U.S. Health Care in 2025 Requires Scenario Planning: The Uncertainties (AI!?) That Inspire DIY Healthcare

As Weight Watchers prepares to initiate bankruptcy proceedings, I file the news event under “thinking the unthinkable.” “Thinking about the unthinkable” is what Herman Kahn, a father of scenario planning, asked us to do when he pioneered the process. In this book, for Kahn, “the unthinkable” was thermonuclear war, and the year was 1962. The book was tag-lined as “must reading for an informed public” and in it, Kahn I’ve been drawn back to this book lately because of a more intense workflow using
Most Americans Don’t Want to Cut Medicaid (Including Republicans)
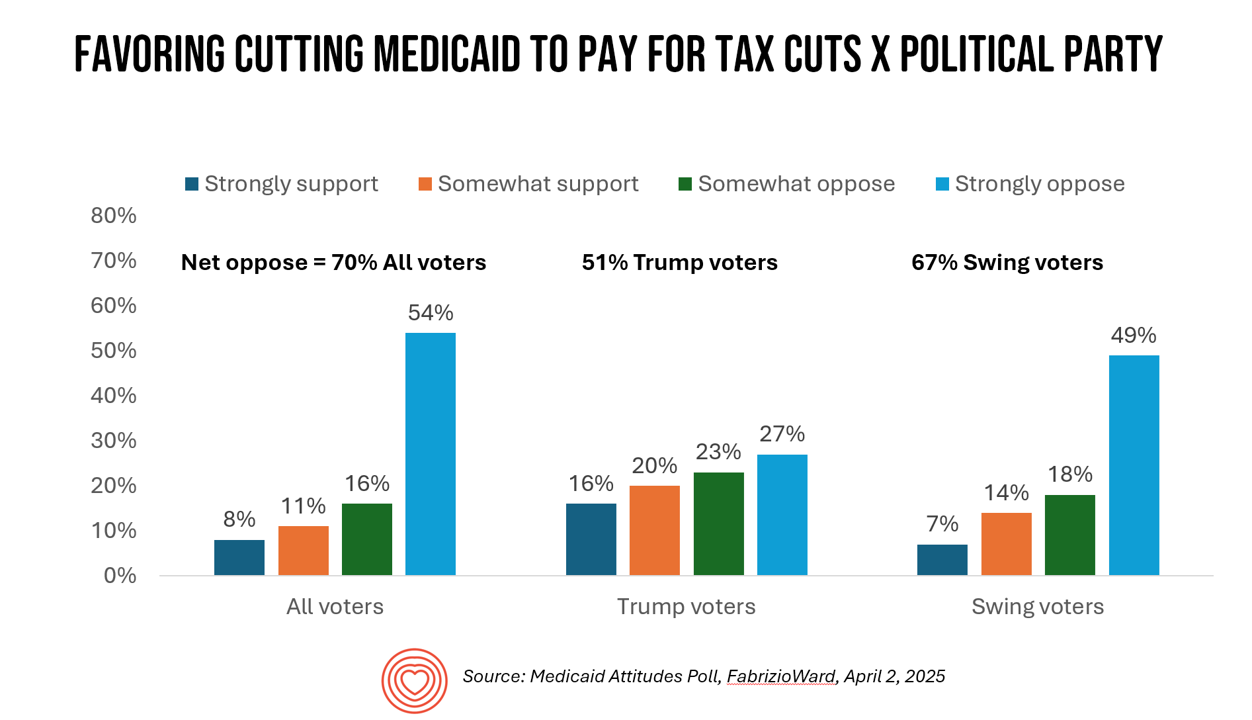
With potential down-sizing of Medicaid on the short-term U.S. political horizon, a fascinating poll found that most people identifying as Republican would not favor cuts to Medicaid. What fascinates me about this survey, published earlier this week, is that it was conducted by FabrizioWard, a polling firm that has often been used by President Trump. The firm’s Bob Ward told POLITICO that, “There’s really not a political appetite out there to go after Medicaid to pay for tax cuts. Medicaid has touched so many families that people have made up their minds about what
Consumers Are Financially Stressed – What This Means for Health/Care in 2025
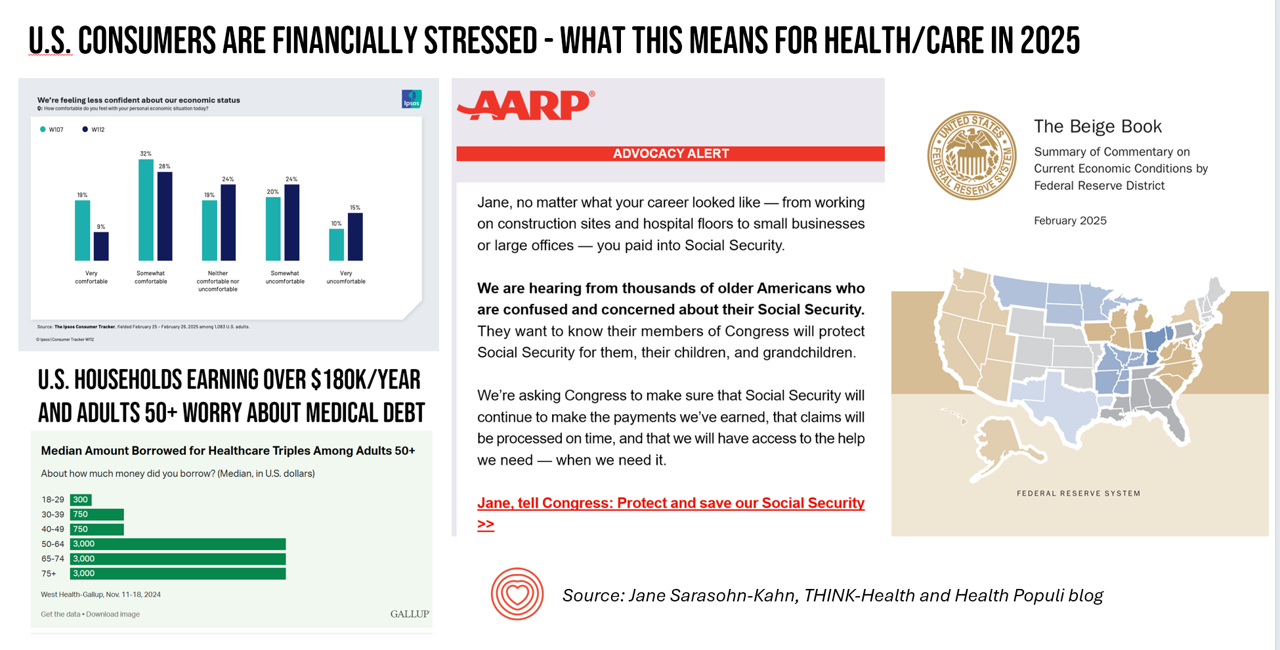
People define health across many life-flows: physical health, mental health, social health, appearance (“how I look impacts how I feel”) and, to be sure, financial well-being. In tracking this last health factor for U.S. consumers, several pollsters are painting a picture of financially-stressed Americans as President Trump tallies his first six weeks into the job. The top-line of the studies is that the percent of people in America feeling financially wobbly has increased since the fourth quarter of 2024. I’ll review these studies in this post, and discuss several potential impacts we should keep in mind for peoples’ health and
Think Quintuple Aim This Week at #HIMSS25
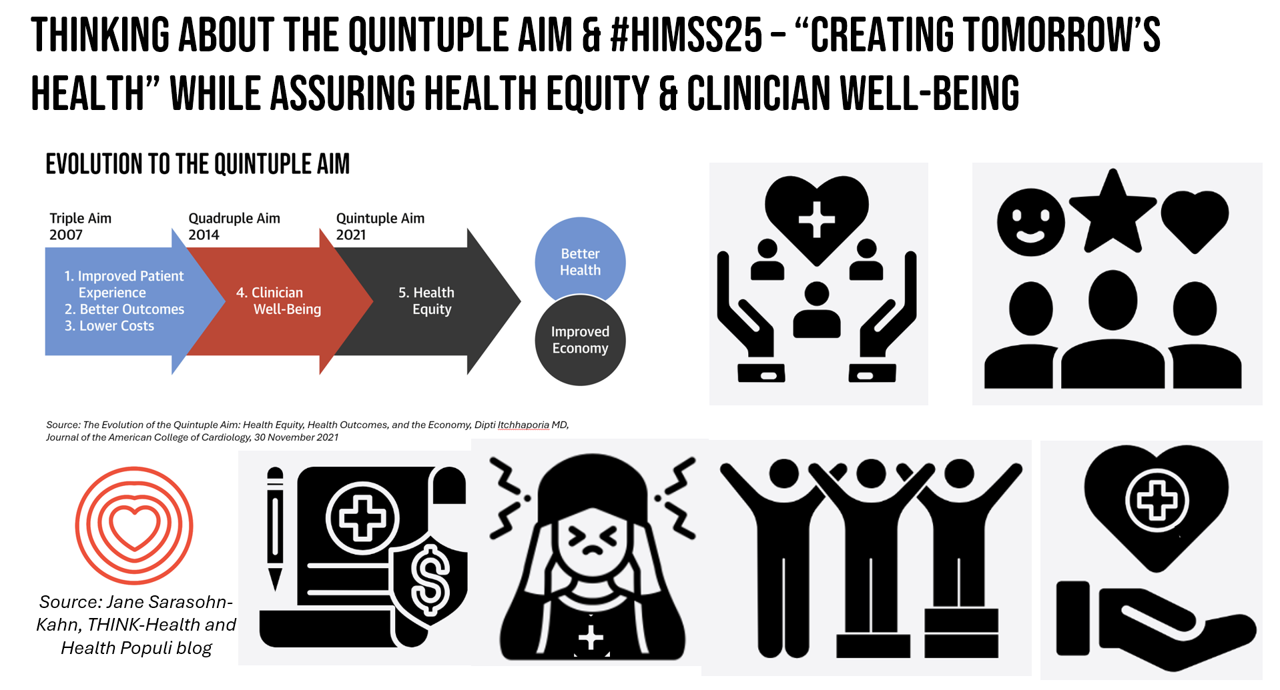
As HIMSS 2025, the largest annual conference on health information and innovation meets up in Las Vegas this week, we can peek into what’s on the organization’s CEO’s mind leading up to the meeting in this conversation between Hal Wolf, CEO of HIMSS, and Gil Bashe, Managing Director of FINN Partners. If you are unfamiliar with HIMSS, Hal explains in the discussion that HIMSS’s four focuses are digital health transformation, the deployment and utilization of AI as a tool, cybersecurity to protect peoples’ personal information and its use, and, workforce development. I have my own research agenda(s) underneath these themes
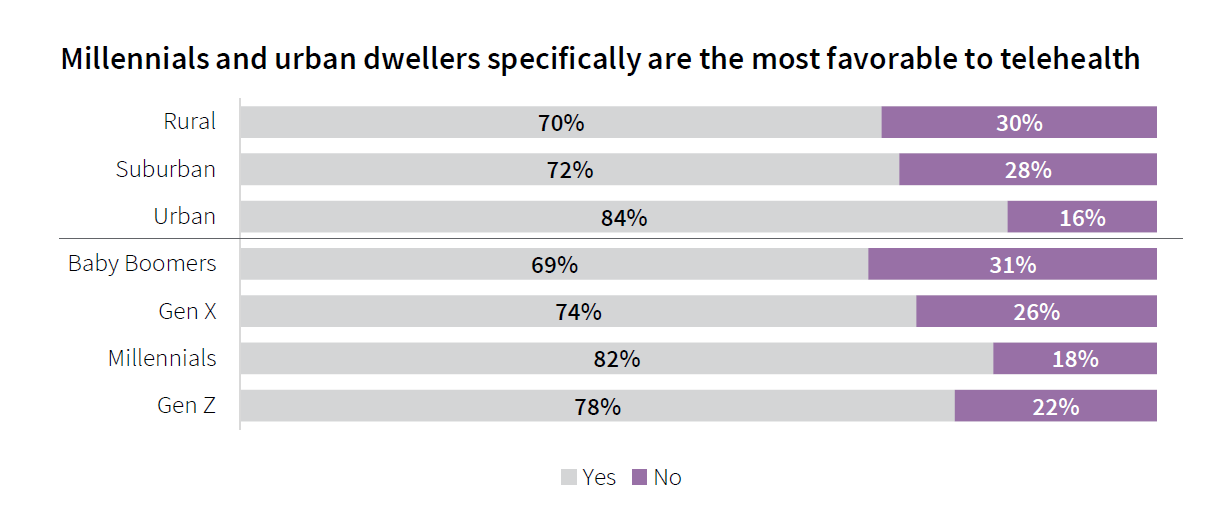
Telehealth, Right Here, Right Now: Calling on Congress to Vote for America’s Health and Well-being
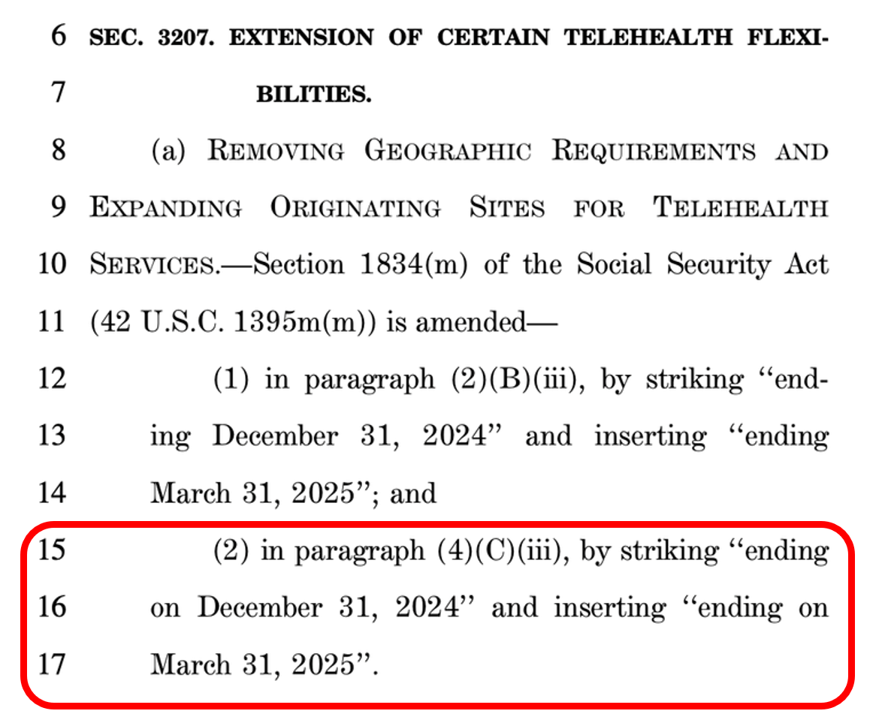
