Consumers’ Favorite Brands for 2025 Look a Lot Like Pandemic Times: All About Hygiene, Safety, Personal Care, and Packages

Shades of the year 2020; it’s déjà vu all over again when it comes to consumers’ most trusted brands in 2025 featured in Morning Consult’s Most Reputable Brands report. Here’s the list of the top 25 most trusted brands across all consumer touch-points and industries for all adults, ages 18 and older. A quick calculation reveals that consumers most trust brands covering, Home keeping and hygiene – Dawn, Clorox, Lysol, Mr. Clean, Home Depot Self- and personal care – Dove, Oral-B, Kleenex, Colgate Health – BAND-AID, Tylenol Packages
That Big Beautiful Bill’s Healthcare Proposals Aren’t So Pretty in the Views of Most People in the U.S. – Including Josh Hawley (R-Mo.) – Listening to the Kaiser Family Foundation June Health Tracking Poll

Across all U.S. voters, the so-called “Big Beautiful Bill” Act (BBB) is seen unfavorably by nearly a 2:1 margin. Underneath that top-line, Democrats, Independents, and non-MAGA Republicans oppose it, while MAGA supporters favor it. But favorability erodes when people hear about possible health impacts, we learn in the June 2025 Health Tracking Poll from the Kaiser Family Foundation. The details on views of the BBB Act are shown in the first bar chart, with overwhelming disfavor among Democrats and Independents, and majority unfavorability among non-MAGA GOP supporters. Next check into partisans’ lenses
Most Americans Don’t Want to Cut Medicaid (Including Republicans)
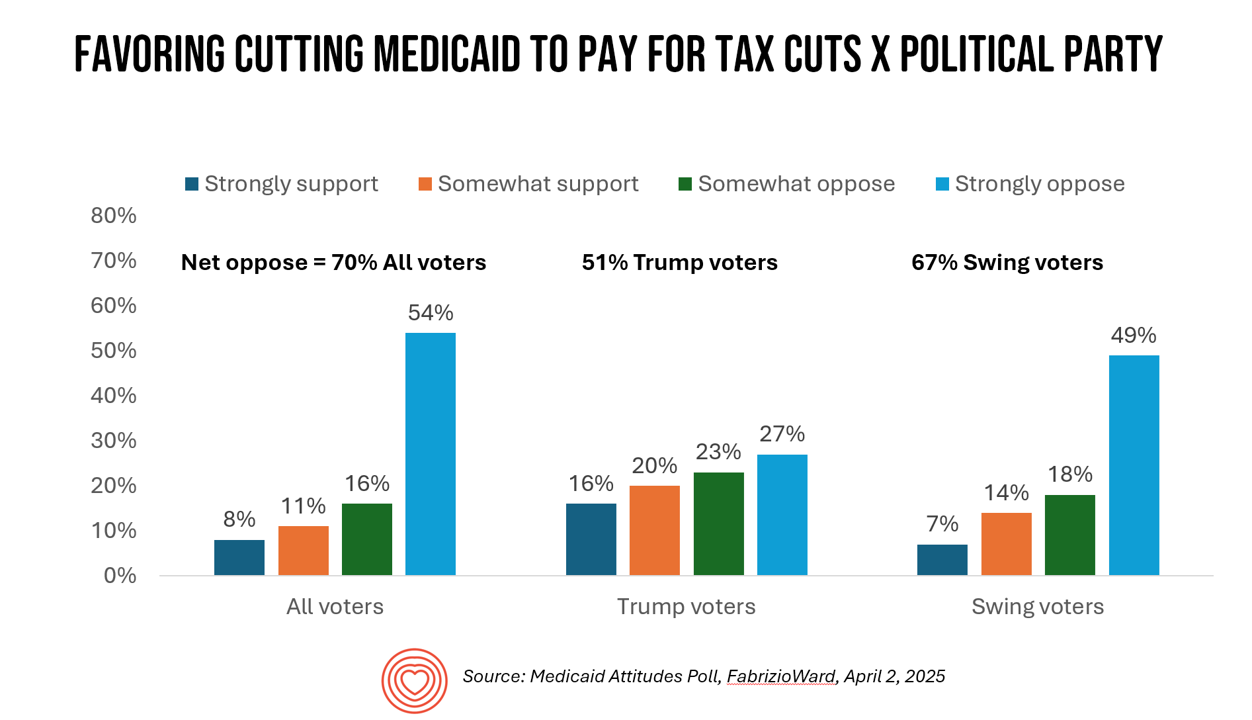
With potential down-sizing of Medicaid on the short-term U.S. political horizon, a fascinating poll found that most people identifying as Republican would not favor cuts to Medicaid. What fascinates me about this survey, published earlier this week, is that it was conducted by FabrizioWard, a polling firm that has often been used by President Trump. The firm’s Bob Ward told POLITICO that, “There’s really not a political appetite out there to go after Medicaid to pay for tax cuts. Medicaid has touched so many families that people have made up their minds about what
GLP-1s at the Pharmacy – A Lens on Consumer-Driven Retail Health (with Hims & Hers stock price update)
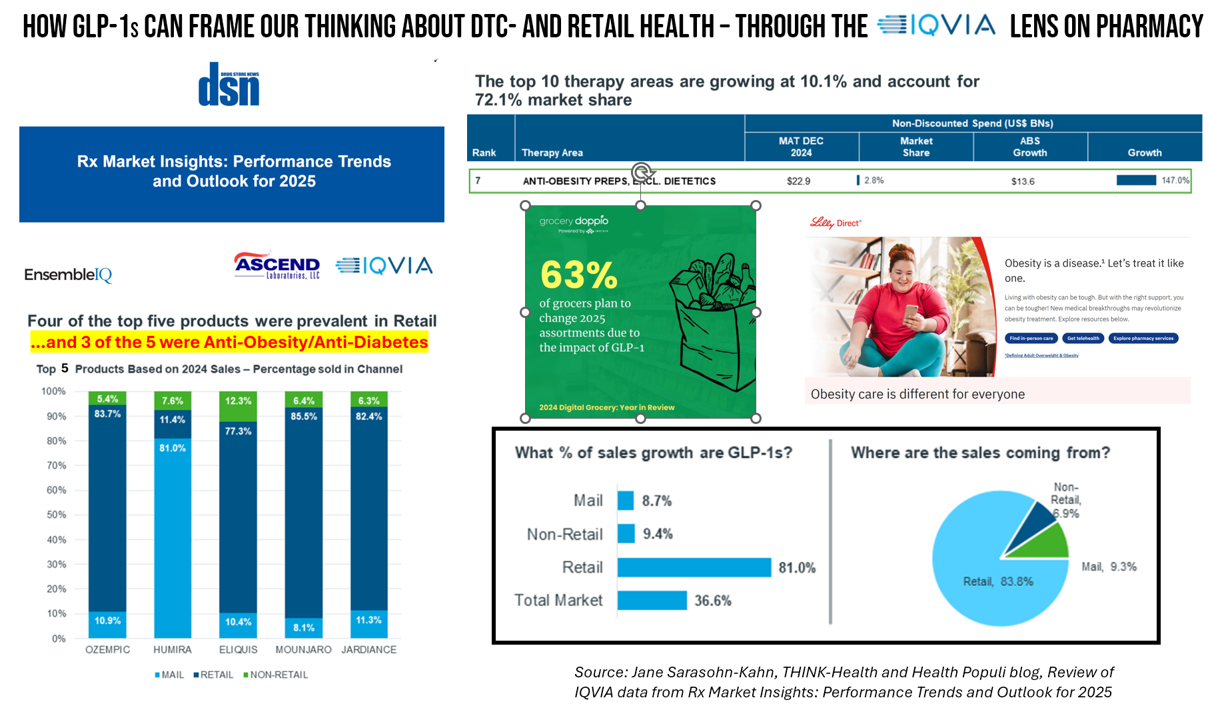
The nature of retail pharmacy is changing, with both threats and opportunities re-shaping the business itself, and the pharmacy’s role in the larger health/care ecosystem. To keep sharp on the topics, I attended Rx Market Insights: Performance Trends and Outlook for 2025, a data-rich session presented on February 18 by IQVIA and sponsored by Ascend Laboratories. The webinar was hosted by DSN (Drug Store News), appropriately so because the action-packed hour went into detail providing the current state of prescription drugs and the pharmacy in America. Doug Long, IQVIA’s VP of Industry Relations, and Scott Biggs, the company’s Director of Supplier
Most People in the U.S. Trust the CDC and NIH for Health Information, and Most Want President Trump to Strengthen Health Institutions
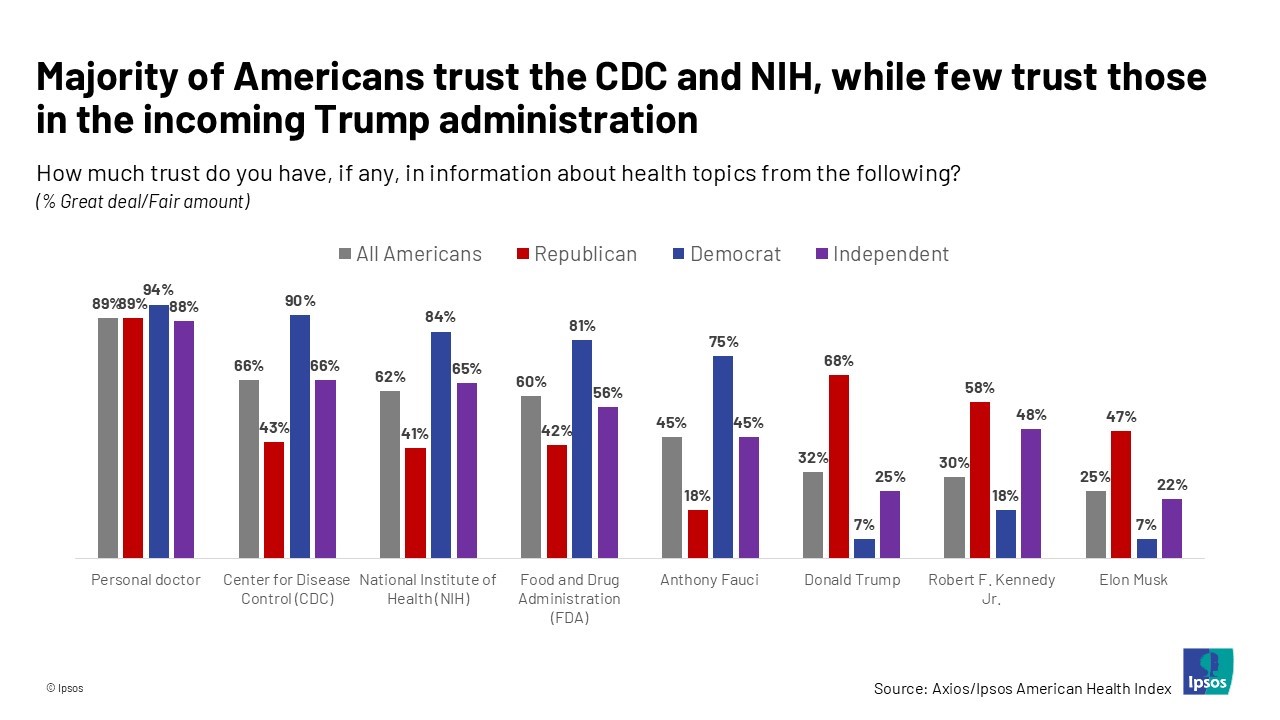
Most health citizens in the U.S. trust the CDC, NIH, and FDA, and most people also want the 47th incoming President Donald Trump to strengthen health/care institutions — from the VA and FDA to Medicare, Medicaid, as well as the CDC and Affordable Care Act. The Axios/Ipsos American Health Index, published this week, reveals both concurrence among U.S. health consumers with some striking differences across political party ID. Axios and Ipsos fielded a survey among 1,002 U.S. adults in early December to glean peoples’ perspectives on health, trust, and a variety of health and social policies.
Americans’ Views on the Quality of Healthcare Fell to a Record Low — with Costs Ranking as the Most Urgent Problem for Health in the U.S.
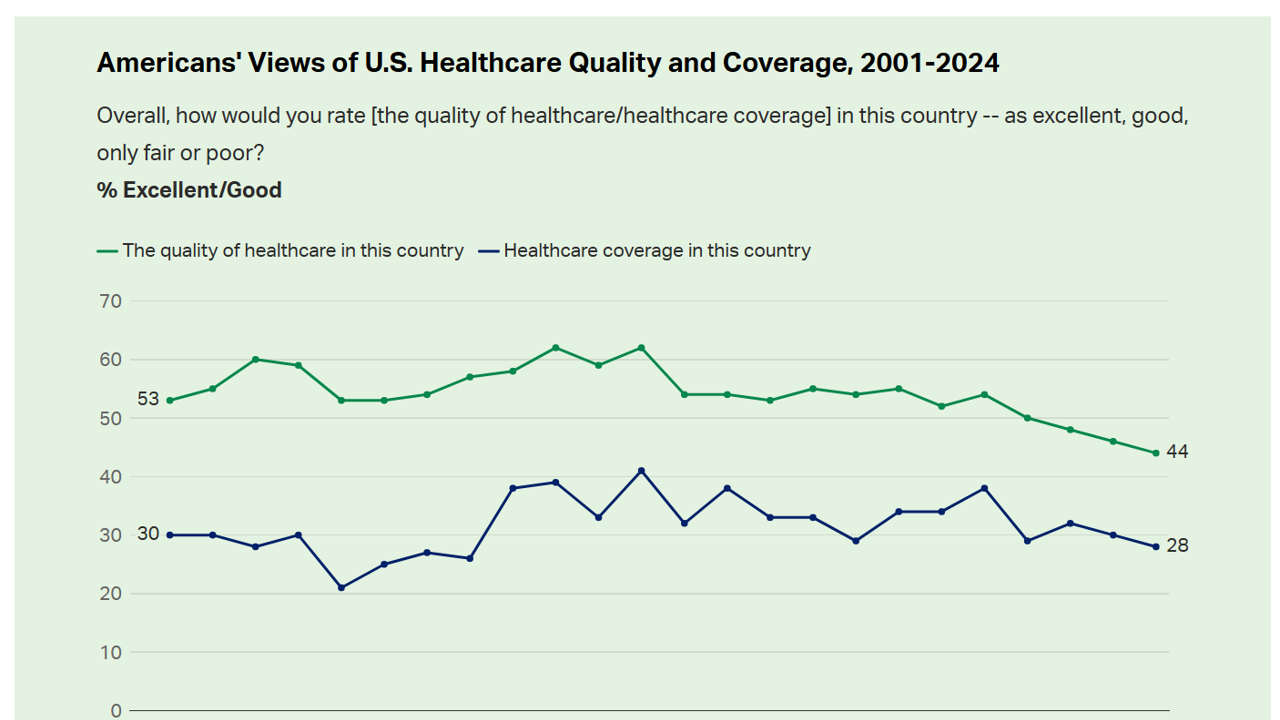
Americans’ perception of the quality of health care in the U.S. fell to the lowest level since 2001, Gallup found in a poll of U.S. health citizens’ views on health care quality, published December 6, 2024. In 2024, only 44% of Americans said that the quality of health care int he U.S. was excellent or good — conversely, 56% of Americans though health care quality was only fair or poor. By political party, that included 50% of Democrats evaluating the quality of care highly compared with 42% of Republicans. Only 28% of people in
Americans Want More Health Care Issues Baked into the 2024 Elections – Gallup
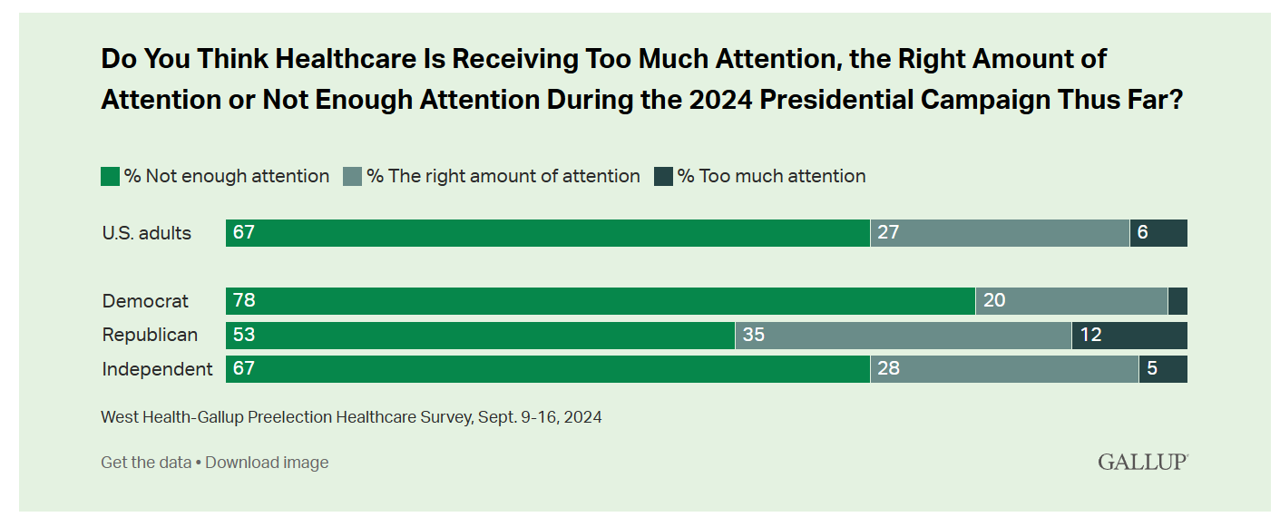
Beyond women’s health and abortion politics, most Americans are looking for more health care baked into the 2024 Elections, based on a new poll from Gallup in collaboration with West Health. Two in three U.S. adults thought health care was not receiving enough attention during the 2024 Presidential campaign as of September 2024. This is a majority shared opinion for voters across the three party IDs in the U.S., shown in the first bar graph. The research polled 3,660 U.S. adults in September, about two-thirds before the presidential debate held September 10, and about one-third
The Cost of Medical Care, Long-Term Care, and Prescription Drugs Top Older Americans’ Health-Related Concerns – With Social Security and Medicare Top of Mind
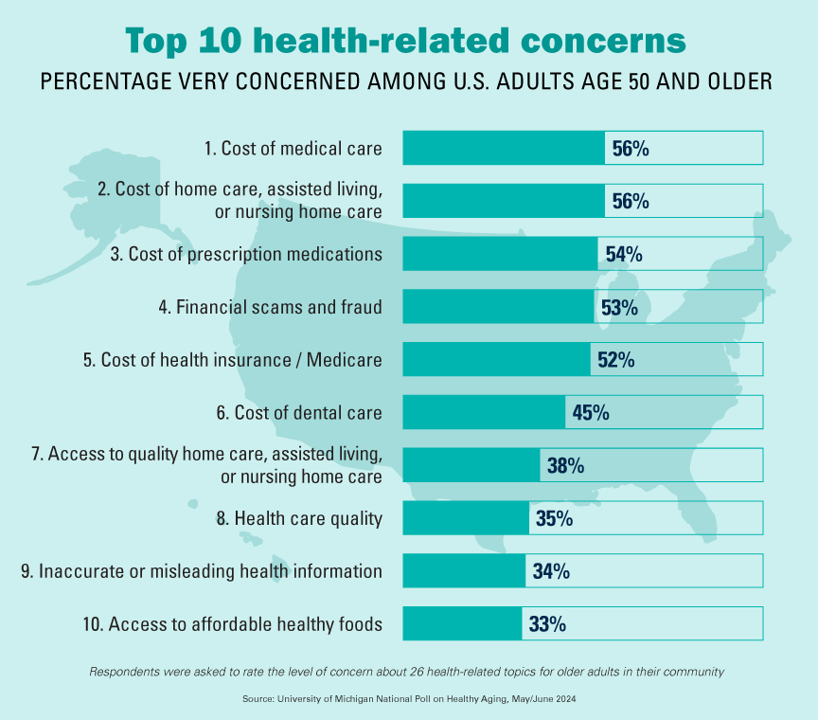
Among Americans 50 years of age and over, the top health-related concerns are Cost, Cost, and Cost — for medical services, for long-term and home care, and for prescription medications. Quality of care ranks lower as a concern versus the financial aspects of health care in America among people 50 years of age and older, as we learn what’s On Their Minds: Older Adults’ Top Health-Related Concerns from the University of Michigan Institute for Healthcare Policy and Innovation. AARP sponsors this study, which is published nearly every month of the year on the Michigan Medicine portal.
More Americans Trust Small Biz and the Military than the Medical System, Gallup Finds
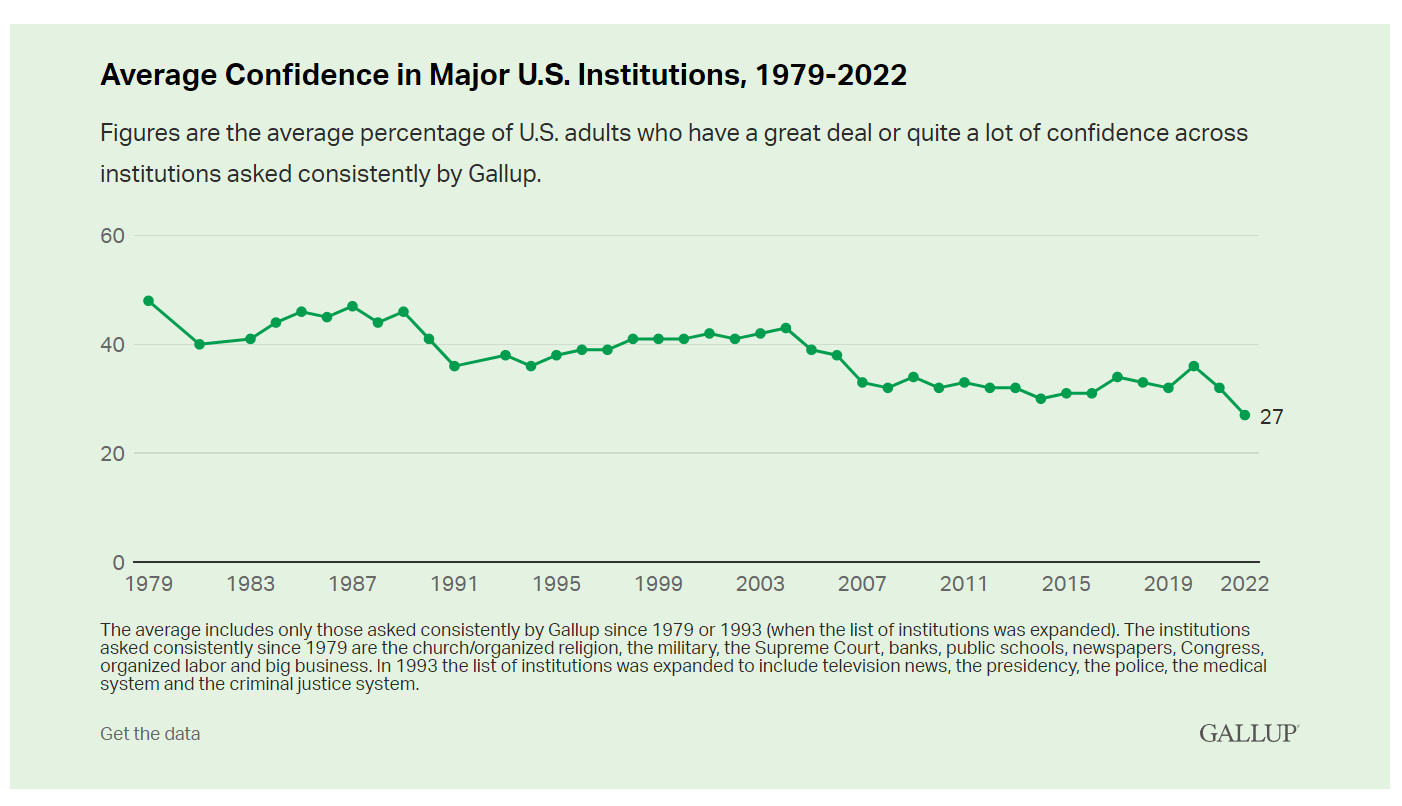
The most trusted institutions in the U.S. are small business and the military, the only two sectors in which a majority of Americans have confidence. Americans’ trust in institutions hit new historic lows in 2022, Gallup found in its latest poll of U.S. sentiment across all major sectors. Today, more Americans have faith in the police than in the medical system, according to a Gallup poll finding that Confidence in U.S. Institutions Down; Average at New Low. published this week of Independence Day 2022. Confidence runs from a higher of 68% for
The 2022 US Health System Report Card: Pretty Terrific If You Live in Hawaii or Massachusetts
