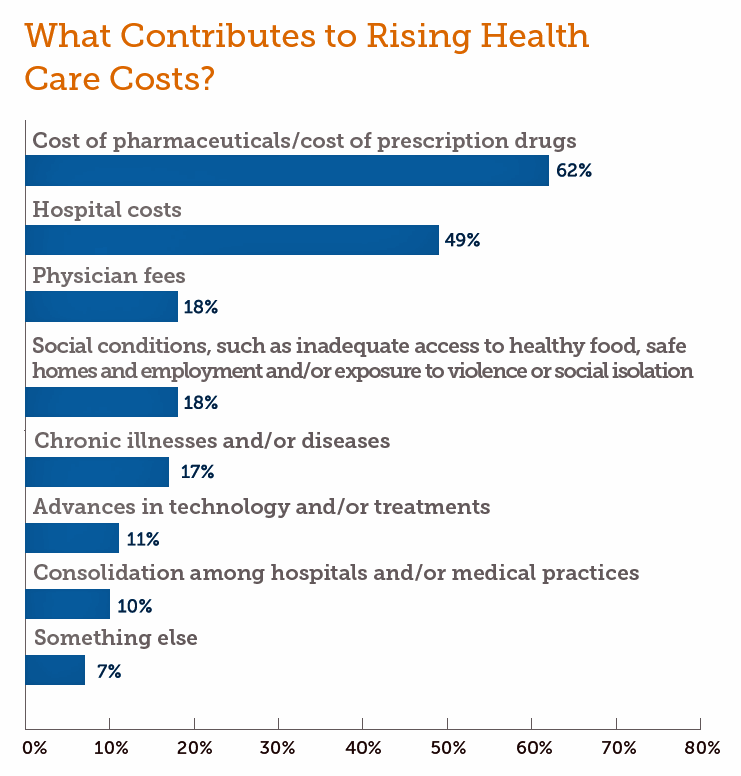
People in the U.S. rank prescription drugs, lab tests, emergency room visits, dental and vision care, preventive services, chronic disease management and mental health care as the “most essential” health care services, according to the 2019 Survey of America’s Patients conducted by The Physicians Foundation. When asked what factors contribute to rising health care costs in America, most consumers cite the cost of prescription drugs. Taken together, these two data points demonstrate the potent political import of prescription drug prices as the U.S. approaches the 2020 Presidential election. The Physicians Foundation surveyed 2,001 U.S. adults between 27 and 75 years
While Costs Are A Top Concern Among Most U.S. Patients, So Are Challenges of Poverty, Food, and Housing
Rising health care costs continue to concern most Americans, with one in two people believing they’re one sickness away from getting into financial trouble, according to the 2019 Survey of America’s Patients conducted for The Physicians Foundation. In addition to paying for “my” medical bills, most people in the U.S. also say that income inequality and inadequate social services significantly contribute to high medical spending for every health citizen in the nation. The Physicians Foundation conducts this study into Americans’ views on the U.S. health care system every other year. This year’s poll was conducted in September 2019 and included input
Wasted: $1 of Every $4 Spent on Health Care In America
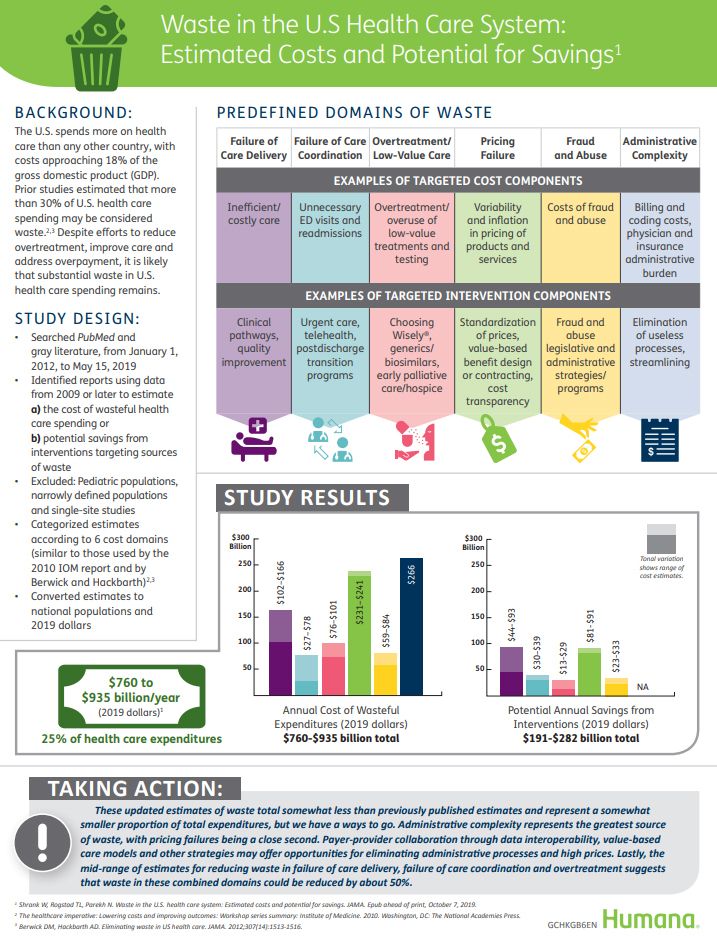
A study in JAMA published this week analyzed research reports that have measured waste in the U.S. health care system, calculating that 25% of medical spending in America is wasted. If spending is gauged at $3.8 trillion, waste amounts to nearly $1 trillion. If spending is 18% of the American gross domestic product (GDP), then some 4.5% of the U.S. economy is wasted spending by the health care system and its stakeholders. In “Waste in the US Health Care System,” a team from Humana and the Univrsity of Pittsburgh recalibrated the previous finding of 30% of wasted spending to the 25%,
Most U.S. Voters Support Building on the ACA, Not Medicare For All, As Fewer Americans Have Insurance Coverage
The vast majority of Americans favor lowering the cost of prescriptions, keeping the Affordable Care Act’s provisions to cover pre-existing conditions, lower overall medical costs, and protect people from surprise medical bills, according to the KFF Health Tracking Poll – September 2019: Health Care Policy In Congress And On The Campaign Trail. The big headline in this poll following last night’s third Democratic Presidential debate is that 55% of Democrats and Democrat-leaning Independent voters prefer a candidate that will build on the Affordable Care Act (ACA) versus a President that would replace the ACA with a Medicare For All plan (M4A).




 Thank you FeedSpot for
Thank you FeedSpot for