In the U.S., there are some issues that still unite most Americans in 2025. We can agree that, • The cost of eggs is too high • AI can be both exciting and promising at the same time as concerning • It sucks to have your personal data cyberattacked and breached, and, • Having access to telehealth is important. While I would be really sad to give up my omelets, I’m sticking a mindful toe into AI for some simple workflows, and I’m still dealing with the aftermath of the Change Healthcare data breach, it’s the looming telehealth deadline that’s
GLP-1s at the Pharmacy – A Lens on Consumer-Driven Retail Health (with Hims & Hers stock price update)
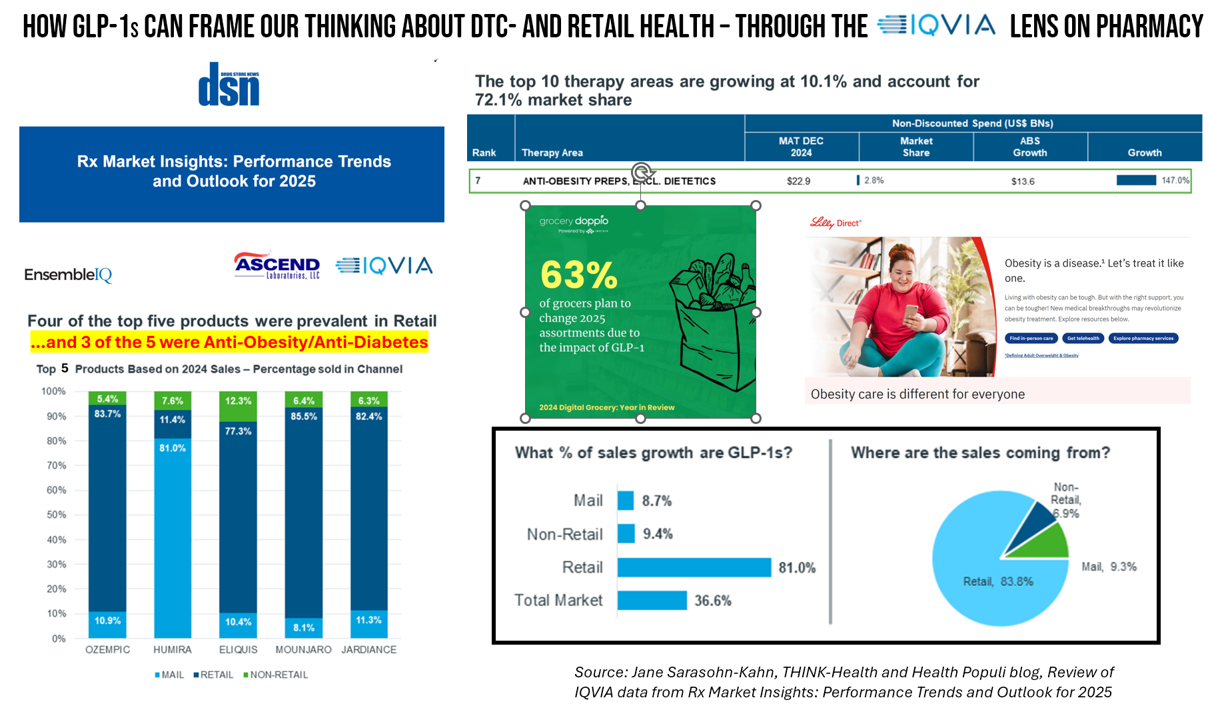
The nature of retail pharmacy is changing, with both threats and opportunities re-shaping the business itself, and the pharmacy’s role in the larger health/care ecosystem. To keep sharp on the topics, I attended Rx Market Insights: Performance Trends and Outlook for 2025, a data-rich session presented on February 18 by IQVIA and sponsored by Ascend Laboratories. The webinar was hosted by DSN (Drug Store News), appropriately so because the action-packed hour went into detail providing the current state of prescription drugs and the pharmacy in America. Doug Long, IQVIA’s VP of Industry Relations, and Scott Biggs, the company’s Director of Supplier
Measuring Progress for Life Sciences: Trust, Patient Access, and Prevention at a Fork in the Road of Public Health
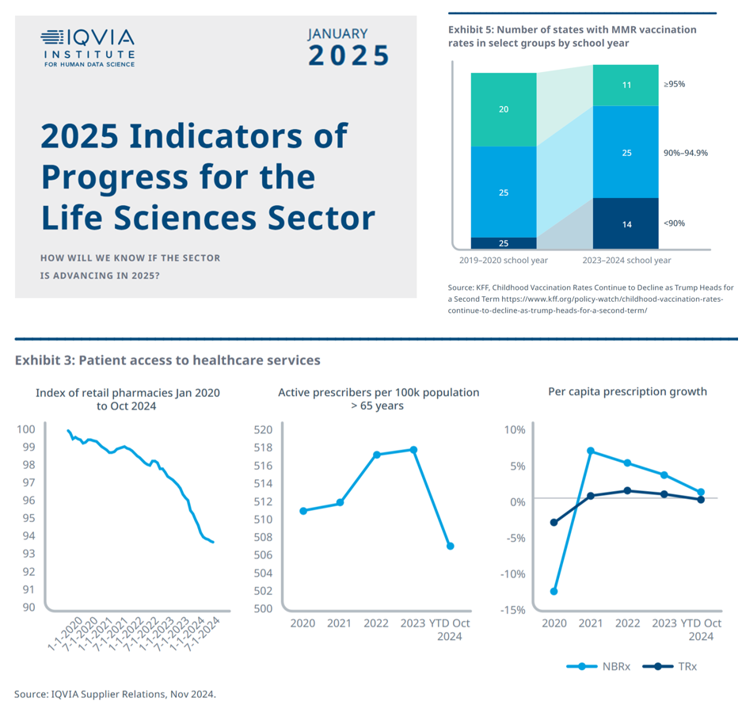
How will we know if the life sciences sector is advancing in 2025? This is the question asked at the start of the report, a Research Brief: 2025 Indicators of Progress for the Life Sciences Sector, from the IQVIA Institute for Human Data Science (IQVIA). To answer that question, IQVIA identified ten indicators for this 2025 profile on the life sciences sector. I selected four key data points for this discussion which provide particularly informative insights for my advisory work right now at the intersection of health, people/consumers, and technology: Trust for/with/in life science
Some Bipartisan Concurrence on Health Care Issues in the U.S. – But Trust in Health Care Isn’t Bipartisan – KFF’s January 2025 Polls
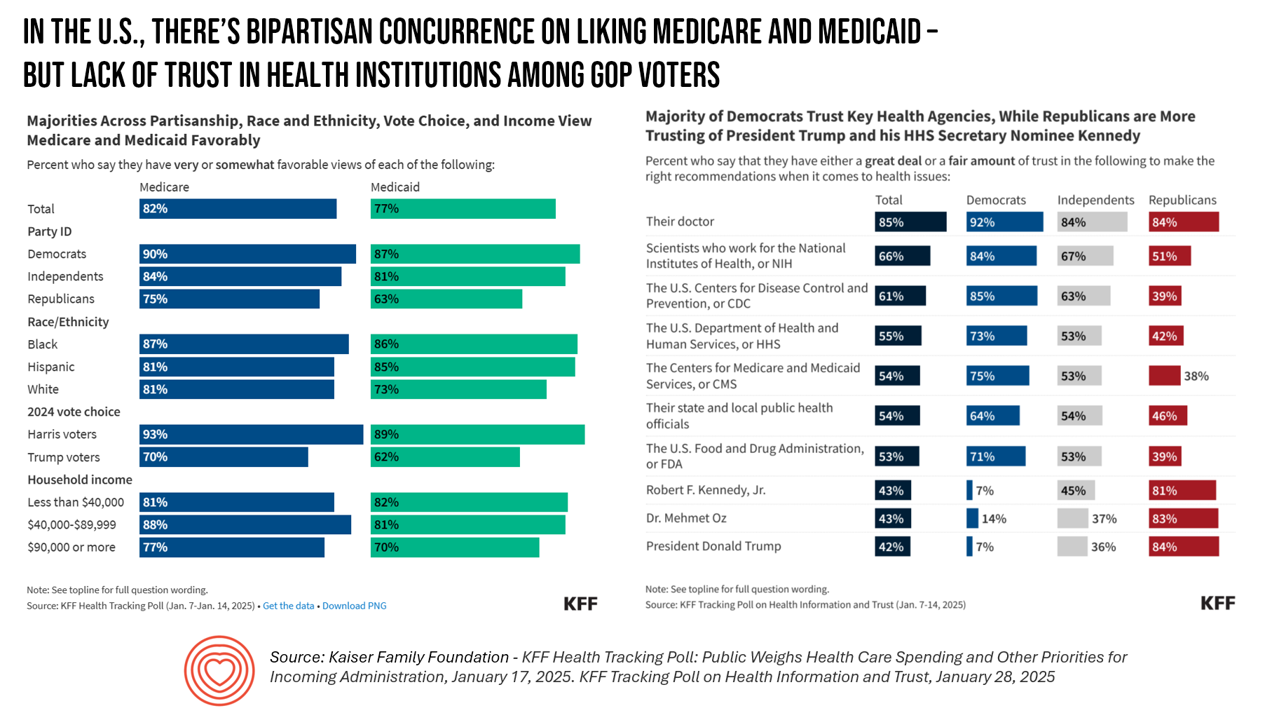
Two polls from one poll source paint at once a bipartisan and bipolar picture of U.S. health citizens when it comes to health care issues versus health care institutions in America. The Kaiser Family Foundation has hit the 2025 health policy ground running in publishing the January 2025 Health Tracking Poll last week and a poll on health care trust and mis-information yesterday. First, the health tracking poll which finds some concurrence between Democrats and Republicans on several big issues facing Americans and various aspects of their health care. As
Seeing Health/Care Everywhere at CES 2025: My Preview for #CES2025