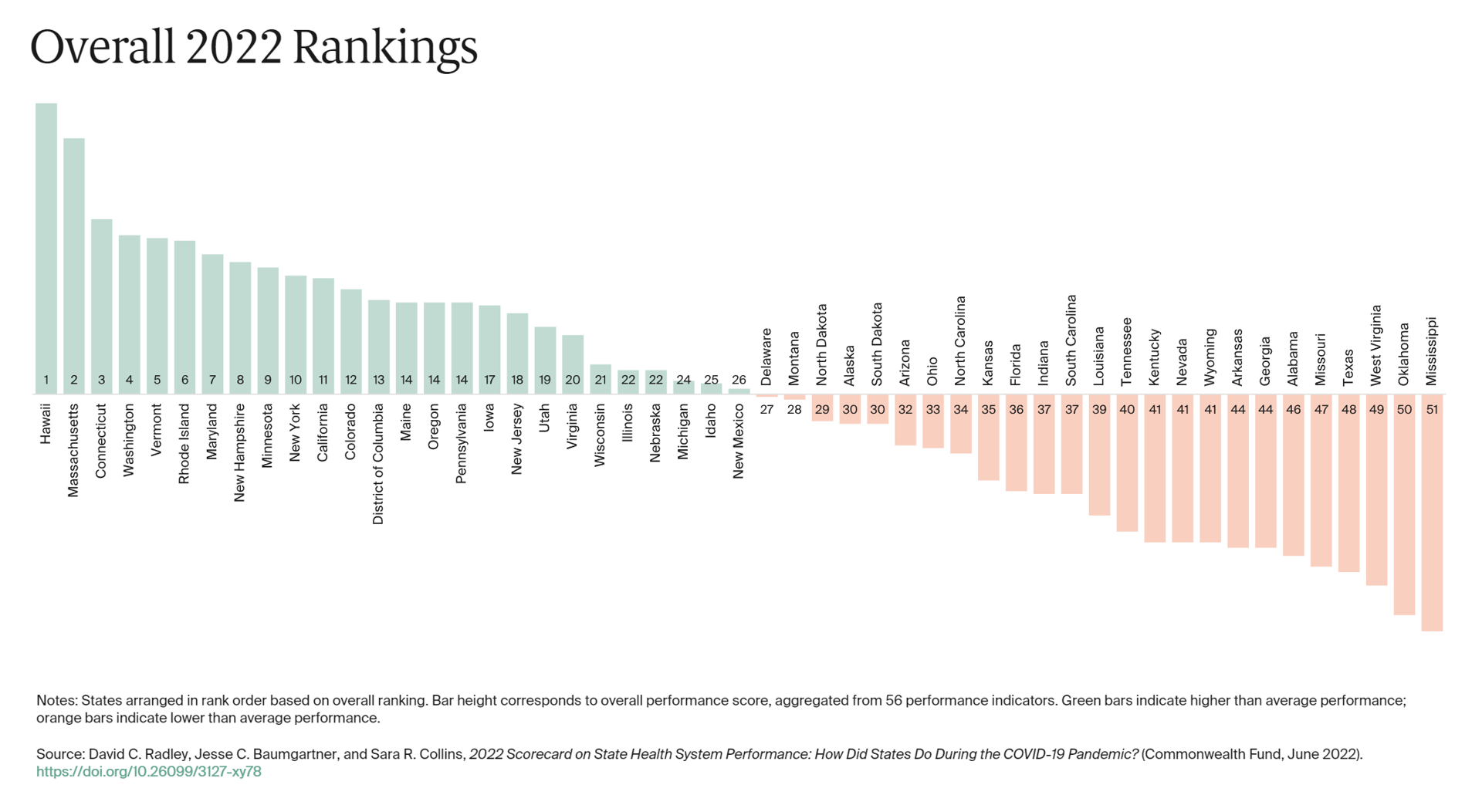
The best U.S. states to live in for health and health care are Hawaii, Massachusetts, Connecticut, Washington, Vermont, Rhode Island, and Maryland… Those are the top health system rankings in the new 2022 Scorecard on State Health System Performance annual report from the Commonwealth Fund. If you live in Mississippi, Oklahoma, West Virginia, Texas, Missouri, Alabama, Georgia, or Arkansas, your health care and outcomes are less likely to be top-notch, the Fund’s research concluded. The Commonwealth Fund has conducted this study since 2006, assessing a range
In the New Inflationary Era, Gas and Health Care Costs Top Household Budget Concerns
Inflation and rising prices are the biggest problem facing America, most people told the Kaiser Family Foundation March 2022 Health Tracking Poll. Underpinning that household budget concern are gas and health care costs. Overall, 55% of people in the U.S. pointed to inflation as the top challenge the nation faces (ranging from 46% of Democrats to 70% of Republicans). Second most challenging problem facing the U.S. was Russia’s invasion into Ukraine, noted by 18% of people — from 14% of Republicans up to 23% of Democrats. The COVID-19 pandemic has fallen far down Americans’ concerns list tied third place with
Primary Care in the U.S. – Still a Weak Backbone for the Health of Health Citizens
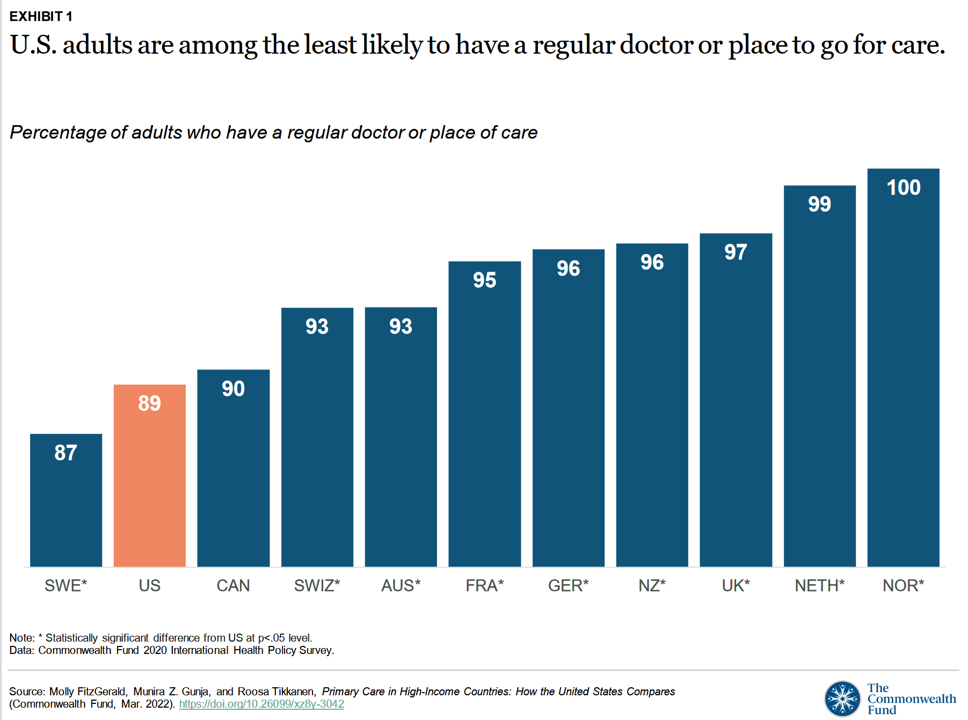
Compared with health citizens living in other wealthy countries, people living in the U.S. are still among the least likely to have a regular doctor or place to go for care. Thus, millions of Americans continue to lack access to primary care compared with peers in other nations, according to a report from The Commonwealth Fund. The Commonwealth Fund has tracked primary care access for many years, and over time has found the United States to lack the kind of primary care “backbone” that many wealthy nations have — whose health citizens also enjoy much better health outcomes that relate
Health Citizens Link Their Views on Democracy, the Economy and the Pandemic
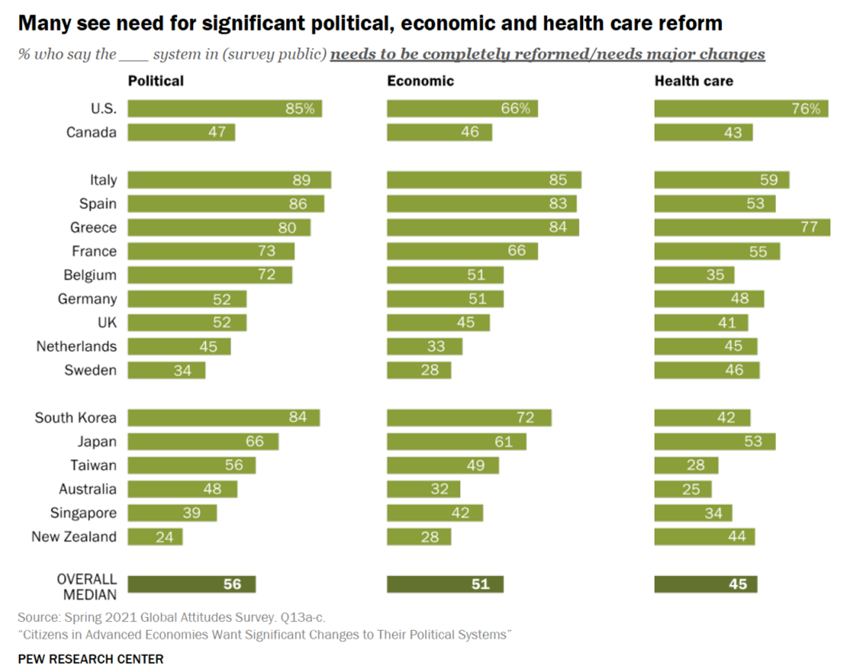
The pandemic has put health care top-of-mind for health citizens the world over. As the public health crisis continues its up-and-downticks around the globe, people are connecting health care to their national economies and politics, based on a global survey from the Pew Research Center, Citizens in Advanced Economies Want Significant Changes to Their Political Systems. For this analysis, the Pew research team assessed the views of some 2,600 health citizens living in 17 developed countries in February 2021. The study report was published in late October 2021. Shown in the first bar chart, the majority of people in at least
And the Oscar Goes To….Power to the Patients!
Health care has increased its role in popular culture over the years. In movies in particular, we’ve seen health care costs and hassles play featured in plotlines in As Good as it Gets [theme: health insurance coverage], M*A*S*H [war and its medical impacts are hell], and Philadelphia [HIV/AIDS in the era of The Band Played On], among dozens of others. And this year’s Oscar winner for leading actor, Anthony Hopkins, played The Father, who with his family is dealing with dementia. [The film, by the way, garnered six nominations and won two]. When I say “Oscar” here on the Health
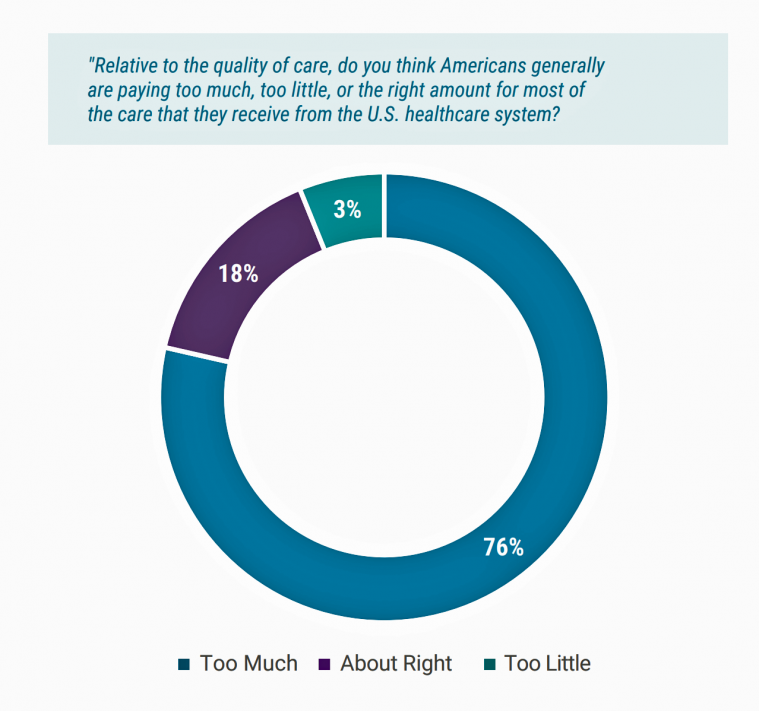
The Cost of Healthcare Can Drive Medical Rationing and Crowd Out Other Household Spending
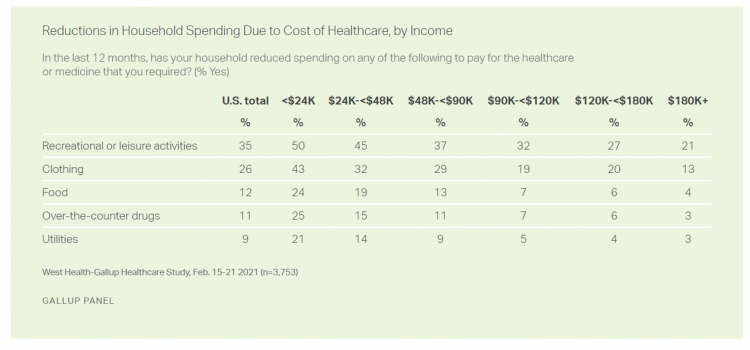
One in five people in the U.S. cannot afford to pay for quality health care — an especially acute challenge for Black and Hispanic Americans, according to a West Health-Gallup poll conducted in March 2021, a year into the COVID-19 pandemic. “The cost of healthcare and its potential ramifications continues to serve as a burdensome part of day-to-day life for millions of Americans,” the study summary observed. Furthermore, “These realities can spill over into other health issues, such as delays in diagnoses of new cancer and associated treatments that are due to forgoing needed care,” the researchers expected. The first table
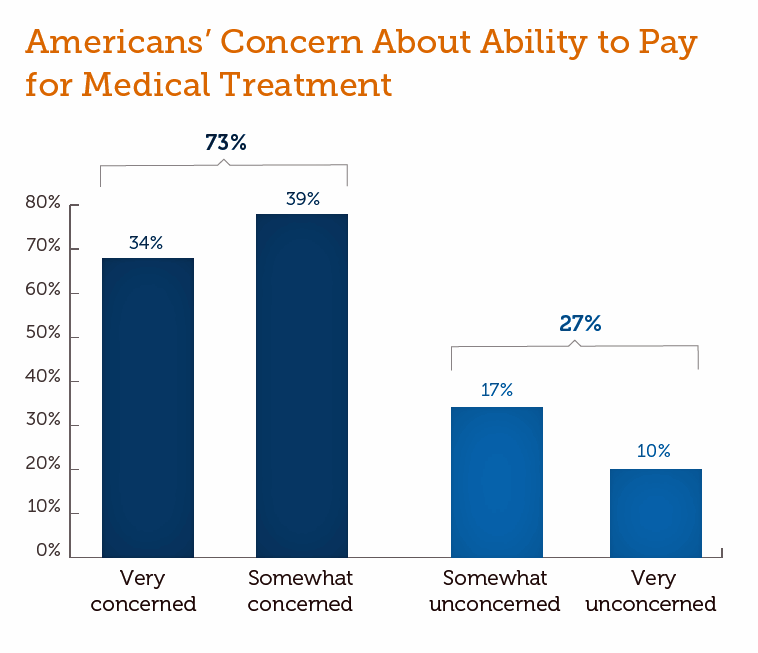
How to Restore Americans’ Confidence in U.S. Health Care: Deal With Access and Cost
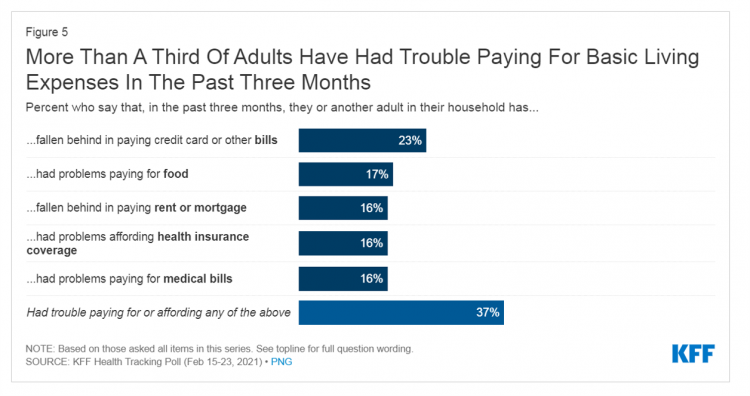
With a vaccine supply proliferating in the U.S. and more health citizens getting their first jabs, there’s growing optimism in America looking to the next-normal by, perhaps, July 4th holiday weekend as President Biden reads the pandemic tea leaves. But that won’t mean Americans will be ready to return to pre-pandemic health care visits to hospital and doctor’s offices. Now that hygiene protocols are well-established in health care providers’ settings, at least two other major consumer barriers to seeking care must be addressed: cost and access. The latest (March 2021) Kaiser Family Foundation Tracking Poll learned that at least one
The Economics of the Pandemic Put Costs at the Top of Americans’ Health Reform Priorities
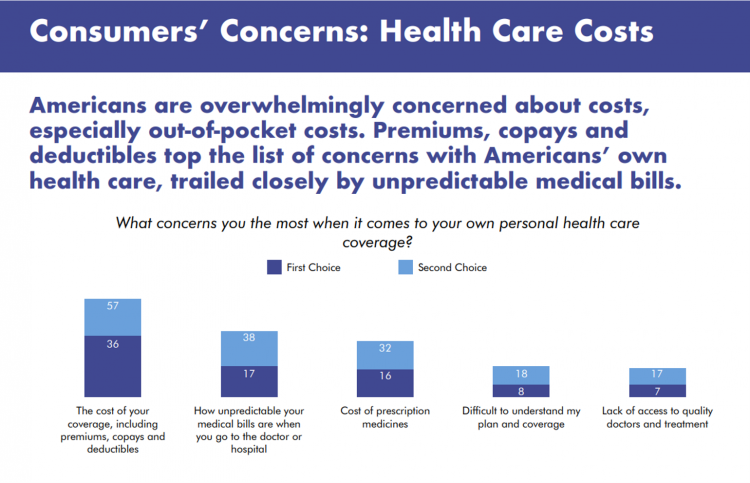
A major side-effect of the coronavirus pandemic in 2020 was its impact on the national U.S. economy, jobs, and peoples’ household finances — in particular, medical spending. In 2021, patients-as-health-consumers seek lower health care and prescription drug costs coupled with higher quality care, discovered by the patient advocacy coalition, Consumers for Quality Care. This broad-spanning patient coalition includes the AIMED Alliance, Autism Speaks, the Black AIDS Institute, Black Women’s Health Initiative, Center Forward, Consumer Action. Fair Foundation, First Focus, Global Liver Institute, Hydrocephalus Association, LULAC, MANA (a Latina advocacy organization), Myositis Association, National Consumers League, National Health IT Collaborative, National Hispanic
The Remarkable Rise of Pharma’s Reputation in the Pandemic
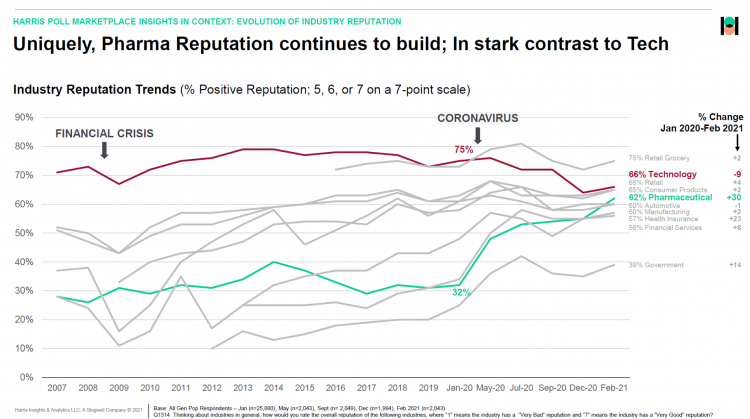
The reputation of the pharmaceutical industry gained a “whopping” 30 points between January 2020 and February 2021, based on the latest Harris Poll in their research into industries’ reputations. The study was written up by Beth Snyder Bulik in FiercePharma. Beth writes that, “a whopping two-thirds of Americans now offer a thumbs-up on pharma” as the title of her article, calling out the 30-point gain from 32% in January 2020 to 62% in February 2021. Thanks to Rob Jekielek, Managing Director of the Harris Poll, for sharing this graph with me for us to understand the details comparing pharma’s to
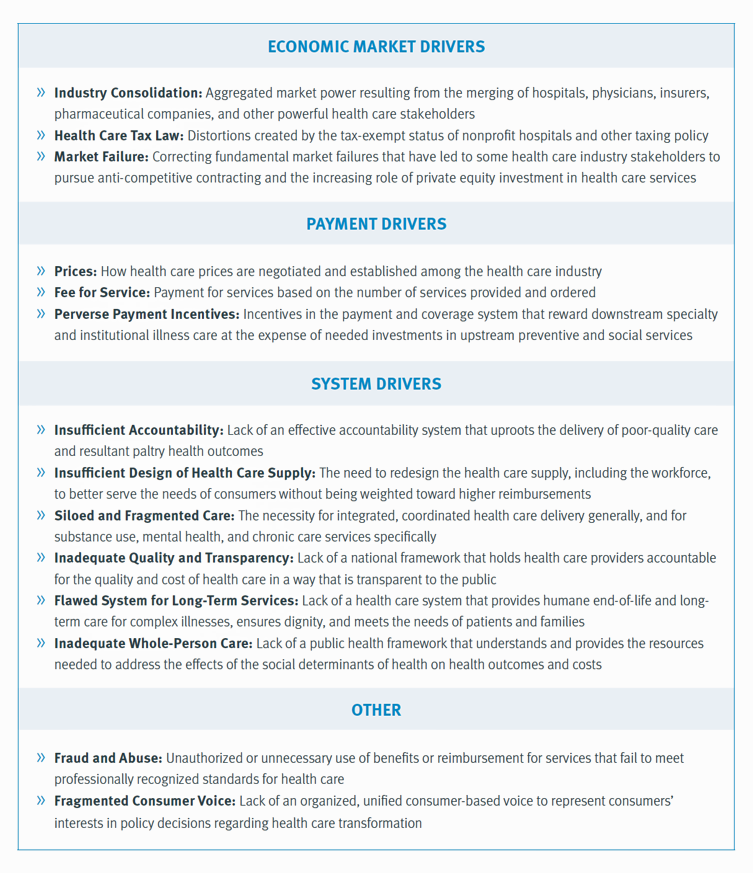
Ten In Ten: Manatt’s Healthcare Priorities to 2031