Health/care is everywhere is the mantra on the back of my business card. And at #CES2025, that will indeed be the situation. The 2025 convening of CES (once known as the Consumer Electronics Show) in Las Vegas officially kicks off on 7 January 2025. But I’ll be there beginning 3rd January, scheduling pre-show meetings with innovators, analysts, and my own clients who will be attending the meeting. This will be my 15th year participating in CES, and marking over a decade as a member of the Consumer Technology Association (CTA). As someone who has tracked
The Rough Guide to Health/Care Consumers in 2025: The 2025 Health Populi TrendCast
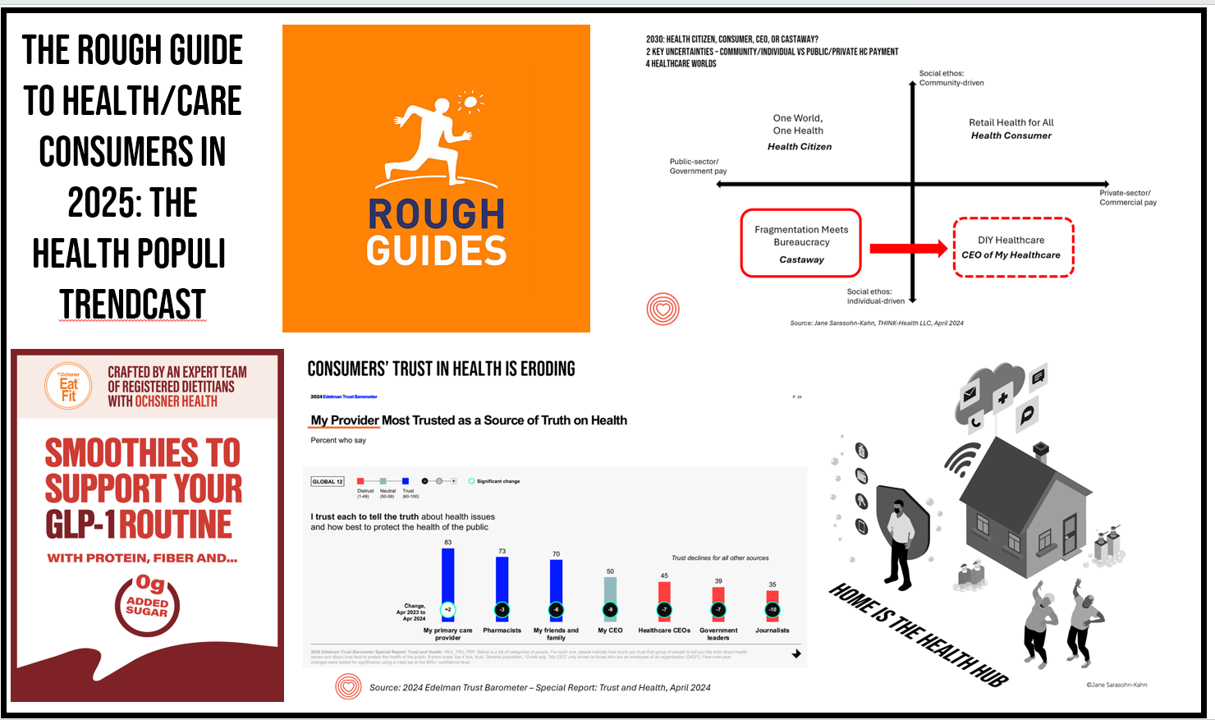
At this year-end time each year, my gift to Health Populi readers is an annual “TrendCast,” weaving together key data and stories at the convergence of people, health care, and technology with a look into the next 1-3 years. If you don’t know my work and “me,” my lens is through health economics broadly defined: I use a slash mark between “health” and “care” because of this orientation, which goes well beyond traditional measurement of how health care spending is included in a nation’s gross domestic product (GDP); I consider health across the many dimensions important to people, addressing physical,
National Healthcare Spending in the U.S. Was Nearly $5 Trillion (with a “T”) in 2023 – New Data from CMS
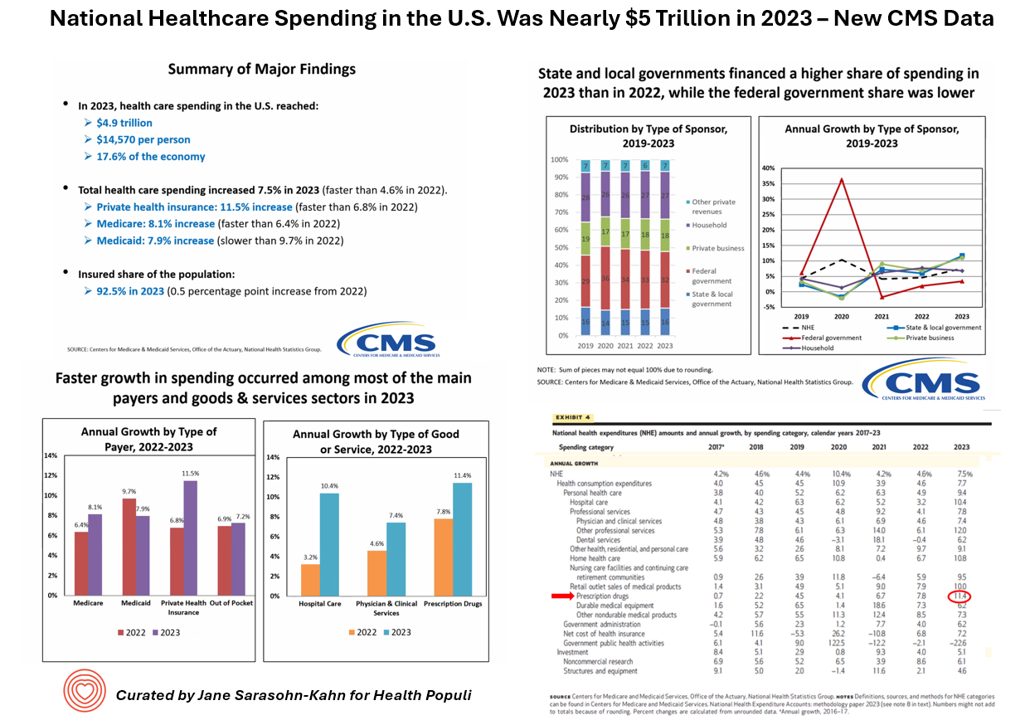
What would $5 trillion be valued around the world or on the stock market? The economy of Germany was gauged around $5 trillion in 2024. India could be the world’s 3rd largest economy by 2026 valued at $5 trillion. Nvidia could be a $5 trillion company in 2025, as could Amazon. But today we report out the latest data from the Centers for Medicare and Medicaid Services (CMS) that national health spending in America reached $4.9 trillion in 2023. The full report on national health expenditures (NHE) in the U.S. was published today in Health Affairs, which came off embargo
Most People in the U.S. Trust the CDC and NIH for Health Information, and Most Want President Trump to Strengthen Health Institutions
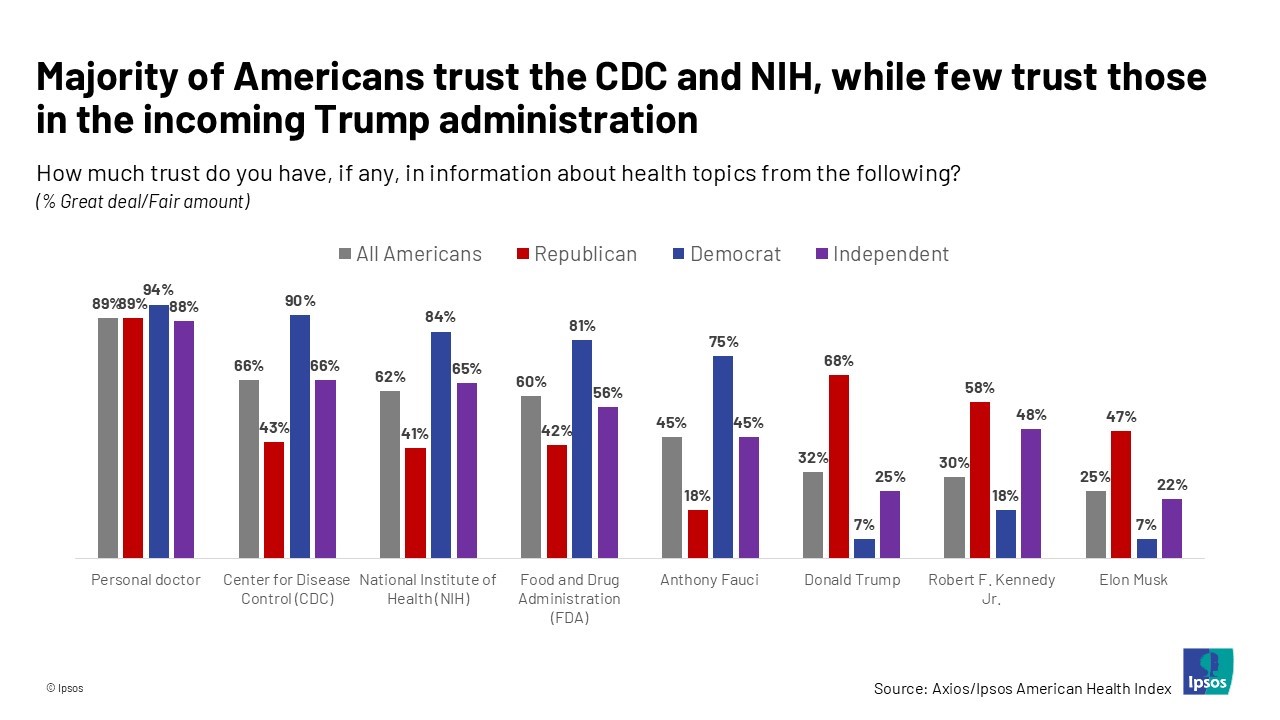
Most health citizens in the U.S. trust the CDC, NIH, and FDA, and most people also want the 47th incoming President Donald Trump to strengthen health/care institutions — from the VA and FDA to Medicare, Medicaid, as well as the CDC and Affordable Care Act. The Axios/Ipsos American Health Index, published this week, reveals both concurrence among U.S. health consumers with some striking differences across political party ID. Axios and Ipsos fielded a survey among 1,002 U.S. adults in early December to glean peoples’ perspectives on health, trust, and a variety of health and social policies.
What Stays True for U.S. Health Care Post #Election2024 (1) – Consumers’ Dissatisfaction with Drug Prices
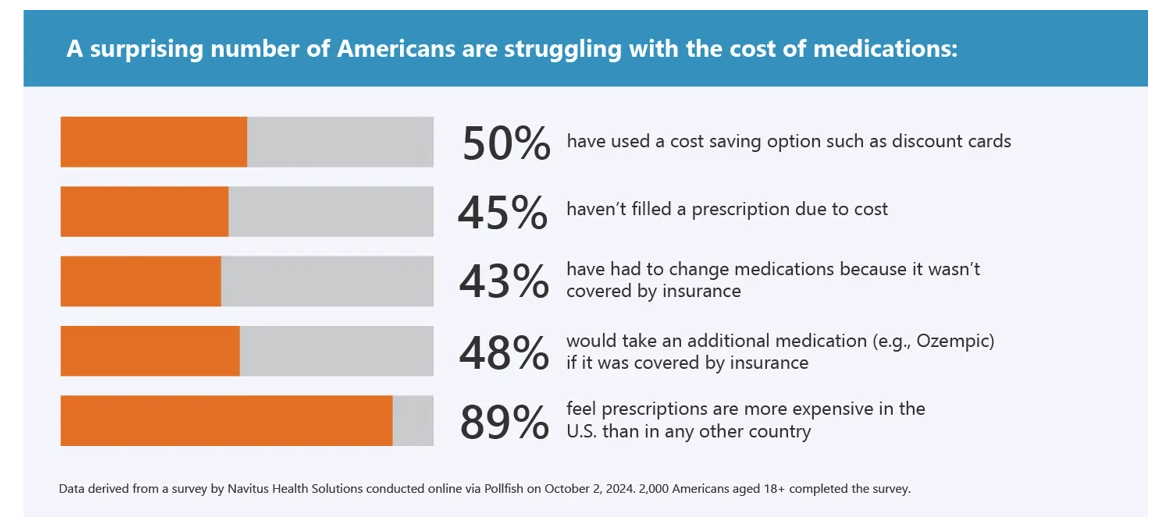
For health care, there are many uncertainties as we reflect, one week after the 2024 U.S. elections, on probably policy and market impacts that we can expect in 2025 and beyond. In today’s Health Populi post, I’ll reflect on the first of several certainties we-know-we-know about U.S. health citizens and key factors shaping the American health ecosystem. In this first of several posts on “What Stays True for U.S. Health Care Post #Election2024,” I’ll focus on U.S. consumer dissatisfaction with drug prices — across political party identification. Let’s set the context with data from a recently-published
Health Care Costs and Access On U.S. Voters’ Minds – Even If “Not on the Ballot” – Ipsos/PhRMA
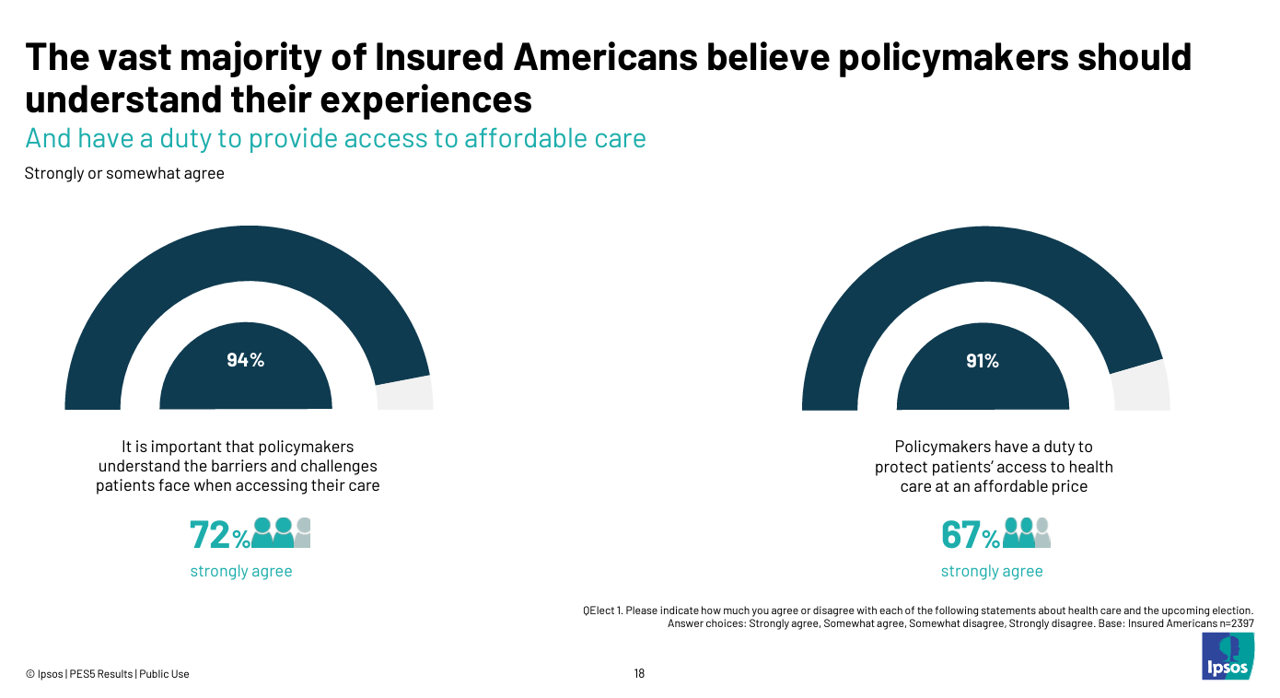
Today marks eight days before #Election2024 in the U.S. While many political pundits assert that “health care is not on the ballot,” I contend it is on voters’ minds in many ways — related to the economy (the top issue in America), social equity, and even immigration (in terms of the health care workforce). In today’s Health Populi blog, I’m digging into Access Denied: patients speak out on insurance barriers and the need for policy change, a study conducted by Ipsos on behalf of PhRMA, the Pharmaceutical Research and Manufacturers of America — the pharma industry’s advocacy organization (i.e., lobby
How Much Would Adults Age 50+ Trust AI-Generated Health Information? Not Much.
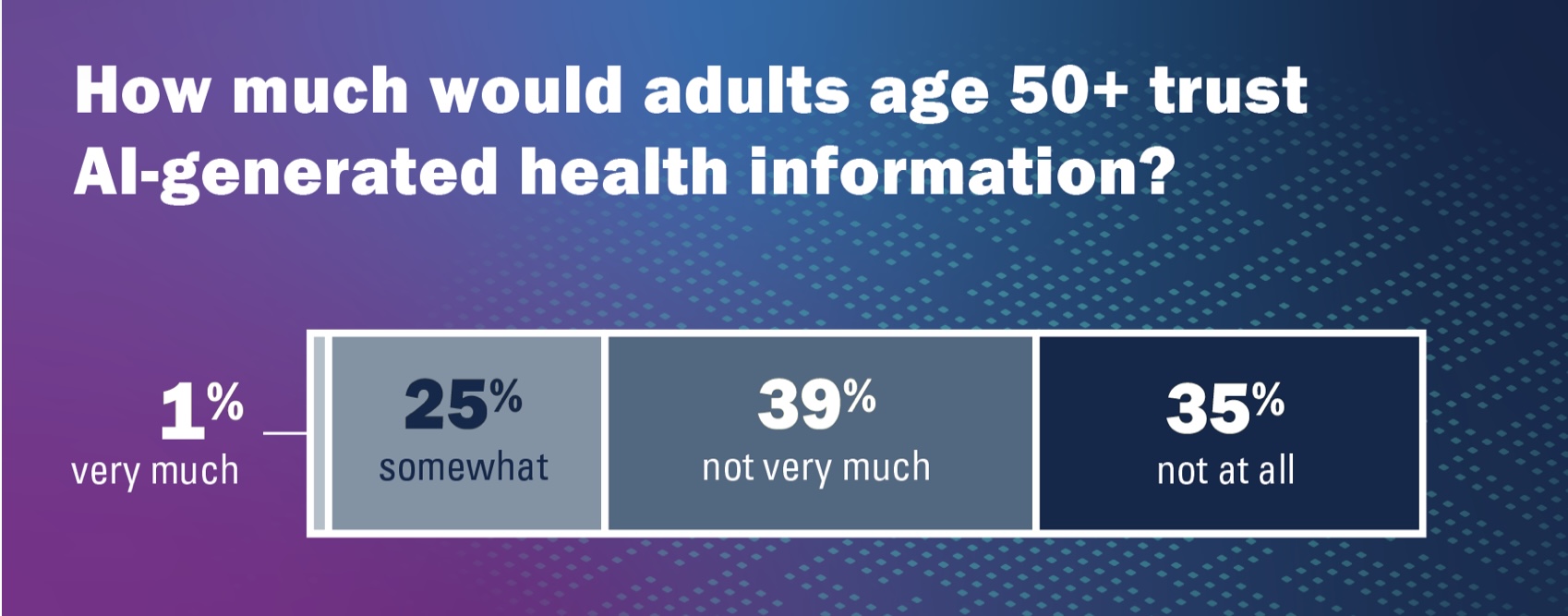
Health literacy and, indeed, literacy across the many layers relevant for health (digital, medical, financial), is a challenge for people of all ages. The Institute for Healthcare Policy Innovation’s National Poll on Healthy Aging at the University of Michigan focused on people 50 and over in their latest study published this month: Health Literacy – How Well Can Older Adults Find, Understand, and Use Health Information. On the upside, 4 in 5 older people (50+) feel confident in being able to spot health mis-information, the chart from the Poll report clearly tells us. 20% of older U.S. health citizens are
Americans Want More Health Care Issues Baked into the 2024 Elections – Gallup
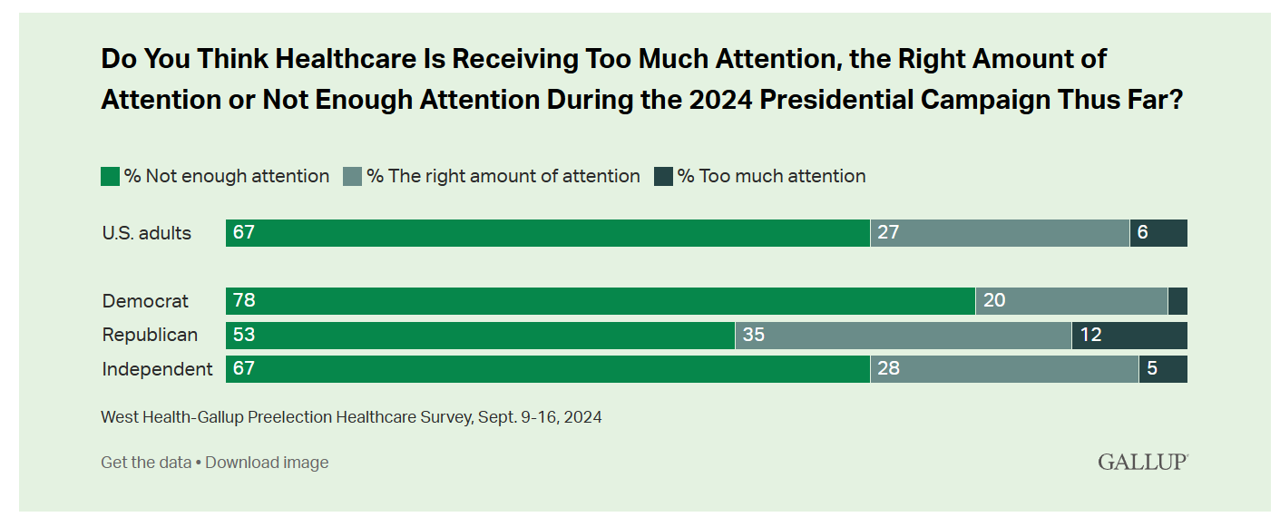
Beyond women’s health and abortion politics, most Americans are looking for more health care baked into the 2024 Elections, based on a new poll from Gallup in collaboration with West Health. Two in three U.S. adults thought health care was not receiving enough attention during the 2024 Presidential campaign as of September 2024. This is a majority shared opinion for voters across the three party IDs in the U.S., shown in the first bar graph. The research polled 3,660 U.S. adults in September, about two-thirds before the presidential debate held September 10, and about one-third
Where Democrats and Republicans Agree on Health Care Policies – From Medicare and Prescription Drugs to Gun Safety
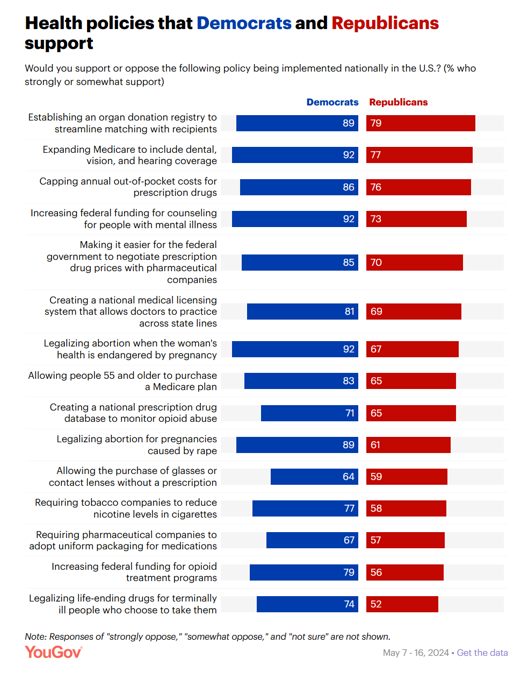
In a super-divided electorate like the U.S. with about 60 days leading up to the 2024 Elections, we might assume there are no “purple” areas of agreement between the Red (Republicans) and the Blue (Democrats) thinking in PANTONE color politics. Surprisingly, there are many health policies on which Democrats and Republicans concur, as found in a series of YouGov polls conducted in May 2024. YouGov fielded the health policies poll in five waves online, each among roughly 1,100 U.S. adults in May 2004. This bar chart summarizes health
Best Buy Health’s Latest Insights into Technology and Care at Home

In the U.S., aging in and staying at home is a priority for most people over the age of 45 — and for nearly one-half of younger people between 18 and 44 — we learn in Best Buy Health’s Research Brief discussing the company’s survey of 1,000 U.S. consumers. Best Buy Health, the health-focused operation which is part of the electronics retailer Best Buy, worked with Sage Growth Partners to assess 1,000 U.S. consumers, 18 years and over, on their perspectives on health care, technology, aging in place, and caregiving. The research was fielded
How Voting Plays Into Health, Health Equity, and Community Well-Being

“Voter registration in hospitals is the new frontier in health care.” That’s the headline in a WBUR story last week detailing the efforts of health care professionals in “amplifying” their patients’ voices inside and outside of the hospital walls by advocating for their health citizenship — through voter registration and public health policy advocacy. I’m a long-time evangelist for health citizenship and the role that a person’s engagement in the civic commons plays in one’s own health, the health of their communities and of the nation as a whole. I’m not alone
The Health Care Costs for Someone Retiring in 2024 in the U.S. Will Reach $165,000 – Fidelity’s 23rd Annual Update
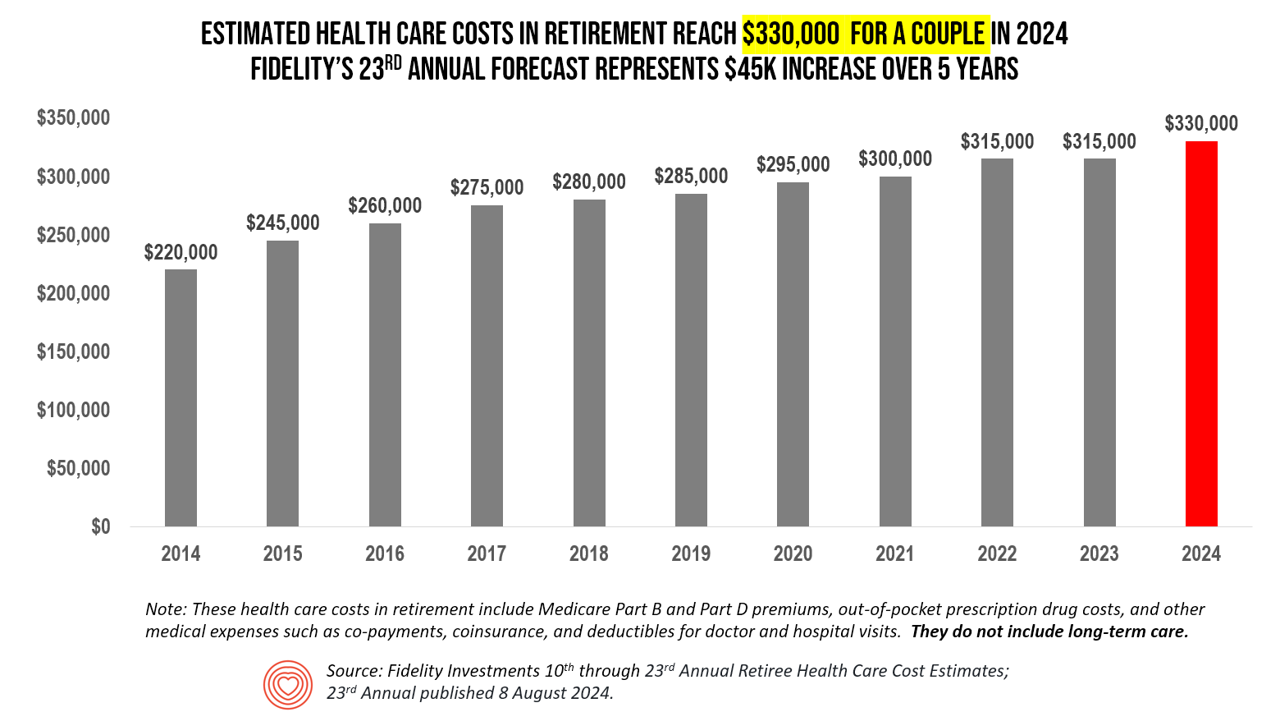
The average person in the U.S. retiring in 2024 will need to bank $165,000 to pay for health care costs in retirement — a sum that does not include long-term care, Fidelity Investments advises us in the 23rd annual look at this always-impactful (and sobering) forecast. I’ve covered this study every year since 2011 here in Health Populi, continuing to add to this bar chart; in the interest of space and legibility, I started this year’s version of the chart at 2014, when the cost for a couple was gauged at $220K. Fidelity began
The Cost of GLP-1 Drugs on Payers’ Minds as Nearly 1/3rd of U.S. Consumers Could Become Users
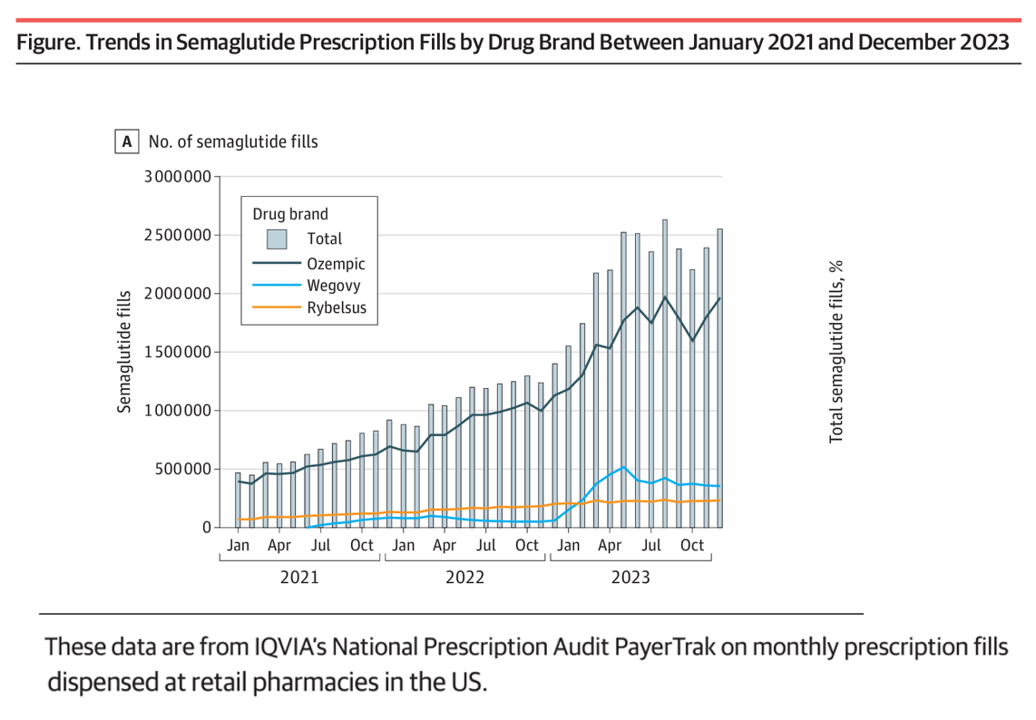
With 70 different clinical trials for GLP-1 drugs in process with the FDA, payers — and other stakeholders in the health care ecosystem — have the semaglutide-SENSE top of mind, based on my ongoing updating of this fast-moving market space. For overall market context on pace-of-growth in adoption, check out this chart from a JAMA Health Forum research letter on Prescription Fills for Semaglutide Products by Payment Method, published August 2nd. The study was based on the IQVIA National Prescription Audit PayerTrak data which captures 92% of Rx’s filled at retail pharmacies in
What’s Expected to Drive Up Health Plan Costs in 2025: GLP-1s, Behavioral Health, and Inflationary Pressures for Hospitals and Doctors – PwC’s Behind the Numbers 2025
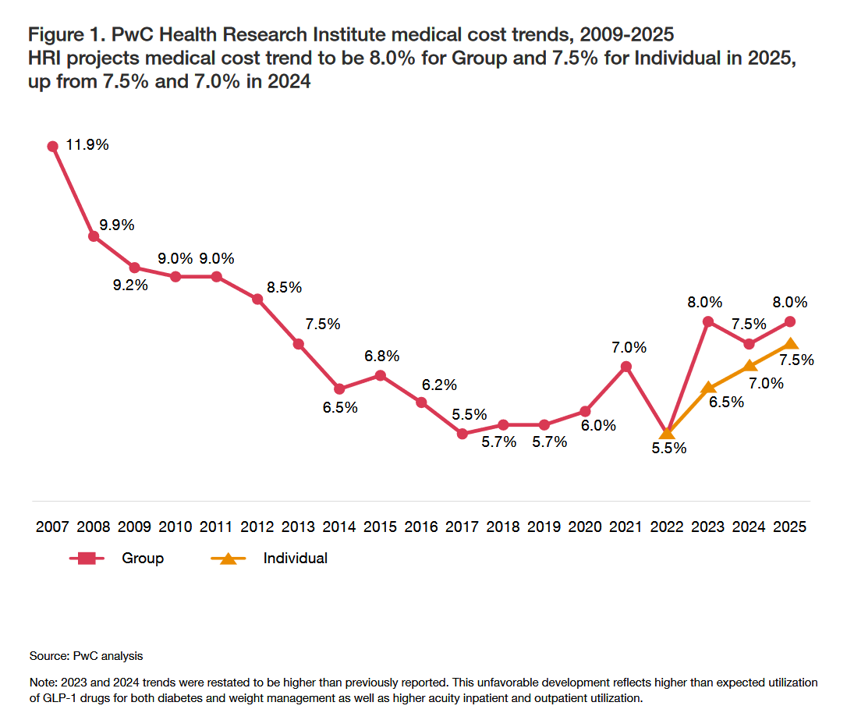
The U.S. Bureau of Labor Statistics had good news for American consumers long-facing inflation for household spending over the past couple of years, announcing on July 11, 2024, that the general consumer price index (CPI) fell, lowering real prices for people buying airline tickets, used cars and trucks, communication, and petrol to fill auto tanks. That positive economic news did not extend to medical care and personal care, the BLS reported, whose costs increased by 3.3% and 3.2%, respectively. (Motor vehicle insurance costs grew a whopping 19.5% in the report, FYI). Following the
Financial Strain Among Older People in America, and What Project 2025 Could Mean for Their Well-Being
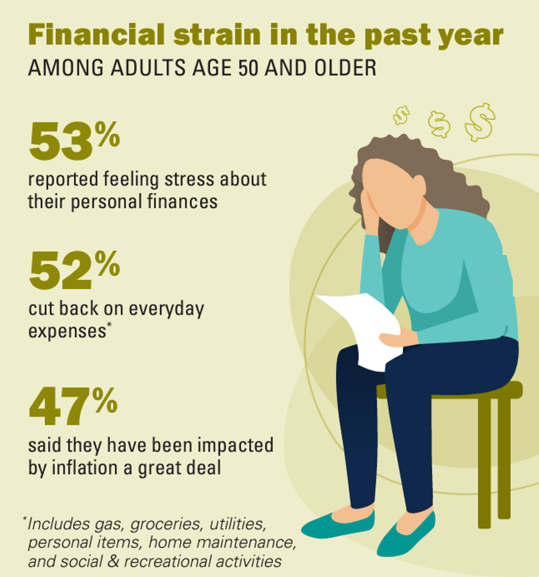
Over one-half of people 50 years of age and older in the U.S. have felt financial strain in the past year, resulting in 1 in 2 folks cutting back on everyday expenses like groceries and gas. We learn that nearly one-half of people 50 and over say they’ve been impacted by inflation “a great deal” in Making Ends Meet: Financial Strain and Well-Being Among Older Adults, the latest report from the Institute for Healthcare Policy and Innovation’s National Poll on Healthy Aging based at the University of Michigan (my alma mater). The poll was conducted by NORC at the University
Medical Debt, Aflac on Eroding Health Benefits, the CBO’s Uninsured Forecast & Who Pays for Rising Health Care Prices: A Health Consumer Financial Update
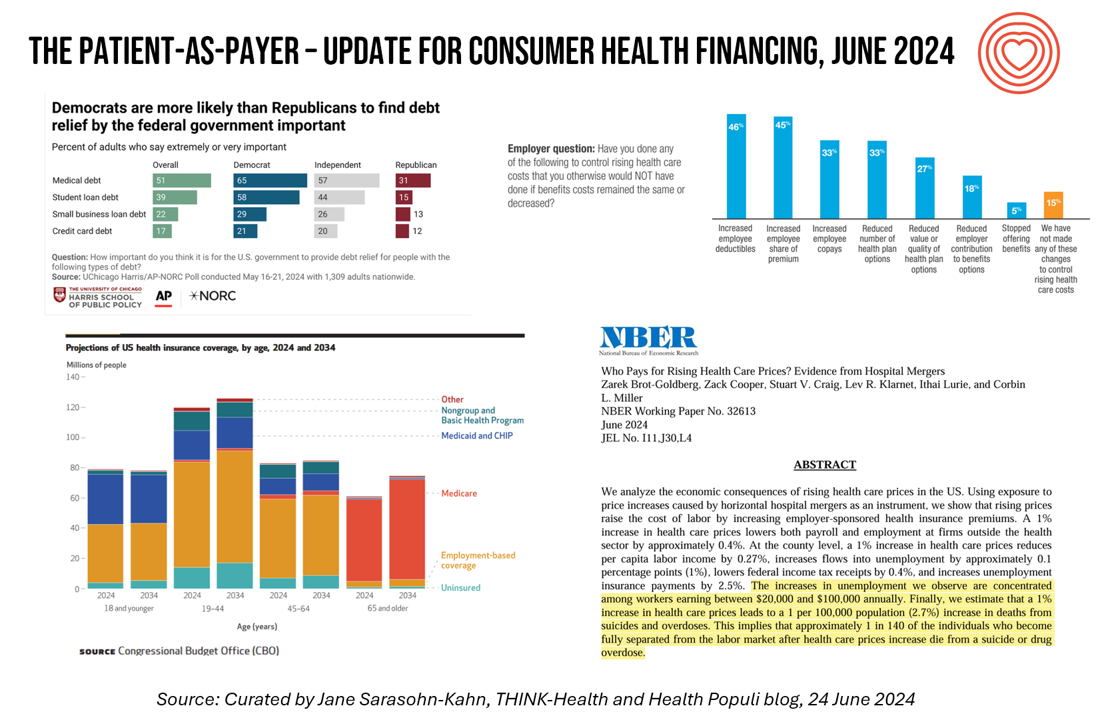
On June 11, Rohit Chopra, the Director of the Consumer Financial Protection Bureau (CFPB) announced the agency’s vision to ban Americans’ medical debt from credit reports. He called out that, “In recent years, however, medical bills became the most common collection item on credit reports. Research from the Consumer Financial Protection Bureau in 2022 showed that medical collections tradelines appeared on 43 million credit reports, and that 58 percent of bills that were in collections and on people’s credit records were medical bills.” Chopra further explained that medical debt on a consumer credit report was quite different than other kinds
Most Americans, Both Younger and Older, Worry About the Future of Medicare and Social Security
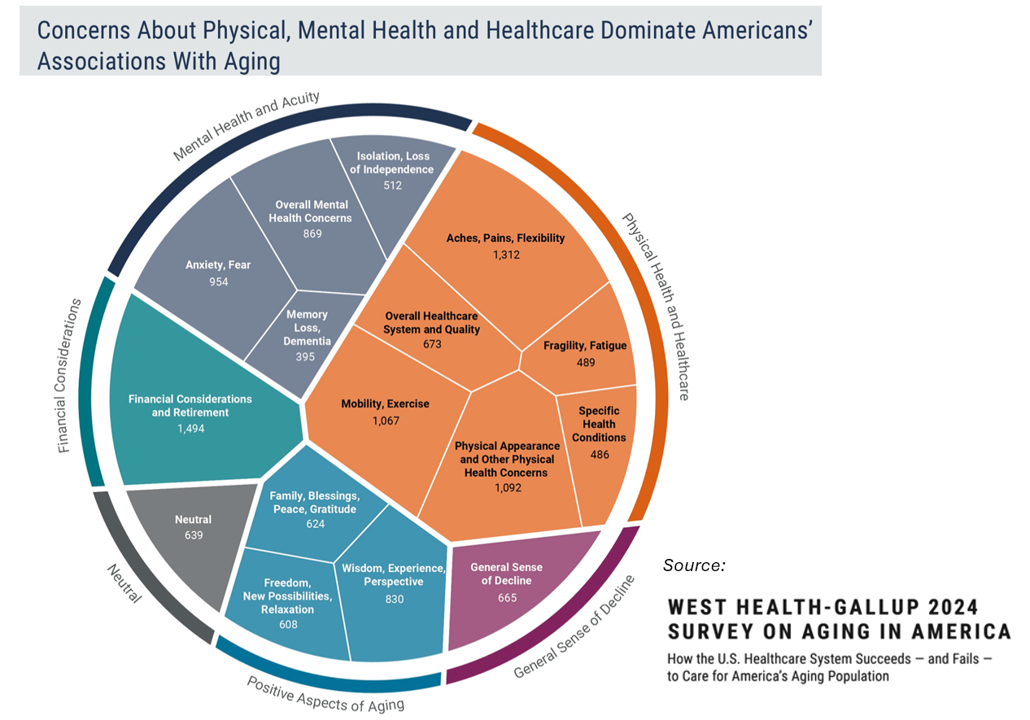
You would assume that most people over 50 would be worried about the financial future of Medicare to cover health care as those middle-aged Americans age. But a surprising two-thirds of young Americans between 18 and 29, and 7 in 10 between 30 and 39 years of age, are concerned that Medicare’s solvency will worsen leading to their not being able to receive Medicare when eligible to receive it, discovered in the 2024 Healthcare in America Report from West Health and Gallup. This year’s research focused on aging in America, exploring areas of U.S. health care system successes as well
The Thematic Roadmap for AHIP 2024: What the Health Insurance Conference Will Cover