The coronavirus pandemic has exposed major weaknesses in the U.S. health care system, especially laying bare inequities and inertia in American health care, explained in The Progress We Need: Ten Health Care Imperatives for the Decade Ahead from Manatt Health. The report details the ten objectives that are central to Manatt’s health care practice, a sort of team manifesto call-to-action and North Star for the next decade. Their ten must-do’s for bending the cost curve while driving constructive change for a better health care system are to: Ensure access Achieve health equity Stability the safety net and rebuild public health
Americans A Year Into the Pandemic – A View from Pew
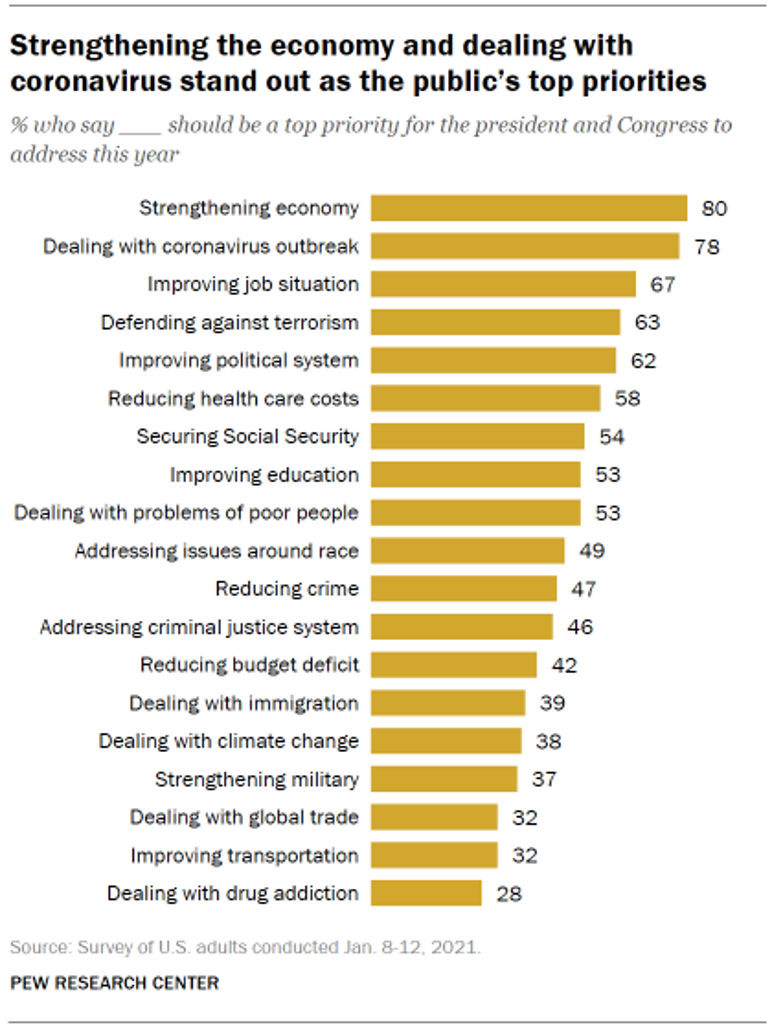
Nearly a year into the COVID-19 pandemic, the same percent of Americans say strengthening the U.S. economy and dealing with the coronavirus outbreak should be a top priority for President Biden and Congress to address this year, according to data from the Pew Research Center collected during the second week of January 2021. Two-thirds of people in the U.S. also want government leaders to prioritize improving the employment situation, defending against terrorism, and improving the political system, the study learned. At Americans’ low end of the priority list for the President and Congress are dealing with global trade, improving transportation,
Can Telemedicine Increase Health Equity? A Conversation with Antoinette Thomas, Dave Ryan, and Me with the ATA