Health insurance plans make mainstream media news every week, whether coverage deals with the cost of a plan, the cost of out-of-network care, prior authorizations, or cybersecurity and ransomware attacks, among other front-page issues. This week, AHIP (the acronym for the industry association of America’s Health Insurance Plans) is convening in Las Vegas for its largest annual 2024 meeting. We expect at least 2,400 attendees registered for the meeting, and they’ll not just be representing the health insurance industry itself; folks will attend #AHIP2024 from other industry segments including pharmaceuticals, technology, hospitals and health systems, and the investment and financial services
Health Information Security – My Interview with Richard Kaufmann, CISO of Amedisys – Part 2: Bit by Bit, Putting It Together – Planning, Implementing, Pivoting
Welcome to post #2 of 3, publishing the results of three dialogue sessions between Richard Kaufmann, CISO of Amedisys, and me. The timing of our conversations, tracking both Richard’s and the company’s evolving approach to cybersecurity in health care, has coincided with the Change Healthcare breach and ransom that emerged in February 2024. This second blog of the three is being edited just days after Andrew Witty’s testimony to the U.S. Senate Finance Committee which convened a hearing on May 1st themed, “Hacking America’s Health Care: Assessing the Change Healthcare Cyber Attack and What’s Next.” UnitedHealth Group acquired Change Healthcare
Most Older People Want to Age in Place and Are Adopting Technologies At Home To Do So