“Yes,” we concurred on our session convened by the American Telemedicine Association (ATA) EDGE session today. “We” was a trio including Antoinette Thomas (@NurseTechExec1), Chief Patient Experience Officer with Microsoft, David Ryan (@DavidPRyan), former long-time Global Head of Intel’s Health/Life Science business; and, me. Antoinette posed three questions for all of us to brainstorm, addressing various aspects of health equity. We covered, The theory that telemedicine should increase health equity — where are we and what are the barriers to getting there? The role of social determinants of health in creating equitable opportunities for health citizens; and, Entering a post-pandemic world,
Food Trends and Hunger in the Pandemic – the Importance of Food Security in Health and Economic Security
In 2020, the COVID-19 pandemic changed all kinds of aspects of our daily lives, not the least of which were our food habits — how we shopped for food, how we bought food, how we cooked and baked from scratch, and how our tastes and nutritional choices changed with our #StayHome and #WorkFromHome lifestyles. People who could keep their jobs and work from home connected by broadband learned how to build up pandemic pantries, shop online, and stay well-fed. But for people in the U.S. who lost employment, had hours cut, or were compelled to stay home to teach kids
The Biden Administration’s Whole-of-Government Approach to Equity – in Health and Beyond
In the U.S., the COVID-19 pandemic has revealed disparities in housing, food, and job security, and the role that one’s ZIP code and social determinants play in health outcomes. Overall, America has done poorly in light of being 4% of the world’s population but having one-fifth of the planet’s deaths due to the coronavirus. But these have disproportionately hit non-white people, who are nearly three times as likely to die from COVID-19 than white Americans. I’ve been head-down reviewing the first two days of President Biden’s signing Executive Orders, reading the National Strategy for COVID-19 Response, and inventorying line items
The 2021 Health Populi TrendCast – Health Care, Self-Care, and the Rebirth of Love in Public Health

In numerology, the symbolic meaning behind the number “21” is death and re-birth. In tarot cards, 21 is a promise of fulfillment, triumph, and victory. How apropos that feels right now as we say goodbye and good riddance to 2020 and turn the page for a kinder, gentler, healthier New Year. It would be sinful to enter a New Year as challenging as 2021 promises to be without taking the many lessons of our 2020 pandemic life and pain into account. For health care in America, it is a time to re-build and re-imagine a better, more equitable landscape for
Voting for Health in 2020

In the 2018 mid-term elections, U.S. voters were driven to polls with health care on their minds. The key issues for health care voters were costs (for care and prescription drugs) and access (read: protecting pre-existing conditions and expanding Medicaid). Issue #2 for 2018 voters was the economy. In 2020, as voting commences in-person tomorrow on 3rd November, U.S. voters have lives and livelihoods on their minds. It’s the pandemic – our physical lives looming largest in the polls – coupled with our fiscal and financial lives. Health is translating across all definitions for U.S. voters in November 2020: for
Stress in America, Like COVID-19, Impacts All Americans
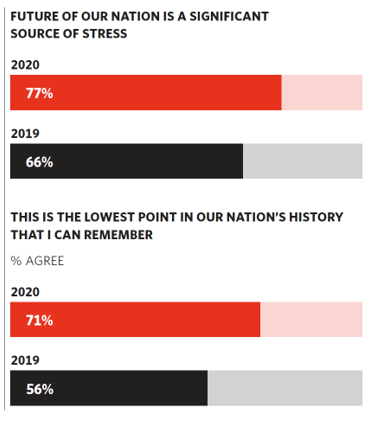
With thirteen days to go until the U.S. #2020Elections day, 3rd November, three in four Americans say the future of America is a significant source of stress, according to the latest Stress in America 2020 study from the American Psychological Association. Furthermore, seven in 10 U.S. adults believe that “now” is the lowest point in the nation’s history that they can remember. “We are facing a national mental health crisis that could yield serious health and social consequences for years to come,” APA introduces their latest read into stressed-out America. Two in three people in the U.S. say that the
Black Health Should Matter More in America: The Undefeated Survey on Race and Health
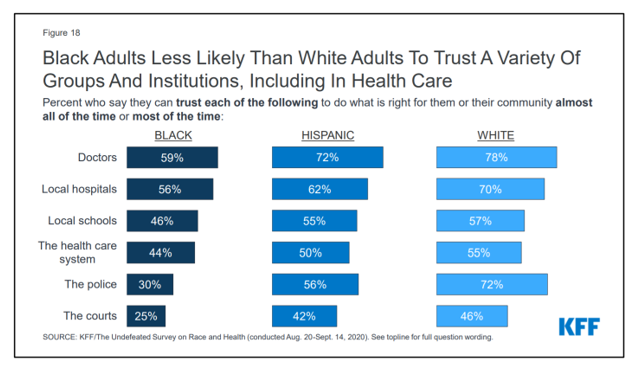
In 2020, most Black people, men and women alike, feel it is a bad time to be Black in America. More than twice as many Black men believed that in 2020 compared with 2006. More than four times as many Black women believed that it’s a bad time to be Black in America in 2020 versus 2011, we learn in The Undefeated Survey on Race and Health from Kaiser Family Foundation (KFF). KFF collaborated with The Undefeated, ESPN’s project that focuses on sports, race, and culture. The Undefeated program was started in May 2016, and has become a thought leader
Two in Three Americans Cite the U.S. Presidential Election is a Significant Source of Stress, Even More than the 2016 Race
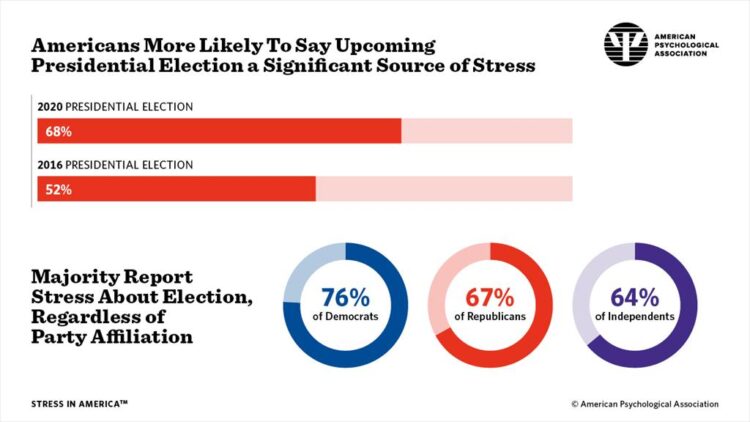
If you perceive you are more stressed in the COVID-19 pandemic than you were in 2019, you are one in many millions feeling so. If you felt stressed during the 2016 Presidential election season, you were also one in a million. Now, as the 2020 Election converges with the coronavirus crisis, even more Americans are feeling significant stress in a double-whammy impact. Our friends at the American Psychological Association have assessed Stress in America for many years of studies. The latest, published 7 October, finds that the 2020 Presidential election is a source of significant stress for more Americans than
Health Citizenship in America. If Not Now, When?
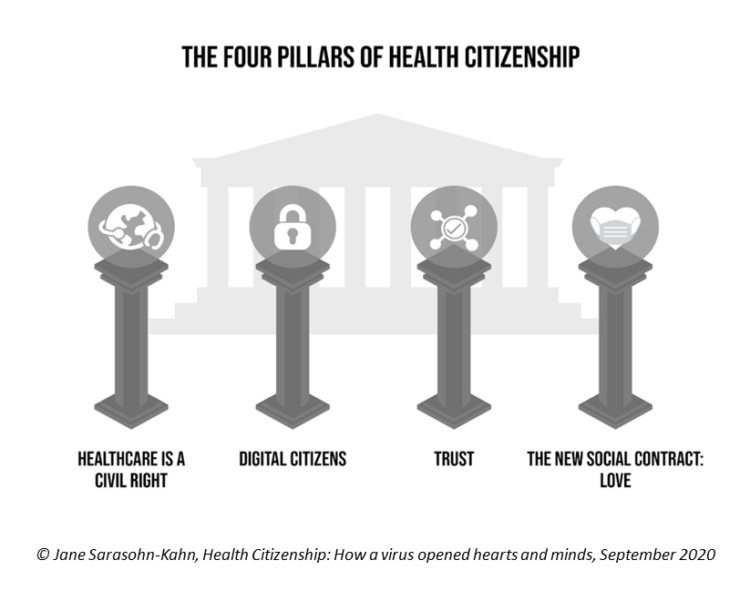
On February 4th, 2020, in a hospital in northern California, the first known inpatient diagnosed with COVID-19 died. On March 11th, the World Health Organization called the growing prevalence of the coronavirus a “pandemic.” On May 25th, George Floyd, a 46-year-old Black man, died at the hands of police in Minneapolis. This summer, the Dixie Chicks dropped the “Dixie” from their name, and NASCAR cancelled the confederate flag from their tracks. Today, nearly 200,000 Americans have died due to the novel coronavirus. My new book, Health Citizenship: How a virus opened hearts and minds, launched this week. In it, I
Only in America: The Loss of Health Insurance as a Toxic Financial Side Effect of the COVID-19 Pandemic

In terms of income, U.S. households entered 2020 in the best financial shape they’d been in years, based on new Census data released earlier this week. However, the U.S. Census Bureau found that the level of health insurance enrollment fell by 1 million people in 2019, with about 30 million Americans not covered by health insurance. In fact, the number of uninsured Americans rose by 2 million people in 2018, and by 1.9 million people in 2017. The coronavirus pandemic has only exacerbated the erosion of the health insured population. What havoc a pandemic can do to minds, bodies, souls, and wallets. By September 2020,
Juneteenth 2020: Inequality and Injustice in Health Care in America
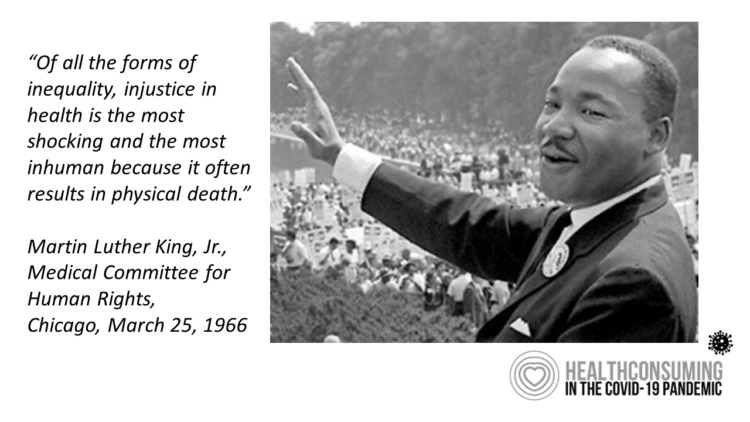
“Of all the forms of inequality, injustice in health is the most shocking and the most inhuman because it often results in physical death,” Martin Luther King, Jr., asserted at the second meeting of the Medical Committee for Human Rights in Chicago on March 25, 1966. This quote has been shortened over the five+ decades since Dr. King told this truth, to the short-hand, “Of all the forms of inequality, injustice in health care is the most shocking and inhumane.” Professor Charlene Galarneau recently enlightened me on Dr. King’s original statement in her seminal essay, “Getting King’s Words Right.” Among
Estimates of COVID-19 Medical Costs in the US: $20K for inpatient stay, $1300 OOP costs
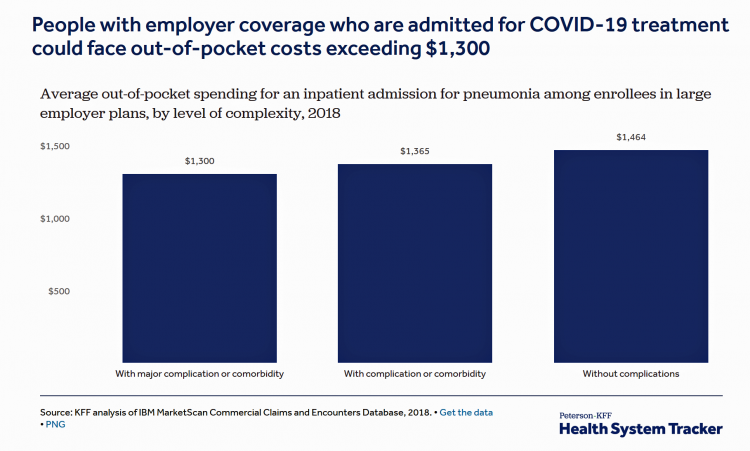
In the midst of growing inpatient admissions and test results for COVID-19, Congress is working as I write this post to finalize a round of legislation to help Americans with the costs-of-living and (hopefully) health care in a national, mandated, clarifying way. Right now in the real world, real patients are already being treated for COVID-19 in American hospitals. Patients are facing health care costs that may result in multi-thousand dollar bills at discharge (or death) that will decimate households’ financial health, particularly among people who don’t have health insurance coverage, covered by skinny or under-benefited plans, and/or lack banked
The High Cost-of-Thriving and the Evolving Social Contract for Health Care
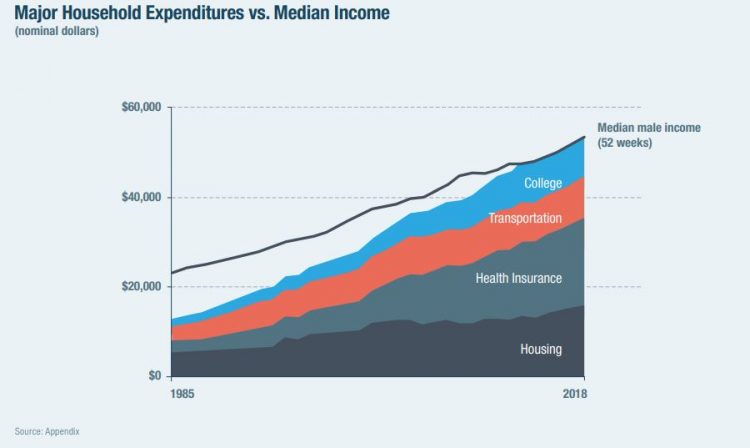
Millions of Americans have to work 53 weeks to cover a year’s worth of household expenses. Most Americans haven’t saved much for their retirement. Furthermore, the bullish macroeconomic outlook for the U.S. in early 2020 hasn’t translated into individual American’s optimism for their own family budgets. (Sidebar and caveat: yesterday was the fourth day in a row of the U.S. financial markets losing as much as 10% of market cap, so the global economic outlook is being revised downward by the likes of Goldman Sachs, Vanguard, and Morningstar, among other financial market prognosticators. MarketWatch called this week the worst market
Americans’ Top 2 Priorities for President Trump and Congress Are To Lower Health Care and Rx Costs
Health care pocketbook issues rank first and second place for Americans in these months leading up to the 2020 Presidential election, according to research from POLITICO and the Harvard Chan School of Public Health published on 19th February 2020. This poll underscores that whether Democrat or Republican, these are the top two domestic priorities among Americans above all other issues polled including immigration, trade agreements, infrastructure and regulations. The point that Robert Blendon, Harvard’s long-time health care pollster, notes is that, “Even among Democrats, the top issues…(are) not the big system reform debates…They’re worried about their own lives, their own
Most Workers and their Employers Want to Receive Digital Healthcare On-Demand
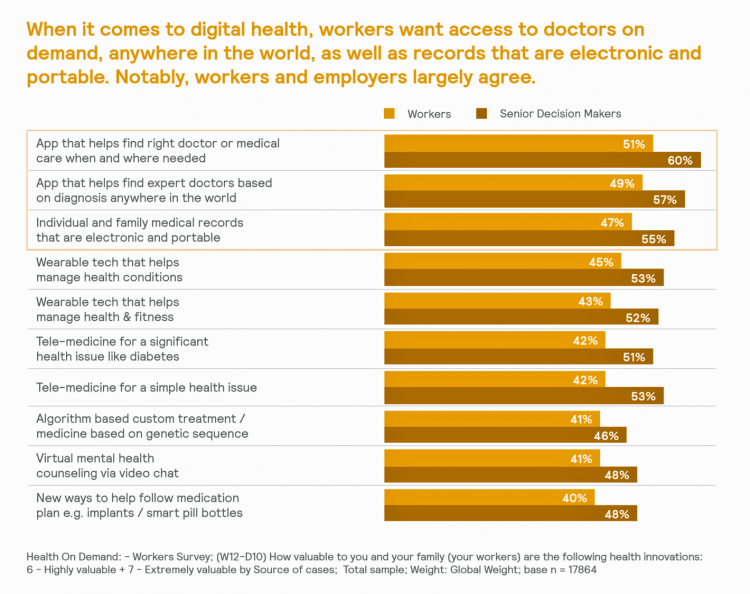
Most employers and their workers see the benefits of digital health in helping make health care more accessible and lower-cost, according to survey research published in Health on Demand from Mercer Marsh Benefits. Interestingly, more workers living in developing countries are keener on going digital for health than people working in wealthier nations. Mercer’s study was global, analyzing companies and their employees in both mature and growth economies around the world. In total, Mercer interviewed 16,564 workers and 1,300 senior decision makers in companies. The U.S. sample size was 2,051 employees and 100 decision makers. There’s a treasure trove of insights
The Federal Reserve Chairman Speaks Out on Health Care Costs: “Spending But Getting Nothing”
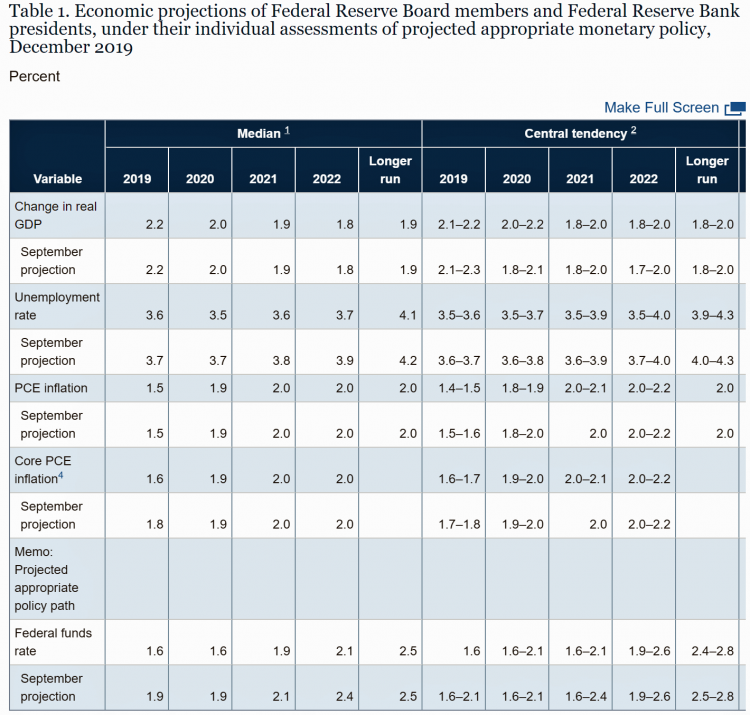
On February 12, 2020, the Chairman of the Federal Reserve Bank of the U.S. submitted the Semiannual Monetary Policy Report to Congress and testified to the Senate Banking Committee. Chairman Jerome Powell detailed the current state of the economy, discussing the state of the macroeconomy, GDP growth, unemployment, inflation, and projections for 2022 and beyond. The top line data points are shown in the first chart. After his prepared remarks, Chairman Powell responded to questions from members of the Senate Banking Committee. Senator Ben Sasse (R-Neb.) asked him about health care costs’ impact on the national U.S. economy. The Chairman
Come Together – A Health Policy Prescription from the Bipartisan Policy Center
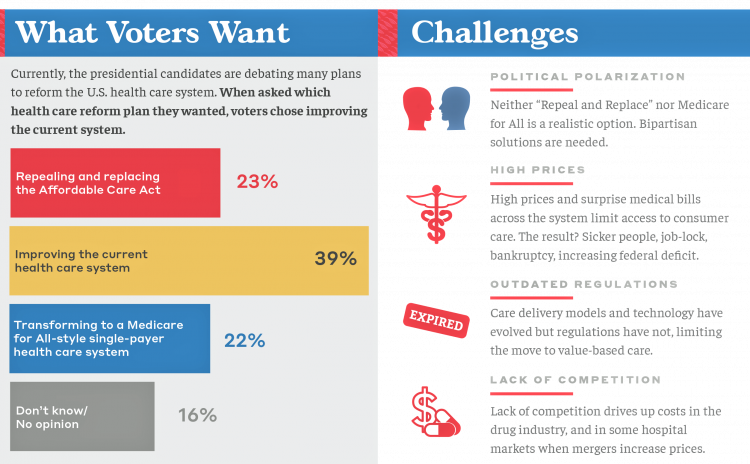
Among all Americans, the most popular approach for improving the health care in the U.S. isn’t repealing or replacing the Affordable Care Act or moving to a Medicare-for-All government-provided plan. It would be to improve the current health care system, according to the Bipartisan Policy Center’s research reported in a Bipartisan Rx for America’s Health Care. The BPC is a truly bipartisan organization, co-founded by Former Democratic Senate Majority Leaders Tom Daschle and George Mitchell, and Former Republican Senate Majority Leaders Howard Baker and Bob Dole. While this political week in America has revealed deep chasms between the Dems and
What’s Causing Fewer Primary Care Visits in the US?
Americans who have commercial health insurance (say, through an employer or union) are rarely thought to face barriers to receiving health care — in particular, primary care, that front line provider and on-ramp to the health care system. But in a new study published in the Annals of Internal Medicine, commercially-insured adults were found to have visited primary care providers (PCPs) less often, and 1 in 2 had no PCP visits in one year. In Declining Use of Primary Care Among Commercially Insured Adults in the United States, 2008-2016, the researchers analyzed data from a national sample of adult health
A Uniting Issue in the United States is Lowering Prescription Drug Costs
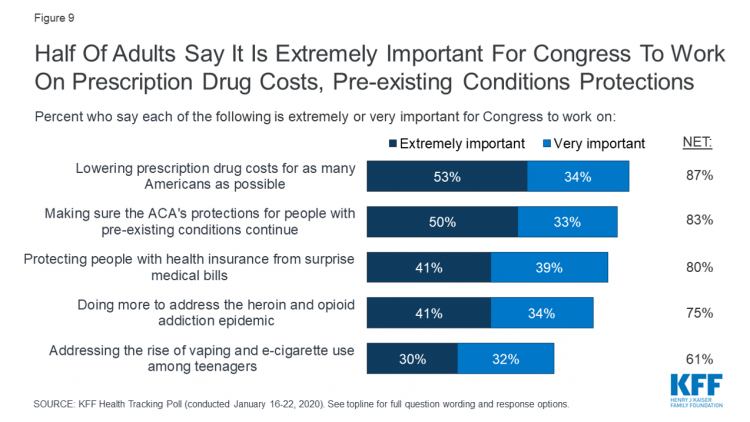
Health care continues to be the top-ranked voting issue in the U.S. looking to the November 2020 Presidential and Congressional elections. The Kaiser Family Foundation conducts the monthly poll which gauges U.S. adults’ perspectives on health care, and this month’s January 2020 Kaiser Health Tracking Poll explores Americans’ views on broad healthcare reform plans and specific medical policy issues. Overall, Americans point to prescription drug costs and the preservation of the Affordable Care Act’s protections for people with pre-existing conditions, the first chart tells us. Third and fourth on voters’ minds are protecting patients from surprise medical bills and better
In 2020, PwC Expects Consumers to Grow DIY Healthcare Muscles As Medical Prices Increase