The vast majority of older people (95%) want to “age in place” — that is, stay put in their homes and avoid moving into long-term care residences or elsewhere. One approach for enabling aging-in-place is peoples’ adoption of various technologies, a topic surveyed by U.S. News & World Report. In April 2024, U.S. News interviewed 1,500 U.S. adults ages 55 and over on their views toward technology and everyday life at home. The first graphic from U.S. News’ study report, published earlier this month, shows that older people identified six categories of
The Cost of Medical Care, Long-Term Care, and Prescription Drugs Top Older Americans’ Health-Related Concerns – With Social Security and Medicare Top of Mind
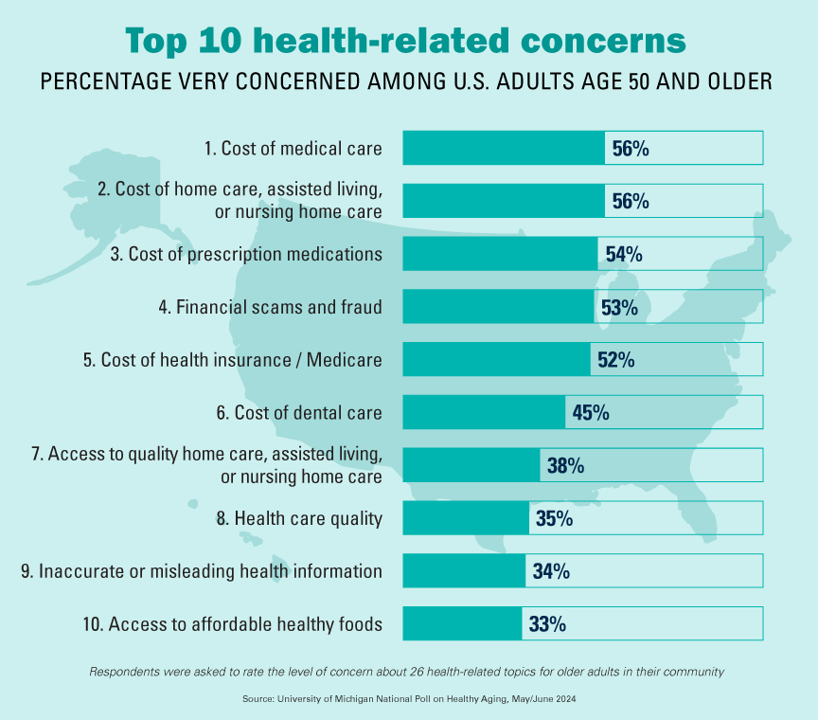
Among Americans 50 years of age and over, the top health-related concerns are Cost, Cost, and Cost — for medical services, for long-term and home care, and for prescription medications. Quality of care ranks lower as a concern versus the financial aspects of health care in America among people 50 years of age and older, as we learn what’s On Their Minds: Older Adults’ Top Health-Related Concerns from the University of Michigan Institute for Healthcare Policy and Innovation. AARP sponsors this study, which is published nearly every month of the year on the Michigan Medicine portal.
The Economic Contours of the Change Healthcare Cyber Attack: Taking Stock So Far

On February 22, 2024, I went to a CVS Pharmacy-Inside-Target in my community to fill a prescription for benzonatate 200 mg capsules. I had caught a bad case of the flu the week before, and subsequently suffered a very long tail of a cough. That’s TMI for me to write about in the Health Populi blog, but this story has a current-events twist: the pharmacist could not electronically link with my insurance company to transact my payment. He tried a few work-flows, and ended up using a discount card which in the moment worked for us, and I paid the
Hospital at Home: Prospects and Challenges, and Learnings from Best Buy Health
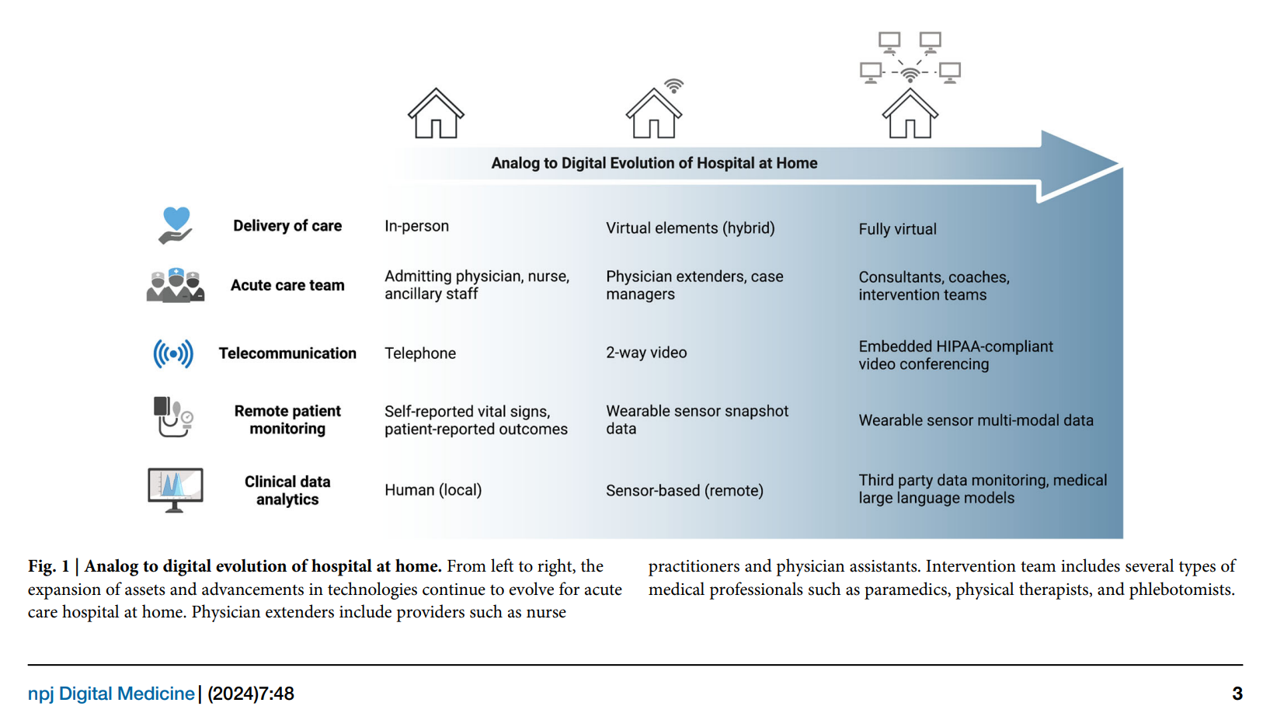
With the urgent need to identify more efficient and lower-cost health care delivery models, we look to growing evidence for digital health technologies that support the Hospital at Home (HaH) model, considered in a new review article published in late February in npj Digital Medicine, The hospital at home in the USA: current status and future prospects. Clinicians from Scripps Research and Johns Hopkins School of Medicine collaborated on this work, calling out the relatively fast adoption of HaH programs during the peak of the COVID-19 pandemic. In some parts of the world, such as Australia and Norway, “in-person at-home
From Evolution to Innovation, from Health Care to Health: How Health Plans With Collaborators Are Re-Defining the Industry
As a constant observer and advisor across the health/care ecosystem, for me the concept of a “health plan” in the U.S. is getting fuzzier by the day. Furthermore, health plan members now see themselves as medical bill payers, seeking value and consumer-level services for their health insurance premium investment. Weaving these ideas together is my mission in preparing a session to deliver at the upcoming AHIP 2024 conference in June, I’m thinking a lot about the evolving nature of health insurance, plans, and the organizations that provide them. To help me define first principles, I turned to the American father
Inflation and the cost of health care top U.S. voters’ issues for 2024 elections
The cost of living ranks top in U.S. voters’ minds among many issues Americans are feeling and following in late 2023. A close second in line is affordability of health care, as consumers’ household budgets must make room for paying medical bills — with prescription drug costs also very important as a discussion topic for 2024 Presidential candidates, we learn from the latest KFF Health Tracking Poll published 1 December. The monthly study focused on U.S. voters’ top issues and perspectives on the health system and care approaching the new year of 2024. KFF fielded the study among 1,301 U.S.
“My Doctor’s Office” Should Accept Wearable Tech Health Data, Most Patients Say

“Do personal health trackers belong in the doctor’s office?” Software Advice wondered. “Yes,” the company’s latest consumer survey found, details of which are discussed in a report published on their website. Unique to this study is the patient sample polled: Software Advice surveyed 876 patients in September 2023 to gauge their perspectives on wearable tech and health. Note that the patient sample was limited to consumers who had seen a health care provider in the past two years and who also owned and used a personal wearable health device such as an Apple Watch or Fitbit. Thus, the responses shared
Don’t Mess with Medicare and Medicaid, Washington: They Remain Popular with Americans Across Party ID
A majority of the U.S. public does not want politicians to “up-end” government-funded health programs, according to the Kaiser Family Foundation’s March 2023 Health Tracking Poll. Social Security, Medicare, and Medicaid all garner most partisans’ support whether identifying as Democrat, Independent, or Republican, KFF found in their monthly poll of U.S. voters ages 18 and over. The survey was conducted online and by telephone among 1,271 U.S. adults between March 14-23, 2023. Among all the important findings in this well-timed poll, I’ll point to the issue of public
Health in the 2022 U.S. Midterm Elections – Women, Prescription Drugs, and Who Shows Up to Vote

On Tuesday November 8, 2022, health and medical issues will be on many U.S. voters’ minds as they enter voting booths to select representatives for the House and the Senate, along with some states’ ballots addressing specific healthcare issues. Health policy experts from Manatt, Phelps & Phillips, AARP, and the United States of Care recently shared perspectives on the health care issues on voters’ and policy makers’ minds for the 2022 midterm elections. This post synthesizes their analyses as we lead up to what will be a pivotal election for Americans’ public health, individual well-being, and access to care.
The Retail Health Battle Royale in the U.S. – A Week-Long Brainstorm, Day 2 of 5 – Amazon and One Medical

Today we review the various viewpoints on Amazon’s announced acquisition of One Medical (ONEM, aka 1life Healthcare) which has been a huge story in both health care trade publications, business news, and mainstream media outlets. Welcome to Day 2 of The Retail Health Battle Royale in the U.S., my week-long update of the American retail health/care ecosystem weaving the latest updates from the market and implications and import for health care consumers. The deal was announced on 21 July, with Amazon striking the price at about $3.9 billion. Goldman Sachs and Morgan Stanley put the deal together,
The Old Gays Working with Walgreens on TikTok: Breaking Down Stereotypes and Having Fun with Health