The new year will see a “looming tsunami” of high prices in healthcare, regulation trumping health reform, more business deals reshaping the health/care industry landscape, and patients growing do-it-yourself care muscles, according to Top health industry issues of 2020: Will digital start to show an ROI from the PwC Health Research Institute. I’ve looked forward to reviewing this annual report for the past few years, and always learn something new from PwC’s team of researchers who reach out to experts spanning the industry. In this 14th year of the publication, PwC polled executives from payers, providers, and pharma/life science organizations. Internally,
A Tale of Two Americas as Told by the 2019 OECD Report on Health

It was the best of times, It was the worst of times, It was the age of wisdom, it was the age of foolishness, It was the epoch of belief, it was the epoch of incredulity, … starts Dickens’ Tale of Two Cities. That’s what came to my mind when reading the latest global health report from the OECD, Health at a Glance 2019, which compares the United States to other nations’ health care outcomes, risk factors, access metrics, and spending. Some trends are consistent across the wealthiest countries of the world, many sobering, such as: Life expectancy rates fell in 19 of the
Great Expectations for Health Care: Patients Look for Consumer Experience and Trust in Salesforce’s Latest Research

On the demand side of U.S. health care economics, patients are now payors as health consumers with more financial skin in paying medical bills. As consumers, people have great expectations from the organizations on the supply side of health care — providers (hospitals and doctors), health insurance plans, pharma and medical device companies. But as payors, health consumers face challenges in getting care, so great expectations are met with frustration and eroding trust with the system, according to the latest Connected Healthcare Consumer report from Salesforce published today as the company announced expansion of their health cloud capabilities. This is
While Costs Are A Top Concern Among Most U.S. Patients, So Are Challenges of Poverty, Food, and Housing
Rising health care costs continue to concern most Americans, with one in two people believing they’re one sickness away from getting into financial trouble, according to the 2019 Survey of America’s Patients conducted for The Physicians Foundation. In addition to paying for “my” medical bills, most people in the U.S. also say that income inequality and inadequate social services significantly contribute to high medical spending for every health citizen in the nation. The Physicians Foundation conducts this study into Americans’ views on the U.S. health care system every other year. This year’s poll was conducted in September 2019 and included input
“It’s the Deductible, Stupid” – Health Premiums Reach $20,576 in 2019 for a Family
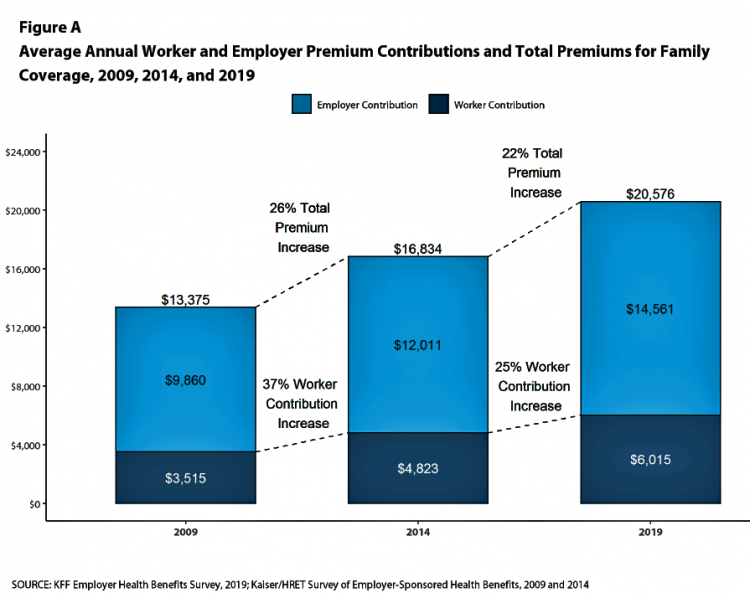
Here’s the latest arithmetic on American workers’ financial trade-off of wages for health care insurance coverage: in the ten years since 2009, family premiums have risen 54% and workers’ contribution to health care spending grew 71%. Wages? They rose 26%, and general price inflation by 20%, according to the Kaiser Family Foundation survey on employer-sponsored benefits for 2019 released yesterday. Survey details for this 21st annual encyclopedia on employer-sponsored health care are published in Health Affairs October 2019 issue in a paper titled, Health Benefits in 2019: Premiums Inch Higher, Employers Respond to Federal Policy. Because this
Most U.S. Voters Support Building on the ACA, Not Medicare For All, As Fewer Americans Have Insurance Coverage
The vast majority of Americans favor lowering the cost of prescriptions, keeping the Affordable Care Act’s provisions to cover pre-existing conditions, lower overall medical costs, and protect people from surprise medical bills, according to the KFF Health Tracking Poll – September 2019: Health Care Policy In Congress And On The Campaign Trail. The big headline in this poll following last night’s third Democratic Presidential debate is that 55% of Democrats and Democrat-leaning Independent voters prefer a candidate that will build on the Affordable Care Act (ACA) versus a President that would replace the ACA with a Medicare For All plan (M4A).
Growing Support for Medicare for All – But Do People Really Understand What It Means?
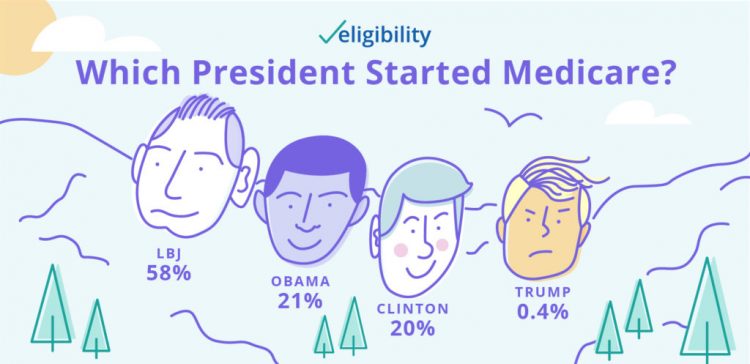
Two new data points converge that beg the question in the title of this post. These two surveys are: The Morning Consult’s poll published today finding growing support among Democratic voters for Medicare for All as the centerpiece for health reform in America; and, A recent study from Eligibility.com on “Medicare Myths Explained,” with the tagline, “How much do you know about Medicare?” Not so very much, Eligibility.com found out. Let’s start with the Morning Consult poll results, which compare support for Medicare for All from January 2019 and August 2019. The headline number from this poll is seen in
Talking “HealthConsuming” on the MM&M Podcast

Marc Iskowitz, Executive Editor of MM&M, warmly welcomed me to the Haymarket Media soundproof studio in New York City yesterday. We’d been trying to schedule meeting up to do a live podcast since February, and we finally got our mutual acts together on 6th August 2019. Here’s a link to the 30-minute conversation, where Marc combed through the over 500 endnotes from HealthConsuming‘s appendix to explore the patient as the new health care payor, the Amazon prime-ing of people, and prospects for social determinants of health to bolster medicines “beyond the pill.” https://www.pscp.tv/MMMnews/1eaJbvgovBYJX Thanks for listening — and if you
100 Million People in America Lack Broadband — an On-Ramp to Health and Safety

One in three Americans does not have a broadband connection, according to a new report from the NPD Group. This means that about 100 million people in the U.S. can’t benefit from telehealth and other digital health connections that can bolster self-care, home care, and lower cost care. Most of these folks in the broadband-digital divide live in rural America/ “The so-called digital divide, between those that can or cannot make the best use of the Internet, can be clearly felt in rural markets where the lack of broadband impacts everything from entertainment to the educational system,” Eddie Hold, President
Gaps in Health Equity in America Are Growing

There’s been a “clear lack of progress on health equity during the past 25 years in the United States,” asserts a data-rich analysis of trends conducted by two professors/researchers from UCLA’s School of Public Health. The study was published this week in JAMA Network Open. The research mashed up several measures of health equity covering the 25 years from 1993 through 2017. The data came out of the Centers for Disease Control and Prevention’s Behavioral Risk Factor Surveillance System looking at trends by race/ethnicity, sex and income across three categories for U.S. adults between 18 and 64 years of age.
Health Care and the Democratic Debates – Round 2 – Battle Royale for M4All vs Medicare for All Who Want It – What It Means for Industry

Looking at this photo of the 2020 Democratic Party Presidential candidate debater line-up might give you a déjà vu feeling, a repeat of the night-before debate. But this was Round 2 of the debate, with ten more White House aspirants sharing views — sometimes sparring — on issues of immigration, economic justice, climate change, and once again health care playing a starring role from the start of the two-hour event. The line-up from left to write included: Marianne Williamson. author and spiritual advisor John Hickenlooper, former Governor of Colorado Andrew Yang. tech company executive Pete Buttigieg, Mayor of South Bend,
Health Care and the Democratic Debates – Part 1 – Medicare For All, Rx Prices, Guns and Mental Health

Twenty Democratic Presidential candidates each have a handful of minutes to make their case for scoring the 2020 nomination, “debating” last night and tonight on major issues facing the United States. I watched every minute, iPad at the ready, taking detailed notes during the 120 minutes of political discourse conducted at breakneck speed. Lester Holt, Savannah Guthrie, and Jose Diaz-Balart asked the ten candidates questions covering guns, butter (the economy), immigration, climate change, and of course, health care — what I’m focusing on in this post, the first of two-debate-days-in-a-row. The first ten of twenty candidates in this debate were,
Healthcare Costs Inspire Employer Activism and Employee Dissatisfaction – What PwC Found Behind the Numbers
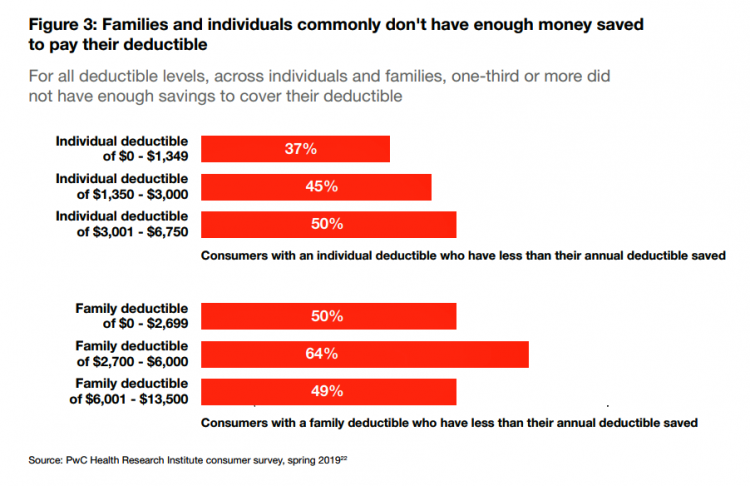
In the U.S. each year between 2006 and 2016, employees’ healthcare cost sharing grew 4.5%. In that decade, Americans’ median wages rose 1.8% a year, PwC notes in their annual report, Medical cost trend: Behind the numbers 2020 from the firm’s Health Research Institute. Medical cost trend is the projected percent growth in healthcare costs over a year based on an equivalent benefit package from one year to the next. As the first chart shows, trend will grow 6% from 2019 to 2020. This is an increase of 0.3 percentage points up from 5.7% for 2019, which was flat from
Americans Could Foster a Health Consumer Movement, Families USA Envisions
Employers, health care providers, unions, leaders and — first and foremost, consumers — must come together to build a more accessible, affordable health care system in America, proposes a call-to-action fostered by a Families USA coalition called Consumers First: The Alliance to Make the Health Care System Work for Everyone. The diverse partners in this Alliance include the American Academy of Family Physicians, AFSCME (the largest public service employees’ union in the U.S.), the American Benefits Council (which represents employers), the American Federation of Teachers (AFT), First Focus (a bipartisan children’s advocacy organization), and the Pacific Business Group on Health
People Want to Flourish, Not Just Live – Speaking Health Politics to Real People
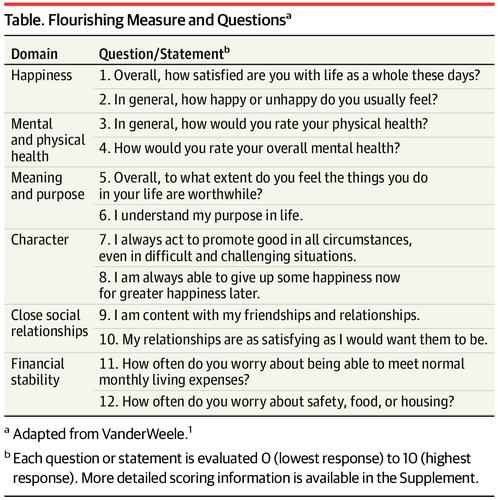
“How should we define ‘health?'” a 2011 BMJ article asked. The context for the question was that the 1948 World Health Organization definition of health — that health is, “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”– was not so useful in the 21st century. The authors, a global, multidisciplinary team from Europe, Canada and the U.S., asserted that by 2011, human health was marked less by infectious disease and more by non-communicable conditions that could be highly influenced, reversed and prevented through self-care by the individual and public health policy
How Consumers’ Belt-Tightening Could Impact Health/Care – Insights from Deloitte’s Retail Team

Over the ten years between 2007 and 2017, U.S. consumer spending for education, food and health care substantially grew, crowding out spending for other categories like transportation and housing. Furthermore, income disparity between wealthy Americans and people earning lower-incomes dramatically widened: between 2007-2017, income for high-income earners grew 1,305 percent more than lower-incomes. These two statistics set the kitchen table for spending in and beyond 2019, particularly for younger people living in America, considered in Deloitte’s report, The consumer is changing, but perhaps not how you think. The authors are part of Deloitte Consulting’s Retail team. The retail spending data
How Consumers Look At Social Determinants of Health for Cancer, Diabetes and Mental Health

Enlightened health/care industry and public policy stakeholders have begun to embrace and address social determinants of health. These are the inputs that bolster health beyond health care services: they include economic stability like job security and income level (and equity), education, and access to healthy food, food security, safe neighborhoods, social support, clean environments (water and air), and in my own update on SDoH factors, access to broadband connectivity. As physician leaders in the AMA, technology advocates from AMIA, and numerous health plans focus efforts on strengthening social determinants, what do people – consumers, patients, caregivers — think about these
Two-Thirds of Americans Say Healthcare Doesn’t Work Well, in RealClear Politics Poll

Health care is the top issue facing the U.S. today, one in three Americans says, with another one-fourth pointing to the economy. Together, health care + the economy rank the top issues for 62% of Americans. Health care and the economy are, in fact, intimately tied in every American’s personal household economy I assert in my book, HealthConsuming: From Health Consumer to Health Citizen. This poll from RealClear Politics, conducted in late April/early May 2019, makes my point that the patient is the consumer and, facing deductibles and more financial exposure to footing the medical bill, the payor. Fully
Assessing the GAO’s Report on Single-Payer Healthcare in America: Let’s Re-Imagine Workflow

Calls for universal health care, some under the banner of Medicare for All,” are growing among some policy makers and presidential candidates looking to run in 2020. As a response, the Chairman of the House Budget Committee in the U.S. Congress, Rep. John Yarmuth (D-Ky.), asked the Congressional Budget Office (CBO) to develop a report outlining definitions and concepts for a single-payer health care system in the U.S. The result of this ask is the report, Key Design Components and Considerations for Establishing a Single-Payer Health Care System, published on 1st May by the CBO. The report provides
Will Health Consumers Morph Into Health Citizens? HealthConsuming Explains, Part 5

The last chapter (8) of HealthConsuming considers whether Americans can become “health citizens.” “Citizens” in this sense goes back to the Ancient Greeks: I return to Hippocrates, whose name is, of course, the root of The Hippocratic Oath that physicians take. Greece was the birthplace of Democracy with a capital “D.” Hippocrates’ book The Corpus is thought to be one of the first medical textbooks. The text covered social, physical, and nutritional influences, and the concept of “place” for health and well-being. Here, the discussion detailed the roles of air and water for health. The Hippocratic texts also coached doctors to
What We Know We Know About ZIP Codes, Food, and Deaths of Despair – HealthConsuming Explains, Part 3

“There’s a 15-year difference in the life expectancy between the richest and poorest Americans.” That’s the first sentence of Chapter 7 in my book, HealthConsuming: From Health Consumer to Health Citizen. This data point comes from research published in JAMA in April 2016 on the association between income and life expectancy in the U.S. (That’s endnote #399 in the back of the book, one of 519 notes I use to support the plotline). Today, the Brookings Institution convened a meeting on the funding for social determinants of health to address disparities, costs, and quality of healthcare in America. The overall
Medical Costs Are Consuming Americans’ Financial Health
Spending on medical care costs crowded out other household spending for millions of Americans in 2018, based on The U.S. Healthcare Cost Crisis, a survey from West Health and Gallup. Gallup polled 3,537 U.S. adults 18 and over in January and February 2019. One in three Americans overall are concerned they won’t be able to pay for health care services or prescription drugs: that includes 35% of people who are insured, and 63% of those who do not have insurance. Americans borrowed $88 billion in 2018 to pay for health care spending, West Health and Gallup estimated. 27 million Americans
In the U.S., Patients Consider Costs and Insurance Essential to Their Overall Health Experience
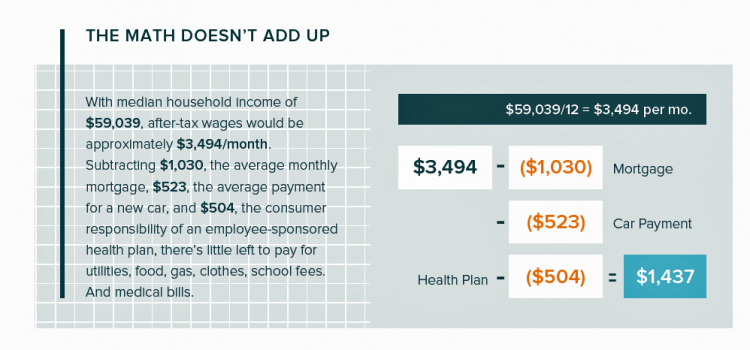
Patients in the U.S. assume the role of payor when they are enrolled in high-deductible health plans. People are also the payor when dealing with paying greater co-payments for prescription drugs, especially as new therapeutic innovations come out of pipelines into commercial markets bearing six-digit prices for oncology and other categories. For mainstream Americans, “the math doesn’t add up” for paying medical bills out of median household budgets, based on the calculations in the 2019 VisitPay Report. Given a $60K median U.S. income and average monthly mortgage and auto payments, there’s not much consumer margin to cover food, utilities, petrol,
Having Health Insurance Is A Social Determinant of Health
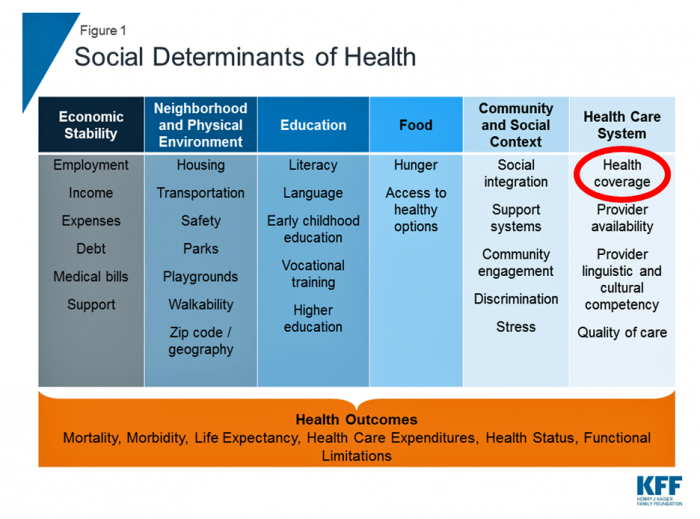
Health insurance was on the collective minds of American voters in the 2018 midterm elections. Health care, broadly defined, drove many people to the polls voting with feet and ballots to protect their access to a health plan covering a pre-existing condition or to protest the cost of expensive prescription drugs. These were the two top health care issues among voters in late 2018, a Kaiser Family Foundation poll at the time assessed. Yesterday, President Trump verbally re-branded the Republican Party as “the party of healthcare.” That Presidential pronouncement was tied to a letter written on U.S. Department of Justice
Patients, Health Consumers, People, Citizens: Who Are We In America?

“Patients as Consumers” is the theme of the Health Affairs issue for March 2019. Research published in this trustworthy health policy publication covers a wide range of perspectives, including the promise of patients’ engagement with data to drive health outcomes, citizen science and participatory research where patients crowdsource cures, the results of financial incentives in value-based plans to drive health care “shopping” and decision making, and ultimately, whether the concept of patients-as-consumers is useful or even appropriate. Health care consumerism is a central focus in my work, and so it’s no surprise that I’ve consumed every bit of this publication. [In
National Health Spending Will Reach Nearly 20% of U.S. GDP By 2027
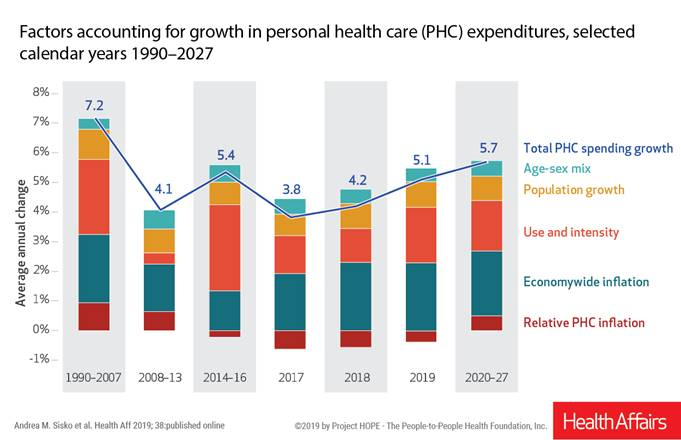
National health spending in the U.S. is expected to grow by 5.7% every year from 2020 to 2027, the actuaries at the Centers for Medicare and Medicaid Services forecast in their report, National Health Expenditure Projections, 2018-2927: Economic And Demographic Trends Drive Spending And Enrollment Growth, published yesterday by Health Affairs. For context, note that general price inflation in the U.S. was 1.6% for the 12 months ending January 2019 according to the U.S. Bureau of Labor Statistics. This growth rate for health care costs exceeds every period measured since the high of 7.2% recorded in 1990-2007. The bar chart illustrates the
In U.S. Health Care, It’s Still the Prices, Stupid – But Transparency and Consumer Behavior Aren’t Working As Planned
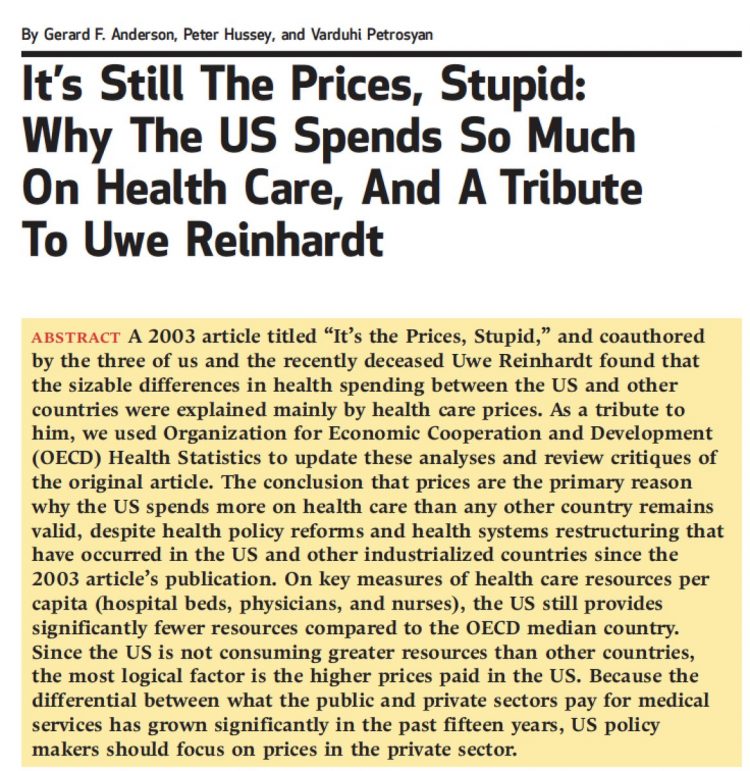
I’m glad to be getting back to health economic issues after spending the last couple of weeks firmly focused on consumers, digital health technologies and CES 2019. There’s a lot for me to address concerning health care costs based on news and research published over the past couple of weeks. We’ll start with the centerpiece that will provide the overall context for this post: that’s the ongoing research of Gerard Anderson and colleagues under the title, It’s Still The Prices, Stupid: Why The US Spends So Much On Health Care, And A Tribute To Uwe Reinhardt. It is bittersweet to
Costs, Consumerism, Cyber and Care, Everywhere – The 2019 Health Populi TrendCast

Today is Boxing Day and St. Stephens Day for people who celebrate Christmas, so I share this post as a holiday gift with well-wishes for you and those you love. The tea leaves have been brewing here at THINK-Health as we prepared our 2019 forecast at the convergence of consumers, health, and technology. Here’s our trend-weaving of 4 C’s for 2019: costs, consumerism, cyber and care, everywhere… Health care costs will continue to be a mainstream pocketbook issue for patients and caregivers, with consequences for payors, suppliers and ultimately, policymakers. Legislators inside the DC Beltway will be challenged by the
Rationing Care in America: Cost Implications Getting to Universal Health Coverage

It would not be surprising to know that when the Great Recession hit the U.S. in 2008, one in three Americans delayed medical treatment due to costs. Ten years later, as media headlines and the President boast an improved American economy, the same proportion of people are self-rationing healthcare due to cost. That percentage of people who delay medical cost based on the expense has remained stable since 2006: between 29 and 31 percent of Americans have self-rationed care due to cost for over a decade. And, 19% of U.S. adults, roughly one-in-five people who are sick and dealing with
Most Americans Want the Federal Government to Ensure Healthcare for All

Most people in the U.S. believe that the Federal government should ensure that their fellow Americans, a new Gallup Poll found. This sentiment has been relatively stable since 2000 except for two big outlying years: a spike of 69% in 2006, and a low-point in 2003 of 42%. In 2006, Medicare Part D launched, which may have boosted consumers’ faith in Federal healthcare programs. In contrast, in 2013 the Affordable Care Act was in implementation and consumer-adoption mode, accompanied by aggressive anti-“Obamacare” campaigns in mass media. That’s the top lighter green line in the first chart. But while there’s majority support
Vote As If Your Health Depended Upon It; Learning from Governor Kasich on Voting Day 2018

…because it does. “Citizens scare politicians,” I heard Governor John Kasich say to Nicole Wallace on her show Deadline: White House yesterday, just hours from today’s U.S. 2018 midterm elections. Governor Kasich has led the Buckeye State since 2011, and his second and final term ends in January 2019. The Governor expanded Medicaid under the Affordable Care Act in the State of Ohio, discussed in this insightful Washington Post article. “I am my brothers’ and sisters’ keeper,” Kasich told Wallace. The Governor asserted this in the context of the role of protecting his fellow citizens for health and well-being, for
Healthcare and the F-Word: Health Politics Rank High on November 6, 2018

“Let’s get this thing f-ing done,” Martha McSally passionately asserted on May 4, 2017. Paul Ryan said, on the floor of the U.S. House of Representatives without cursing, “A lot of us have waited seven years to cast this vote.” McSally, who represents Tucson, Arizona, in the U.S. Congress, is running to replace retiring Senator Jeff Flake. McSally was one of the 217 Republicans in the House who voted to repeal the Affordable Care Act, subsequently celebrating a victory in the Rose Garden of the White House with jubilant peers. The final vote was 217-213. Here’s the final roll call
Healthcare Costs Stress Out U.S. Voters One Week Ahead of 2018 Mid-Term Elections

With seven days until voters go to the polls for what some call the most momentous U.S. election in decades, most Americans say that healthcare costs are a major stress, second only to money. So warns the Sixth Annual Nationwide TCHS Consumers Healthcare Survey, with the tagline: “Stressed Out: Americans and Healthcare.” Perhaps this is why healthcare has become a top voting issue for the 2018 mid-term elections that will be held on November 6 one week from today. The first chart illustrates that healthcare costs, the economy, and family responsibilities all closely cluster as sources of stress for a
Most U.S. Physicians, Burned Out, Favor A Flavor of Single Payer Health System