How much do I love this media campaign from Walgreens, collaborating with the foursome The Old Gays who have a growing multi-million person fan base on TikTok? How much? A whole lot! Kudos to Walgreens for creating engaging, informative, and fun! content to learn about how people can benefit from using the company’s app ….for, Ordering prescriptions (90-day supply) Receiving delivery same-day 24/7 pharmacy chat on pricing, prescription drug information, and medications. The plotline kicks off with 3 of the 4 quartet (Jessay Martin, Robert Reeves and Mick Peterson) looking for their friend Bill Lyons, who is missing from their
What If Costco Designed the Prescription Drugs Sales Model?
The good news about prescription drugs, in the context of medical spending in the U.S., is that 9 in 10 medicines prescribed are generics. They comprise only 3% of all U.S. healthcare spending. But there’s bad news about prescription drugs in the context of medical spending in America. U.S. Consumers Overpay for Generic Drugs, a new paper from the Leonard Schaeffer Center for Health Policy & Economics asserts, with recommendations to address the intermediaries who benefit from the way Americans currently pay for medicines. Generics are “an American success story,” the authors call out, bringing
The Health of Older Americans in 2022 – Risks from the Pandemic, Isolation, and Social Determinants
For millions of older people in America, health and well-being got worse in the wake of the COVID-19 pandemic. Physical, mental and behavioral health took hits, depending on one’s living situation, social determinants of health risks, and even health plan, I write in the Medecision Liberate Health blog. In this essay on health disparities and equity for older adults, I weave together new data from, The United Health Foundation’s study on seniors’ health status in America’s Health Rankings for 2022 RAND and CMS research into seniors health disparities among Medicare Advantage
Health Care Costs At Retirement in 2022 Hit $315,000, Fidelity Forecasts
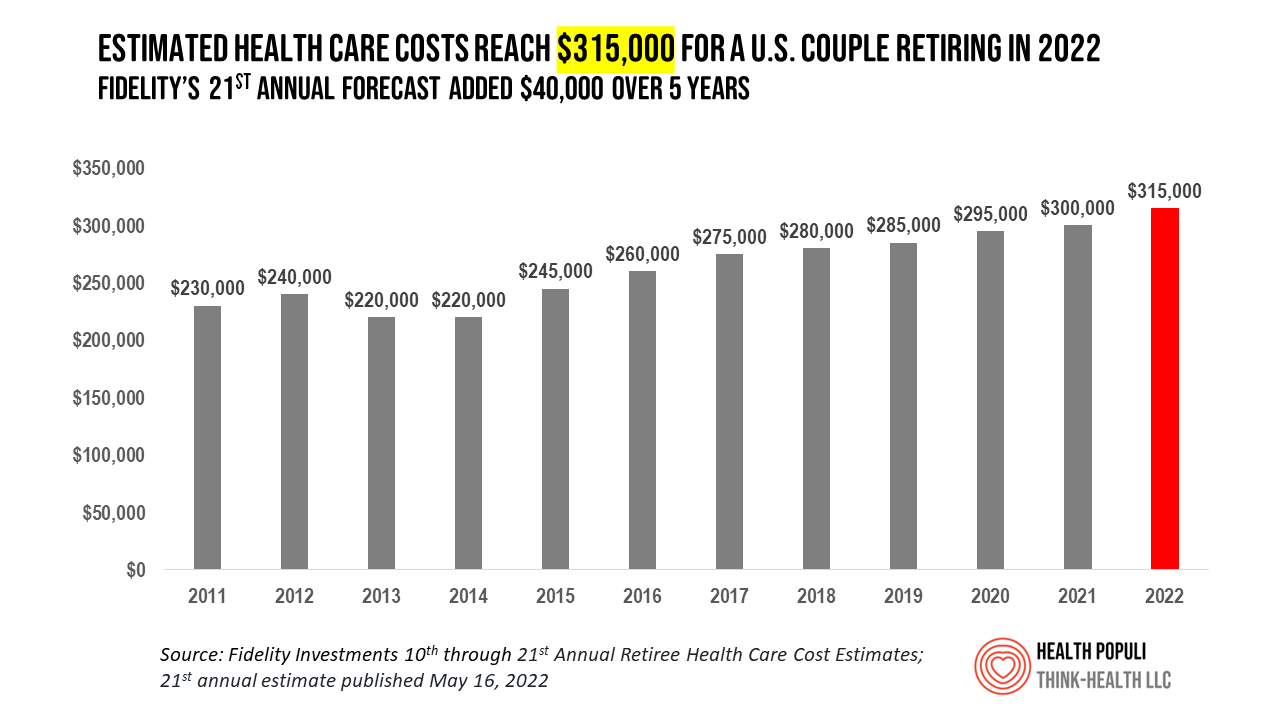
A couple retiring in 2022 should budget $315,000 to cover their health care costs in retirement, based on the 21st annual Retiree Health Care Cost Estimate from Fidelity Investments. For context, note that the median sales price of a home in the U.S. in April 2022 was $391,200. It’s important to understand what the $315,000 for “health care costs” in retirement does not cover, explained in Fidelity’s footnoted methodology: the assumption is that the hypothetical opposite-sex couple is enrolled in Original Medicare (not Medicare Advantage), and the cost estimate does not include other health-related expenses
Three in Five People 50+ in the US Will Likely Use Telehealth In the Future – An Update from AARP
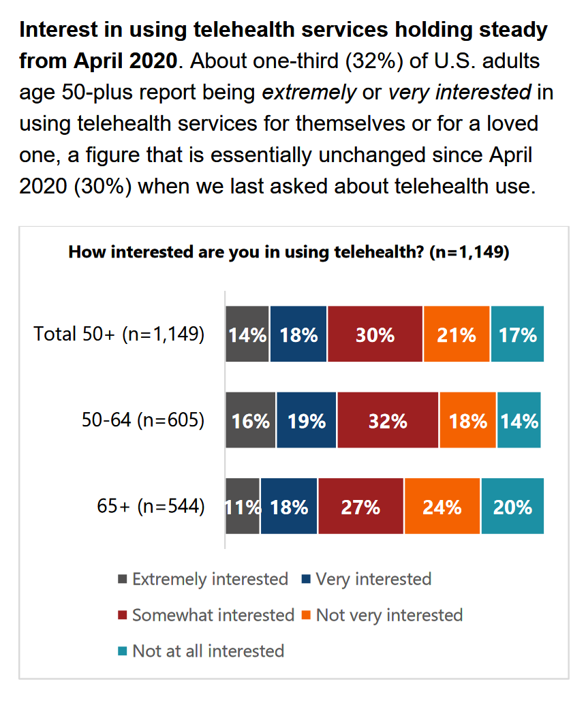
“Telehealth certainly appears to be here to stay,” the AARP forecasts in An Updated Look at Telehealth Use Among U.S. Adults 50-Plus from AARP. Two years after the emergence of the COVID-19 pandemic, one-half of U.S. adults over 50 said they or someone in their family had used telehealth. In early 2022, over half of those over 50 (the AARP core membership base) told the Association they would likely use telehealth in the future. This future expectation varies by race, the implications of which I discuss below in
Thinking About Telehealth Through the Lens of Real Estate – Listening to JLL
If you made your living in commercial real estate — and especially, working with hospitals’ and health systems’ office space — would the concept of telehealth be freaking you out right now? If you heed the words of JLL’s 2022 Patient Consumer Survey, you’d chill (at least a bit). The tagline on this paper is, “Convenience and choice drive patient decisions as new digital options take hold.” I was particularly keen to dig into this study based on its sponsoring organization: JLL is a real estate services company serving over a dozen vertical markets — including health care, life sciences,
Only 1 in 4 People Over 50 Use a Mobile Health App – And They Tend to Be Healthier and Wealthier
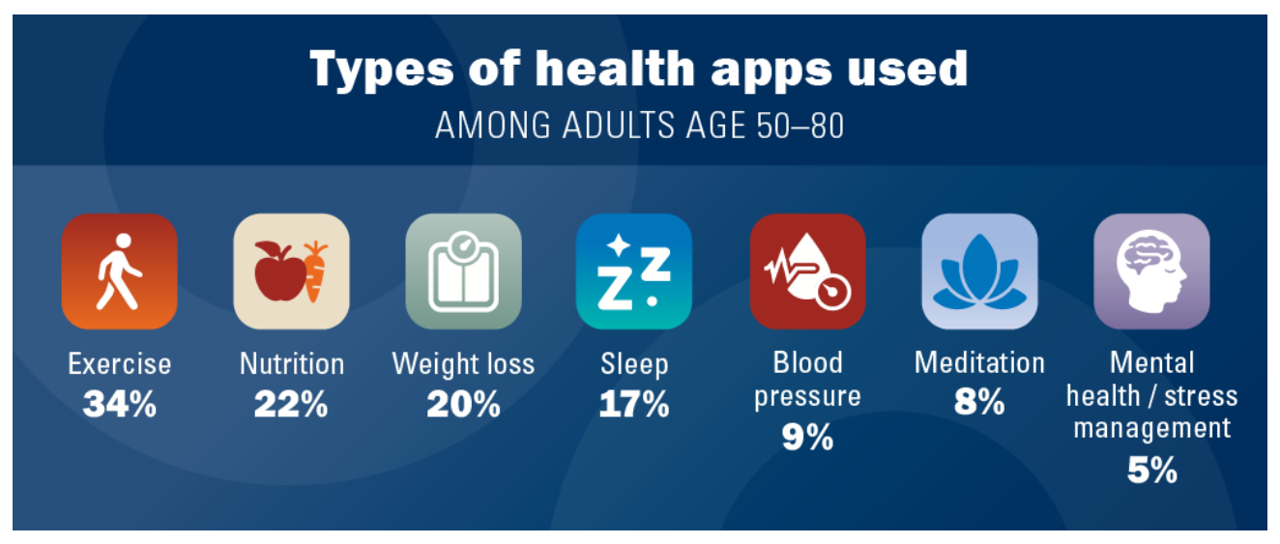
Just over 1 in 4 people over 50 in the U.S. use at least one mobile health app, and 56% of older people have never used one. Among seven mhealth tools, the most commonly-used is to track exercise. Among older people who do not use health apps, half say it is because of their lack of interest, we learn from the research in Mobile Health App Use Among Older Adults from the University of Michigan’s National Poll on Healthy Aging, sponsored by AARP. The project is part of Michigan Medicine, U-M’s med school, and directed by the Institute for Healthcare
The 2022 Health Populi TrendCast for Consumers and Health Citizens
I cannot recall a season when so many health consumer studies have been launched into my email inbox. While I have believed consumers’ health engagement has been The New Black for the bulk of my career span, the current Zeitgeist for health care consumerism reflects that futurist mantra: “”We tend to overestimate the effect of a technology in the short run and underestimate the effect in the long run,” coined by Roy Amara, past president of Institute for the Future. That well-used and timely observation is known as Amara’s Law. This feels especially apt right “now” as we enter 2022,
Fastest-Growing Brands for 2021 Are About Digital Money, Social Connections and Boomers’ Best Lives

Two pharmaceutical companies bubble up among the 20 fastest-growing brands for 2021 in Morning Consult’s report on the Fastest-Growing Brands of 2021. But the surprise in this year’s top 20 brand rankings was that five of them addressed consumers’ financial flows: Coinbase, AfterPay. Cash App, Mastercard, Chime, and Bitcoin. One year ago when I covered this study, I found that the fastest-growing brands of 2020 had everything to do with the pandemic. They dealt with home entertainment, digital connectivity, hygiene, and indeed, health (with Pfizer and AstraZeneca the two pharma brands top-of-mind for consumers). In this year’s update, exploring consumers’
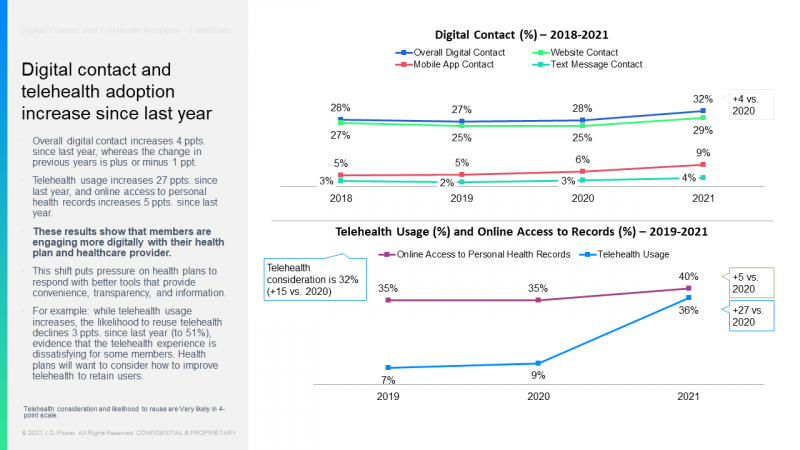
Support for Drug Price Negotiation Brings Partisans Together in the U.S.
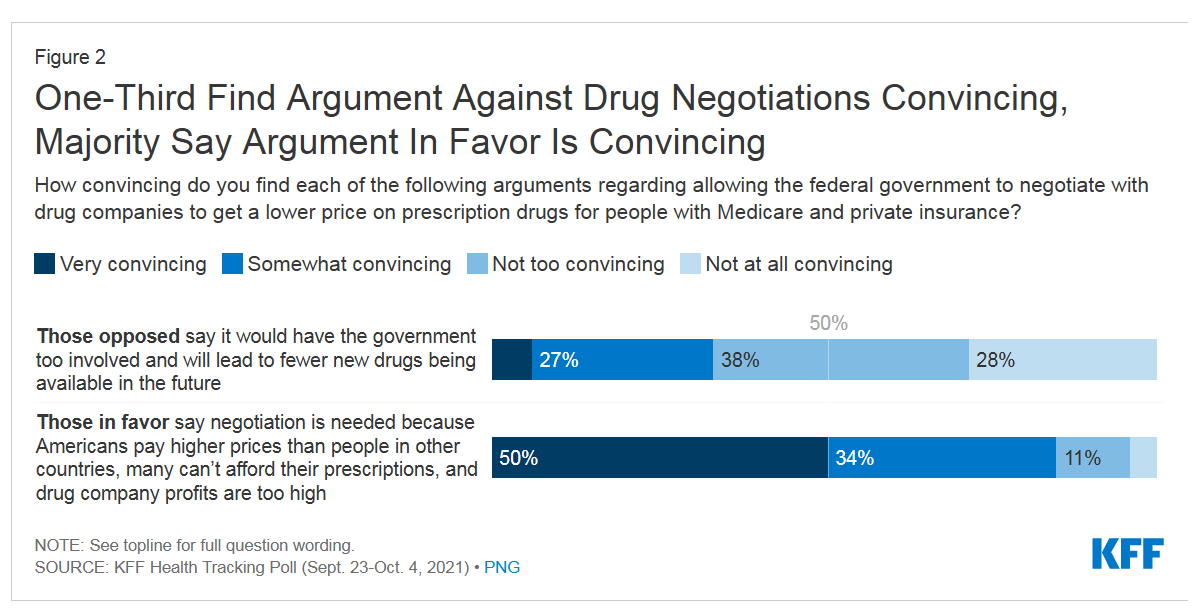
Most U.S. adults across political parties favor allowing the Federal government authority to negotiate for drug prices — even after hearing the arguments against the health policy. Drug price negotiation, say by the Medicare program, is a unifying public policy in the current era of political schisms in America, based on the findings in a special Kaiser Family Foundation (KFF) Health Tracking Poll conducted in late September-early October 2021. Overall, 4 in 5 Americans favor allowing the Federal government negotiating power for prescription drug prices, shown in the first chart from the KFF report. By party, nearly all Democrats agree
Telehealth is Health: It’s Telehealth Awareness Week

In April 2020, telemedicine morphed into mainstream medical care as hospitals and physicians risk-managed exposure to infection by meeting with patients, virtually, when possible. By March 2020, telehealth channels were replacing visits to doctors and emergency departments as shown in the first chart from the CDC’s report on the early pandemic period. By the spring of 2021, telehealth use stabilized, but health systems had built the processes and policies to deliver on the promise of omni-channel health care — from the patient’s home and hands (via smartphones) into community sites closer-to-home, and returning to brick-and-mortar medical buildings. Welcome to Telehealth
Pondering Prescription Drugs: Pricing Rx and Going Direct-to-Consumer
There is one health care public policy issue that unites U.S. voters across political party: that is the consumer-facing costs of prescription drugs. With the price of medicines in politicians’ and health citizens’ cross-hairs, the pharmaceutical and biotech industries have responded in many ways to the Rx pricing critiques from consumers (via, for example, Consumer Reports/Consumers Union and AARP), hospitals (through the American Hospital Association), and insurance companies (from AHIP, America’s Health Insurance Plans). The latest poll from the University of Chicago/Harris Public Policy and the Associate Press-NORC Center for Public Affairs Research quantifies the issue cross-party, finding that 74%
Health Insurance in Aisle 3: Why a Grocery Chain is Working on Medicare