Most physicians feel some level of burnout, hassled by electronic health records and lost autonomy. No wonder, then, that a majority of doctors favor some type single payer health system — one-quarter fully single payer, a la Britain’s National Health Service; and another one-third a single payer combined with a private insurance option, discovered in the 2018 Survey of America’s Physicians report on practice patterns & perspectives, published by The Physicians Foundation. Eight in ten physicians are working at full-capacity or are over-extended, the survey found. Furthermore, 62% of doctors are pessimistic about the future of medicine. Physician burnout is a
Self-Care is Healthcare for Everyday People

Patients are the new healthcare payors, and as such, taking on the role of health consumers. In fact, health and wellness consumers have existed since a person purchased the first toothpaste, aspirin, heating pad, and moisturizing cream at retail. Or consulted with their neighborhood herbalista, homeopathic practitioner, therapeutic masseuse, or skin aesthetician. Today, the health and wellness consumer can DIY all of these things at home through a huge array of products available in pharmacies, supermarkets, Big Box stores, cosmetic superstores, convenience and dollar stores, and other retail channels – increasingly, online (THINK, of course, of Amazon — more on
Healthcare, and Especially Covering Pre-Existing Conditions, Ranks High for Voters in 2018
President Trump and his administrative have been trying to make the ACA fail, claim most U.S. adults. Thus, the public holds the POTUS and the Republican party responsible for moving the Affordable Care Act forward….or not, according to the July 2018 Kaiser Health Tracking Poll conducted by the Kaiser Family Foundation (KFF). Health care will be a key issue in the 2018 mid-term elections that will be held in November. Among U.S. voters’ key health care concerns in 2018, one ranks “most” or “very important” for two-thirds of Americans: that is continuing to protect people with pre-existing health conditions. Other issues
Consumers Consider Cost When They Think About Medical Innovation
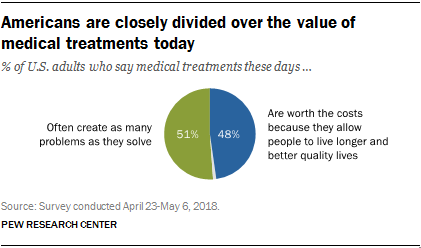
While the vast majority of Americans say that science has made life easier for most people, and especially for health care, people are split in questioning the financial cost and value of medical treatments, the Pew Research Center has found. The first chart illustrates the percent of Americans identifying various aspects of medical treatments as “big problems.” If you add in people who see these as “small problems,” 9 in 10 Americans say that all of these line items are “problems.” In the sample, two-thirds of respondents had seen a health care provider for an illness or medical condition in
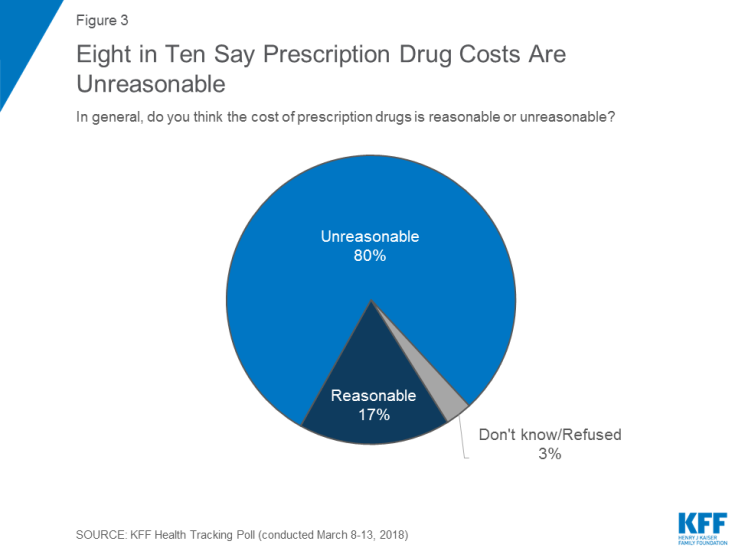
Healthcare Policies We Can Agree On: Pre-Existing Conditions, Drug Prices, and PillPack – the June 2018 KFF Health Tracking Poll
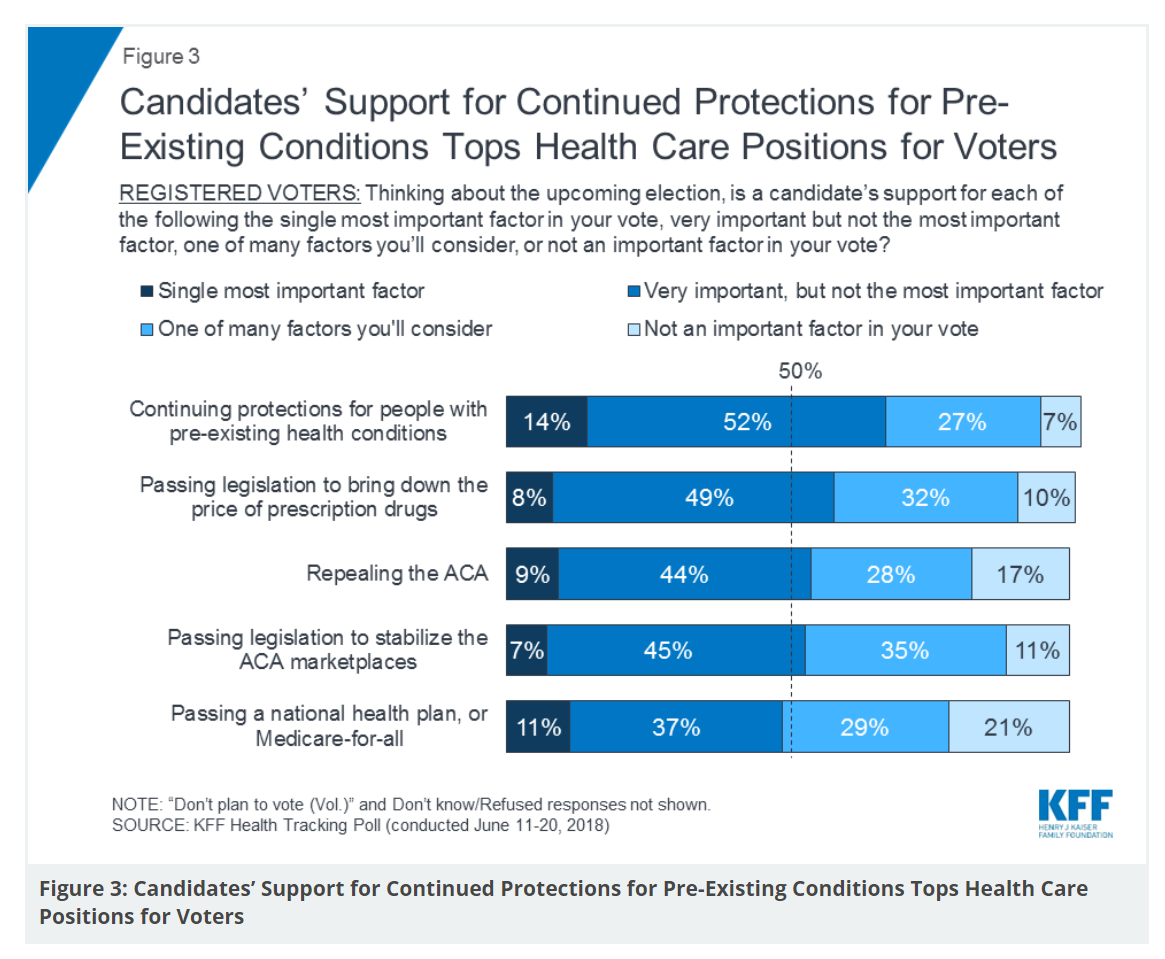
There are countless chasms in the U.S. this moment in social, political, and economic perspectives. but one issue is on the mind of most American voters where there is evidence of some agreements: health care, as evidenced in the June 2018 Health Tracking Poll from Kaiser Family Foundation. Top-line, health care is one of the most important issues that voters want addressed in the 2018 mid-term elections, tied with the economy. Immigration, gun policy, and foreign policy follow. While health care is most important to voters registered as Democrats, Republicans rank it very important. Among various specific health care factors, protecting
Obese, Access-Challenged and Self-Rationing: America’s Health Vs Rest-of-World

The U.S. gets relatively low ROI for its relatively exorbitant spending on healthcare, noted once again in the latest Health at a Glance, the annual OECD report on member nations’ healthcare systems. The report includes U.S. country data asking, “How does the United States compare?” with its sister OECD countries. The answer is, “not well across most population health, access, and mortality measures.” For the Cliff’s Notes/Where’s Waldo top-line of the research, find the two long bars in this chart heading “south” of the OECD average, and one long blue bar going “north.” The northern climbing bar
The True Costs of Diabetes Go Well Beyond the Wallet

The daily life of a person managing diabetes feels many costs: at work, on relationships, at play, during sleep, on time, on mental health, and to be sure, on personal finances. The True Cost of Diabetes report from Upwell details the many tolls on the person with diabetes. The first-order impact for a patient engaging in self-care to manage diabetes is time that the many tasks in a day borrow from work, sleep, home-keeping, and relationships. Seventy percent of PwD (people with diabetes) checks blood sugar at least once a day (41% one to two times, 29% three to five
Health Care for a Typical Working Family of Four in America Will Cost $28,166 in 2018
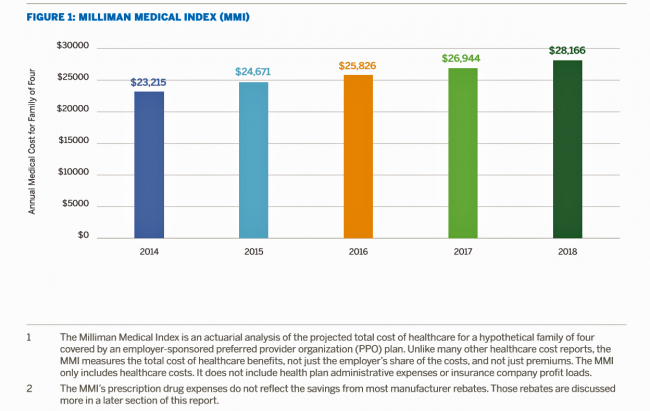
What could $28,166 buy you in 2018? A new car? A year of your child’s college education? A plot of land for your retirement home? Or a year of healthcare for a family of four? Welcome to this year’s edition of the Milliman Medical Index (MMI), one of the most important forecasts of the year in the world of the Health Populi blog and THINK-Health universe. That’s because we’re in the business of thinking about the future of health and health care through the health economics lens; the MMI is a key component of our ongoing environmental analysis of the
The Gap Between the Trump Administration’s Promise of Reducing Rx Costs for Consumers and What People Really Want
This is what happened to pharma stock prices on Friday after President Trump and Secretary of Health and Human Services Alex Azar outlined their new policies focusing on prescription drug prices. The graph is the Nasdaq U.S. Smart Pharmaceuticals Index (NQSSPH) from May 11, 2018, the date when POTUS and Secretary Azar made their announcement. What this upward driving curve indicates, from the start of stock trading in the morning until the ring of the closing bell, is that the pharma industry players, both manufacturers and PBMs, were quite delighted with what they heard. The blueprint for restructuring the prescription drug industry,
Having Health Insurance Is a Social Determinant of Health: the implications of growing uninsured in the U.S.
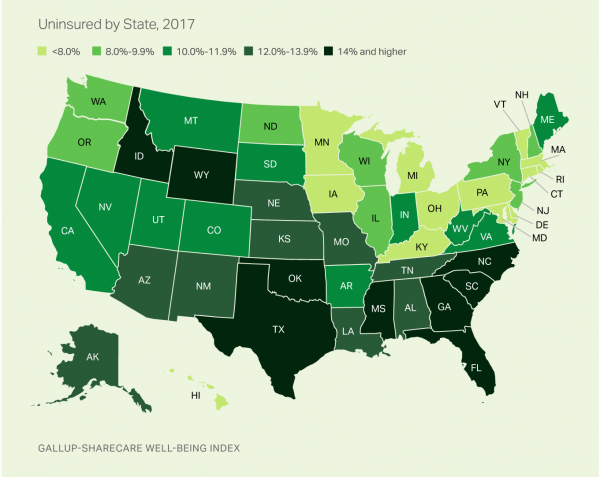
The rolls of the uninsured are growing in America, the latest Gallup-Sharecare Poll indicates. The U.S. uninsurance rate rose to 12.2% by the fourth quarter of 2017, up 1.3 percentage points from the year before. 2017 reversed advancements in health insurance coverage increases since the advent of the Affordable Care Act, and for the first time since 2014 no states’ uninsured rates fell. The 17 states with declines in insurance rates were Arizona, Colorado, Florida, Hawaii, Illinois, Indiana, Iowa, Missouri, New Mexico, New York, North Carolina, South Carolina, Texas, Utah, Washington, West Virginia, Wisconsin, and Wyoming. Among these, the greatest
Healthcare Access and Cost Top Americans’ Concerns in Latest Gallup Poll

Healthcare — availability and affordability — is a more intense worry for Americans in March 2018 than crime and violence, Federal spending, guns, drug use, and hunger and homelessness. The Gallup Poll, fielded in the first week of March 2018, found that peoples’ overall economic and employment concerns are on the decline since 2010, at the height of the Great Recession which began in 2008. While 70% of Americans were worried about economic matters in 2010, only 34% of people in the U.S. were worried about the economy, and 23% about unemployment, in March 2018. Gallup has asked this “worry”
How We Spend Versus What We Get: America’s Healthcare Spending Makes for Poor Health
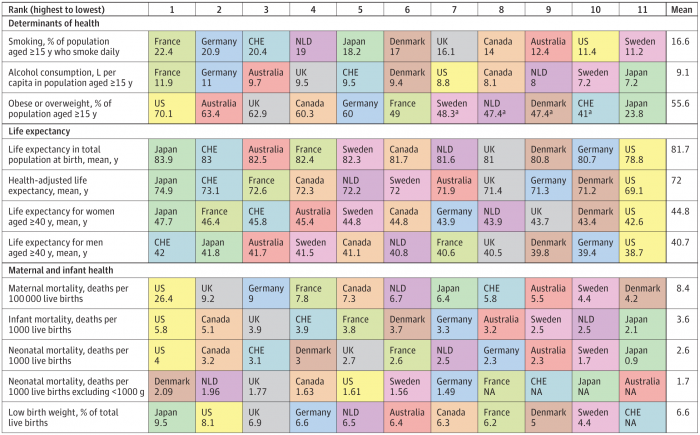
The U.S. spent nearly twice as much as other wealthy countries on healthcare, mostly due to higher prices for both labor and products (especially prescription drugs). And, America spends more on administrative costs compared to other high-income countries. What do U.S. taxpayers get in return for that spending? Lower life spans, higher maternal and infant mortality, and the highest level of obesity and overweight among our OECD peer nations. These sobering statistics were published in Health Care Spending in the United States and Other High-Income Countries this week in JAMA, the Journal of the American Medical Association. The study analyzes
Majority Rules? The Right to Affordable Health Care is A Right for All Americans
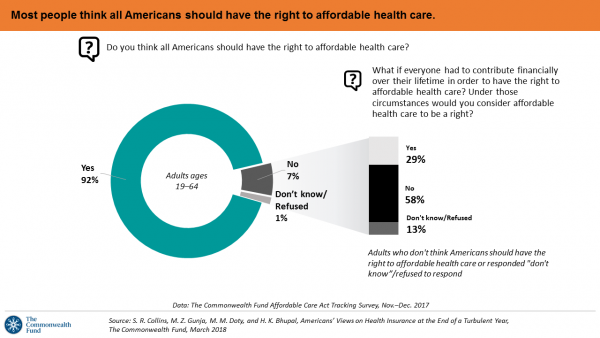
If we’re playing a game of “majority rules,” then everyone in America would have the right to affordable health care, according to a new poll from The Commonwealth Fund. The report is aptly titled, Americans’ Views on Health Insurance at the End of a Turbulent Year. The Fund surveyed 2,410 U.S. adults, age 19 to 64, by phone in November and December 2017. This is the sixth survey conducted by the Fund to track Americans’ views of the Affordable Care Act; the first survey was fielded in mid-to-fall 2013. 9 in 10 working-age adults say “yes” indeed, my fellow Americans
A Tale of Two States: Idaho, Limiting Health Plan Benefits; and Oregon, Moving Toward Universal Health Care
The United States don’t feel very united these days on a whole range of issues. But today, I’m struck by a 180-degree-apart chasm between Idaho and Oregon. While the centers of these two states only lie 290 miles from each other, they are worlds apart when it comes to their views on their residents as health citizens. Idaho. First, let’s travel to Idaho, aka the Gem State due to its rich endowment of natural resources. Health insurers in the state are now allowed to offer plans with limited benefits, escaping the rules for plans in the Affordable Care Act that
The United States of Care Launches to Promote Healthcare for All of US

Let’s change the conversation and put healthcare over politics. Sounds just right, doesn’t it? If you’re reading Health Populi, then you’re keen on health policy, health economics, most of all, patients: now playing starring roles as consumers, caregivers, and payors in their own care. Andy Slavitt, former Acting Administrator of the Centers for Medicare and Medicaid Services (CMS), has assembled a diverse group of health care leaders who care about those patients/people, too, appropriately named the United States of Care. Founders include Dr. Bill Frist, former Republican U.S. Senator from Tennessee, Dave Durenberger, former Republican U.S. Senator from Minnesota, and
Hug Your Physician: S/He Needs It – Listening to the 2018 Medscape National Physician Burnout & Depression Report

Two in five U.S. physicians feels burned out, according to the Medscape National Physician Burnout & Depression Report for 2018. This year, Medscape explicitly adds the condition of “depression” to its important study, and its title. In 2017, the Medscape report was about bias and burnout. Physicians involved in primary care specialties and critical care are especially at-risk for burnout, the study found. One in five OBGYNs experience both burnout and depression. Furthermore, there’s a big gender disparity when it comes to feeling burned out: nearly one-half of female physicians feel burnout compared with 38% of male doctors. Being employed by
Calling Out Health Disparities on Martin Luther King Day 2018

On this day appreciating the legacy of Martin Luther King, Jr., I post a photo of him in my hometown of Detroit in 1963, giving a preliminary version of the “I Have a Dream” speech he would deliver two months later in Washington, DC. Wisdom from the speech: “But now more than ever before, America is forced to grapple with this problem, for the shape of the world today does not afford us the luxury of an anemic democracy. The price that this nation must pay for the continued oppression and exploitation of the Negro or any other minority group
Most Americans Say Healthcare is #1 Policy Issue Entering 2018

Concerns about health care are, by a large margin, the top domestic policy issue U.S. voters identified as they enter 2018. The proportion of Americans citing healthcare as the top public agenda priority grew by 50% since 2016, from 31% two years ago to 48%. Taxes rank #2 this year, garnering 31% of Americans’ concerned, followed by immigration, which has remained flat cited by about one-in-four Americans. The Associated Press (AP)-NORC Center for Public Affairs Research polled 1,444 U.S. adults 18 and over between November 30 and December 4, 2017 for this survey. While one-half of Americans would like the
Let’s Increase Life Expectancy in America in 2018 – A New Year for Opioids, Social Determinants, and Financial Health
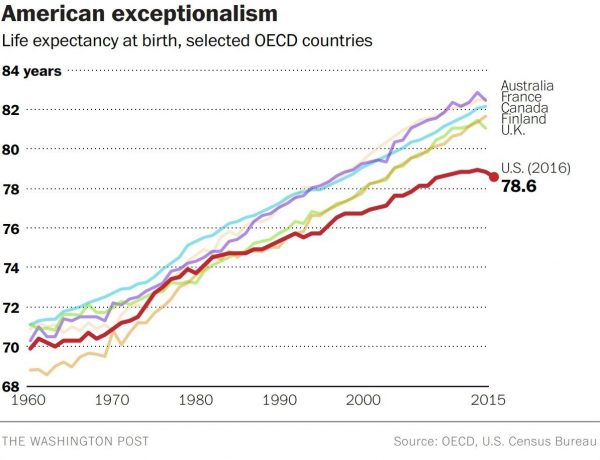
For this end-of-year post leading into 2018, I choose to address the big topic of how long we live in America, and what underpins the sobering fact that life expectancy is falling. Life expectancy in the United States declined to 78.6 years in 2016, placing America at number 37 on the list of 137 countries the World Economic Forum (WEF) has ranked in their annual Global Competitiveness Report 2017-2018. The first chart shows the declining years for Americans compared with health citizens of Australia, France, Canada, Finland, and the UK. While Australians’ and Britons’ life expectancies declined from 2015-16, their
Health Consumers Face the New Year Concerned About Costs, Security and Caring – Health Populi’s 2018 Forecast
As 2018 approaches, consumers will gather healthy New Year’s Resolutions together. Entering the New Year, most Americans are also dealing with concerns about healthcare costs, cybersecurity, and caring – for physical health, mental stress, and the nation. Healthcare costs continue to be top-of-mind for consumer pocketbook issues. Entrenched frugality is the new consumer ethos. While the economy might be statistically improving, American consumers’ haven’t regained confidence. In 2018, frugality will impact how people look at healthcare costs. 88% of US consumers are likely to consider cost when selecting a healthcare provider, a Conduent survey found. Physicians know this: 81% of
Support for the Affordable Care Act the Highest Since Passage
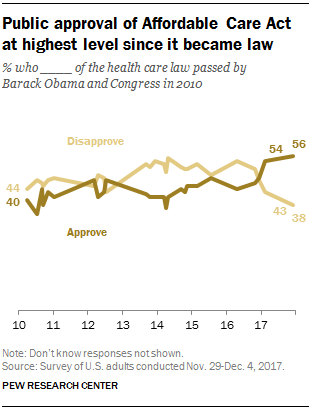
Americans’ approval of the Affordable Care Act reached its apex in December 2017, the Pew Research Center found. The proportion of people approving the ACA has been growing since the middle of 2016, now at 56% of the public. The timing of this survey, conducted at the end of November and first few days of December 2017, coincides with Congress’s arm-wrestling a tax bill that would eliminate the individual mandate for health insurance which is an ACA building block for universal coverage in the United States. Most people in the U.S. also believe that the ACA has had a positive
Six Healthcare News Stories to Keep Hospital CFOs Up At Night
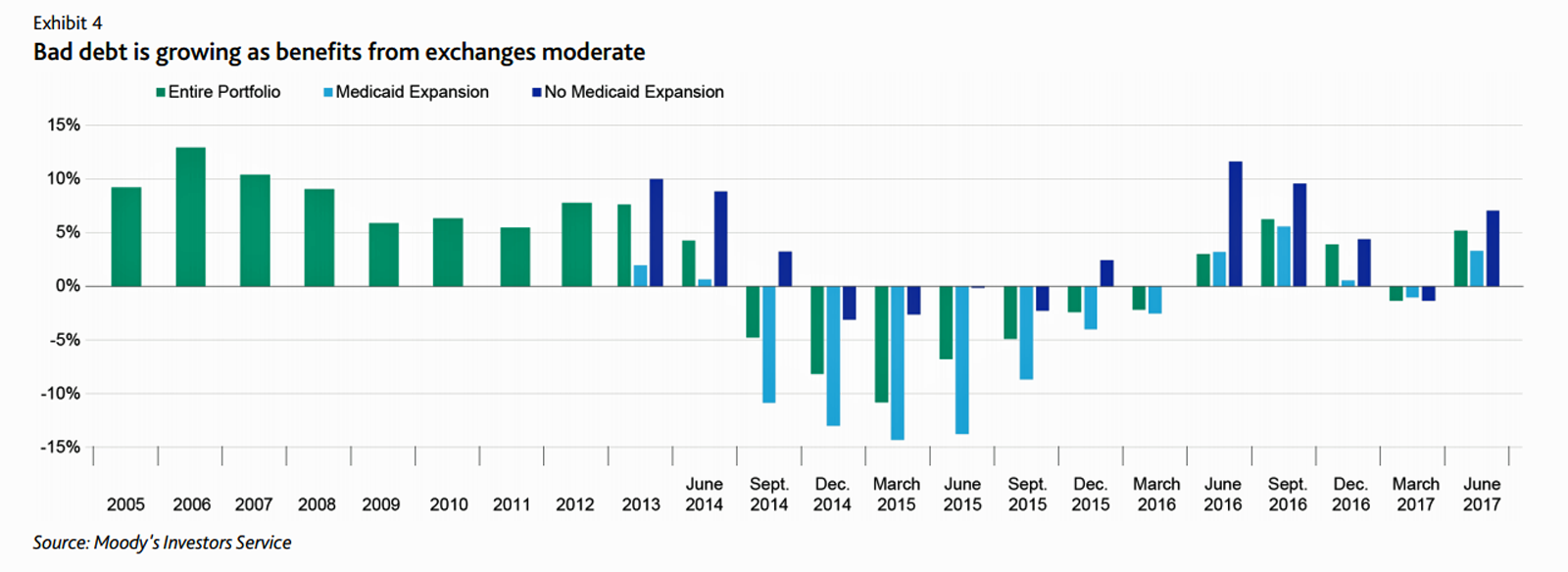
At this moment, the healthcare job I’d least like to have is that of a non-profit hospital Chief Financial Officer (CFO). Five news stories, published in the past 24 hours, tell the tale: First, Moody’s forecast for non-profit hospitals and healthcare in 2018 is negative due to reimbursement and expense pressures. The investors report cited an expected contraction in cash flow, lower reimbursement rates, and rising expense pressures in the midst of rising bad debt. Second, three-quarters of Federally Qualified Health Centers plan to lay off staff given lack of budget allocations resulting from Congressional inaction. Furthermore, if the $3.6
Health Care Is 2.5 More Expensive Than Food for the Average U.S. Family
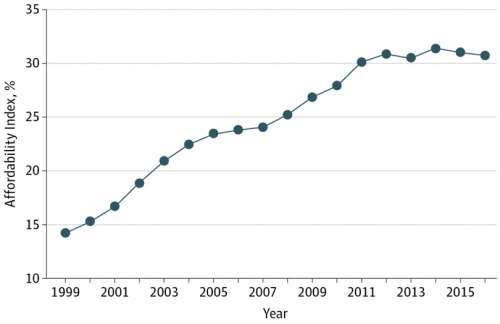
The math is straightforward. Assume “A” equals $59.039, the median household income in 2016. Assume “B” is $18,142, the mean employer-sponsored family insurance premium last year. B divided by A equals 30.7%, which is the percent of the average U.S. family’s income represented by the premium cost of health insurance. Compare that to what American households spent on food: just over $7,000, including groceries and eating out (which is garnering a larger share of U.S. eating opportunities, a topic for another post). Thus, health care represents, via the home’s health insurance premium, represents 2.5 times more than food for the
What Patients Feel About Technology, Healthcare Costs and Social Determinants
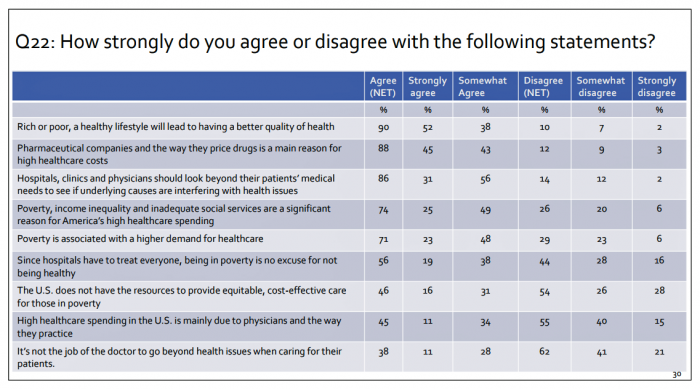
U.S. consumers feel positive about the roles of technology and social determinants in improving healthcare, but are concerned about costs, according to the 2017 Patient Survey Report conducted for The Physicians Foundation. The survey gauged patients’ perspectives across four issues: the physician-patient relationship, the cost of healthcare, social determinants of health, and lifestyle choices. Two key threads in the research explain how Americans feel about healthcare in the U.S. at this moment: the role of technology and the cost of health care. First, the vast majority of consumers view technology, broadly defined, as important for their health care. 85% of people
2017 Rx Cost Trend Over 5 Times U.S. Inflation, Segal Projects
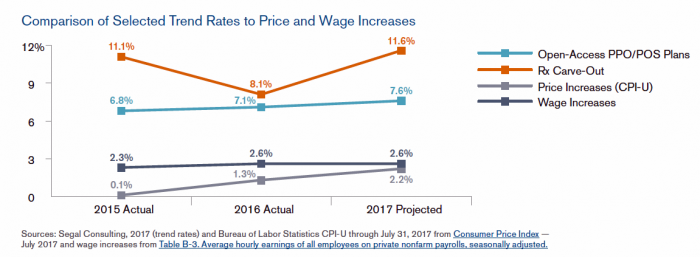
Driven by price increases, costs for the prescription drug benefit carve-out will increase 11.6% this year, based on Segal Consulting’s survey report, High Rx Cost Trends Projected to Be Lower for 2018, published today. The report is accessible on the Segal Co. website. While the Segal team expects prescription drug (Rx) benefit plan cost trends to be “less severe” in 2018, Rx cost increases is a top priority for many sponsors of health plans as their rate of increase far exceeds those for inpatient hospital claims or physician expense. Drug costs continue to be the fastest-growing line item in health
Employees Continue To Pick Up More Health Insurance Costs, Even As Their Growth Slows
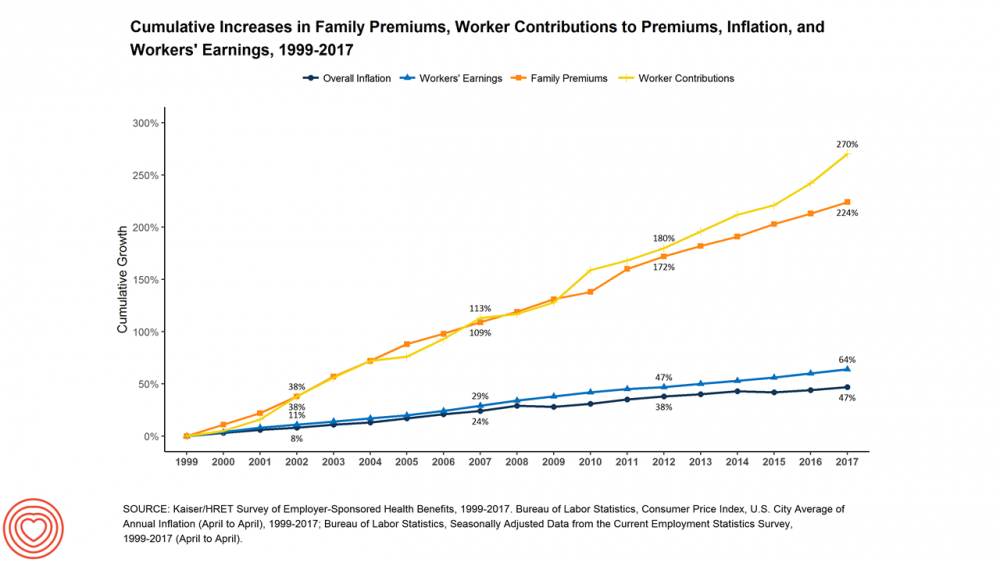
The average cost of an employer=sponsored health plan for a family reached $18,764 in 2017. While this premium grew overall by a historically relative low of 3.4%, employees covered under that plan faced an increase of 8.3% over what their plan share cost them in 2016, according to the 2017 Employer Health Benefit Survey published today by the Kaiser Family Foundation. [Here’s a link to the 2016 KFF report, which provided the baseline for this 8.3% calculation]. Average family premiums at the workplace rose 19% since 2012, a slowdown from the two previous five-year periods — 30% between 2007 and 2012, and
Women’s Access to Health Care Improved Under the Affordable Care Act
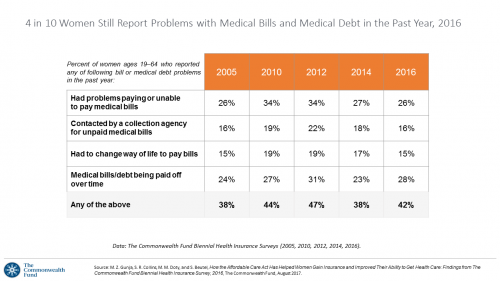
The Affordable Care Act (ACT) was implemented in 2010. Since the inception of the ACA, the proportion of uninsured women in the U.S. fell by nearly one-half, from 19 million in 2010 to 11 million in 2016. The Commonwealth Fund has documented the healthcare gains that American women made since the ACA launch in their issue brief, How the Affordable Care Act Has Helped Women Gain Insurance and Improved Their Ability to Get Health Care, published earlier this month. The first chart talks about insurance: health care plan coverage, which is the prime raison d’être of the ACA. It’s
Most Americans, Including Republicans, Want President Trump’s Administration to Make the ACA Work – Not Fail
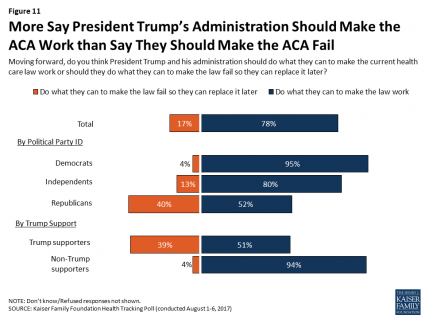
8 in 10 Americans want President Trump and his administration to do what they can to make the Affordable Care Act work, according to the latest August 2017 health tracking poll from Kaiser Family Foundation (KFF). By political party affiliation, this includes 95% of Democrats, 80% of Independents, and 52% of Republicans (that is, to emphasize the point, just over half, a majority, of Republicans). More Americans are also relieved and happy, versus disappointed and angry, that the ACA repeal did not occur (thus far), the second chart illustrates. To be sure, a majority of Republicans register anger and disappointment,






 Grateful to Gregg Malkary for inviting me to join his podcast
Grateful to Gregg Malkary for inviting me to join his podcast  This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're
This conversation with Lynn Hanessian, chief strategist at Edelman, rings truer in today's context than on the day we recorded it. We're