“You can trust us to help you find the right Medicare coverage for you and your lifestyle,” the tagline reads. What kind of organization would be behind this campaign: a healthcare navigator company, an insurance company, or a social services agency? In fact, it’s a grocery store called Hy-Vee, which launched the “Medicare Aisle” to help consumers living in the eight states in which the chain’s 240+ stores operate to sort through the daunting labyrinth of Medicare choices. “Hy-Vee is a trusted leader in the health and wellness space, and as a retail and specialty pharmacy provider, we are deeply
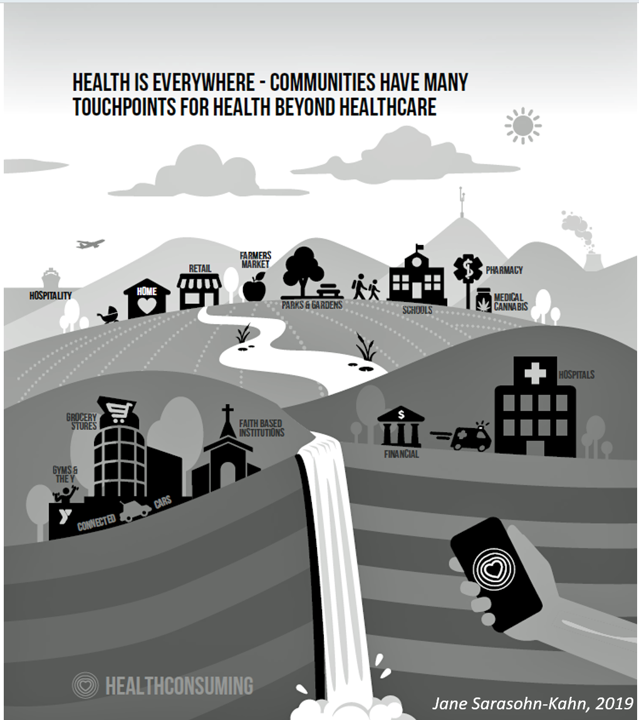
Dollar General, the Latest Retail Health Destination?

“What if…healthcare happened where we live, work, play, pray and shop, delivering the highest levels of retail experience?” I asked and answered in my book HealthConsuming: From Health Consumer to Health Citizen. The chapter called “The new retail health” began with that “what if,” and much of the book responded with the explanation of patients evolving toward health consumers and, ultimately, health citizens empowered and owning their health and care. This week, Dollar General announced the hiring of its first Chief Medical Officer, Dr. Albert Wu. With that announcement, America’s largest dollar-store chain makes clear its ambitions to join a
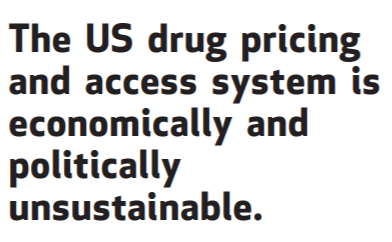
Aduhelm and Alzheimer’s Disease: A Potential Medicare Budget-Buster Puts A Blazing Light on Health Care Costs and Innovation
The FDA’s approval of the first therapy to treat Alzheimer’s Disease in over twenty years brought attention to a not-yet-convened debate of U.S. health care costs and spending, innovation, and return-on-the-investment (as well as “for whom” do the returns accrue). In my latest post for Medecision, I explore different angles on the Aduhelm and Alzheimer’s discussion, covering: The macro- and micro-economics of Alzheimer’s and the $56,000 list price for the drug The FDA regulatory process and aftermath U.S. consumers’ bipartisan support for drug price regulation through Medicare negotiation and private/commercial sector adoption Congressional legislation addressing the price of medicines in
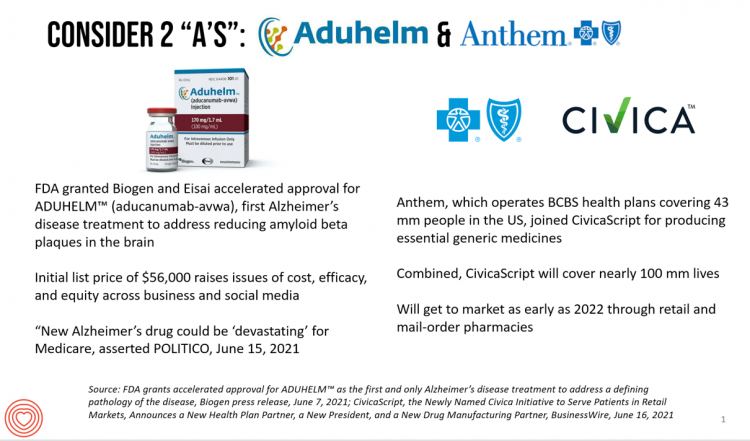
Telehealth Bolsters Patient Satisfaction (J.D. Power), and Providers Are Working to Catch Up (BDO)
Two studies published in May 2021 illustrate the value and importance of telehealth to patients in 2020, and a disconnect among many C-level executives working in hospitals, academic medical centers, and other care provider organizations. Together, the two reports from J.D. Power and BDO illustrate some mis-alignment between the demand and supply side of telehealth. On the consumer demand side, patients’ growing use of telehealth in the COVID-19 pandemic along with more frequent digital contacts with health plans bolstered member satisfaction, discovered by the J.D. Power 2021 U.S. Commercial Member Health Plan Study. J.D. Power has conducted the U.S. Commercial
What Do Democrats and Republicans Agree On? Allowing Negotiations to Lower Rx Prices
People living in the U.S. have weathered over fifteen months of life-shifts for work, school, prayer, fitness, and social lives. So you might think that the most important public priority for Congress might have something to do with COVID-19, vaccines, or health insurance coverage. But across all priorities, it turns out that prescription drug costs rank higher in Americans’ minds than any other issue in the Kaiser Family Foundation Health Tracking Poll for May 2021. Two-thirds of U.S. adults said that allowing the federal government and private insurance plans to negotiate for lower prices on Rx drugs was their top
Wearables Are Good For Older People, Too — The Latest From Laurie Orlov
The COVID-19 pandemic accelerated a whole lot of digital transformation for people staying home. For digital natives, that wasn’t such an exogenous shock. For older people who are digital immigrants, they will remember their initial Zoom get-together’s with much-missed family, ordering groceries online in the first ecommerce purchase, and using telemedicine for the first time as a digital health front-door. Laurie Orlov, tech industry veteran, writer, speaker and elder care advocate, is the founder of the encyclopedic Aging and Health Technology Watch website. She takes this propitious moment to assess The Future of Wearables and Older Adult in a new report.
The ROI on Virtual Care – Thinking About Value and Future Prospects With the AMA
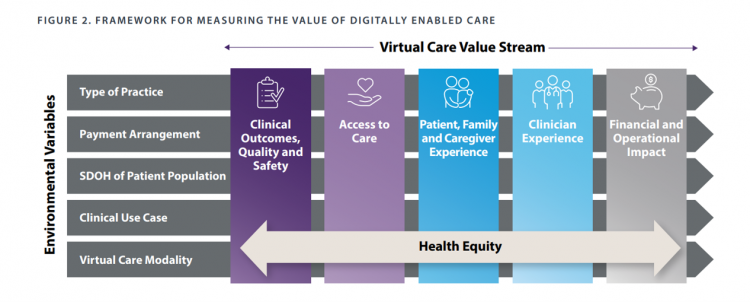
When a new technology or product starts to get used in a market, it follows a diffusion curve whose slope depends on the pace of adoption in that market. For telehealth, that S-curve has had a very long and fairly flat front-end of the “S” followed by a hockey stick trajectory in March and April 2020 as the COVID-19 pandemic was an exogenous shock to in-person health care delivery. The first chart from the CDC illustrates that dramatic growth in the use of telehealth ratcheting up since the first case of COVID-19 was diagnosed in the U.S. Virtual care has
Health Care Costs for a Couple in Retirement in the U.S. Reach $300,000
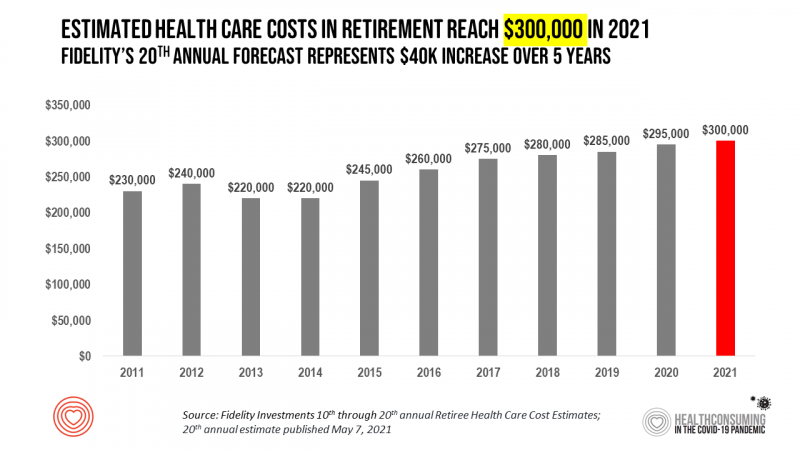
To pay for health care expenses, the average nest-egg required for a couple retiring in the U.S. in 2021 will be $300,000 according to the 20th annual Fidelity Investments Retiree Health Care Cost Estimate. I’ve tracked this survey for over a decade here on Health Populi, and updated the annual chart shown here to reflect a $40,000 increase in retiree costs since 2016. While the rate of increase year-on-year since then has slowed, the $300,000 price-tag for retiree health care costs is a huge number few Americans have saved for. That $300K splits up unequally for an opposite-gender couple (in
The Cost of Healthcare Can Drive Medical Rationing and Crowd Out Other Household Spending
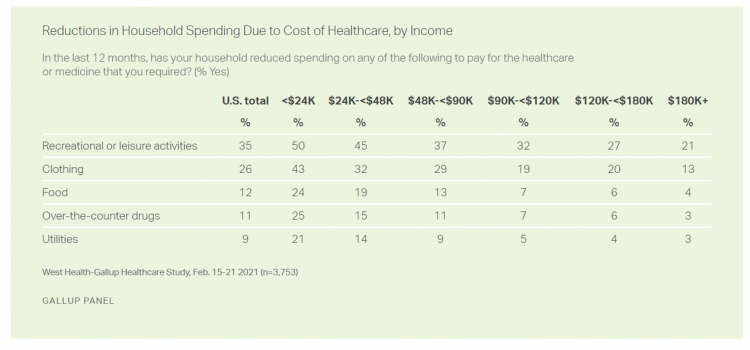
One in five people in the U.S. cannot afford to pay for quality health care — an especially acute challenge for Black and Hispanic Americans, according to a West Health-Gallup poll conducted in March 2021, a year into the COVID-19 pandemic. “The cost of healthcare and its potential ramifications continues to serve as a burdensome part of day-to-day life for millions of Americans,” the study summary observed. Furthermore, “These realities can spill over into other health issues, such as delays in diagnoses of new cancer and associated treatments that are due to forgoing needed care,” the researchers expected. The first table
Housing as Prescription for Health/Care – in Medecision Liberation

COVID-19 ushered in the era of our homes as safe havens for work, shopping, education, fitness-awaking, bread-baking, and health-making. In my latest essay written for Medecision, I weave together new and important data and evidence supporting the basic social determinant of health — shelter, housing, home — and some innovations supporting housing-as-medicine from CVS Health, UnitedHealth Group, AHIP, Brookings Institution, the Urban Land Institute, and other stakeholders learning how housing underpins our health — physical, mental, financial. Read about a wonderful development from Communidad Partners, working with the Veritas Impact Partners group, channeling telehealth to housing programs serving residents with
Value-Based Health Care Needs All Stakeholders at the Table – Especially the Patient

2021 is the 20th anniversary of the University of Michigan Center for Value-Based Insurance Design (V-BID). On March 10th, V-BID held its annual Summit, celebrating the Center’s 20 years of innovation and scholarship. The Center is led by Dr. Mark Fendrick, and has an active and innovative advisory board. [Note: I may be biased as a University of Michigan graduate of both the School of Public Health and Rackham School of Graduate Studies in Economics]. Some of the most important areas of the Center’s impact include initiatives addressing low-value care, waste in U.S. health care, patient assistance programs, Medicare
The Digital Transformation of Home for Health – Brainstorming with Karsten Russell-Wood of Philips

At the start of CES 2021, I had the opportunity to catch up with Karsten Russell-Wood, Portfolio Marketing Leader, Post Acute & Home, Connected Care at Philips. We brainstormed just as CES 2021 was going to “open,” virtually, for the consumer electronics conference’s first all-virtual meeting. Philips, a longtime major exhibitor at CES, created an entirely new online experience for the CES attendees – a sort of virtual gallery of different exhibits that are accessed from a single point in a “room” with various entry points. One of the company’s key messages for CES 2021 was health care delivered outside
The 2021 Health Populi TrendCast – Health Care, Self-Care, and the Rebirth of Love in Public Health

In numerology, the symbolic meaning behind the number “21” is death and re-birth. In tarot cards, 21 is a promise of fulfillment, triumph, and victory. How apropos that feels right now as we say goodbye and good riddance to 2020 and turn the page for a kinder, gentler, healthier New Year. It would be sinful to enter a New Year as challenging as 2021 promises to be without taking the many lessons of our 2020 pandemic life and pain into account. For health care in America, it is a time to re-build and re-imagine a better, more equitable landscape for
Home Is the Health Hub for Older People – Learning from Laurie Orlov
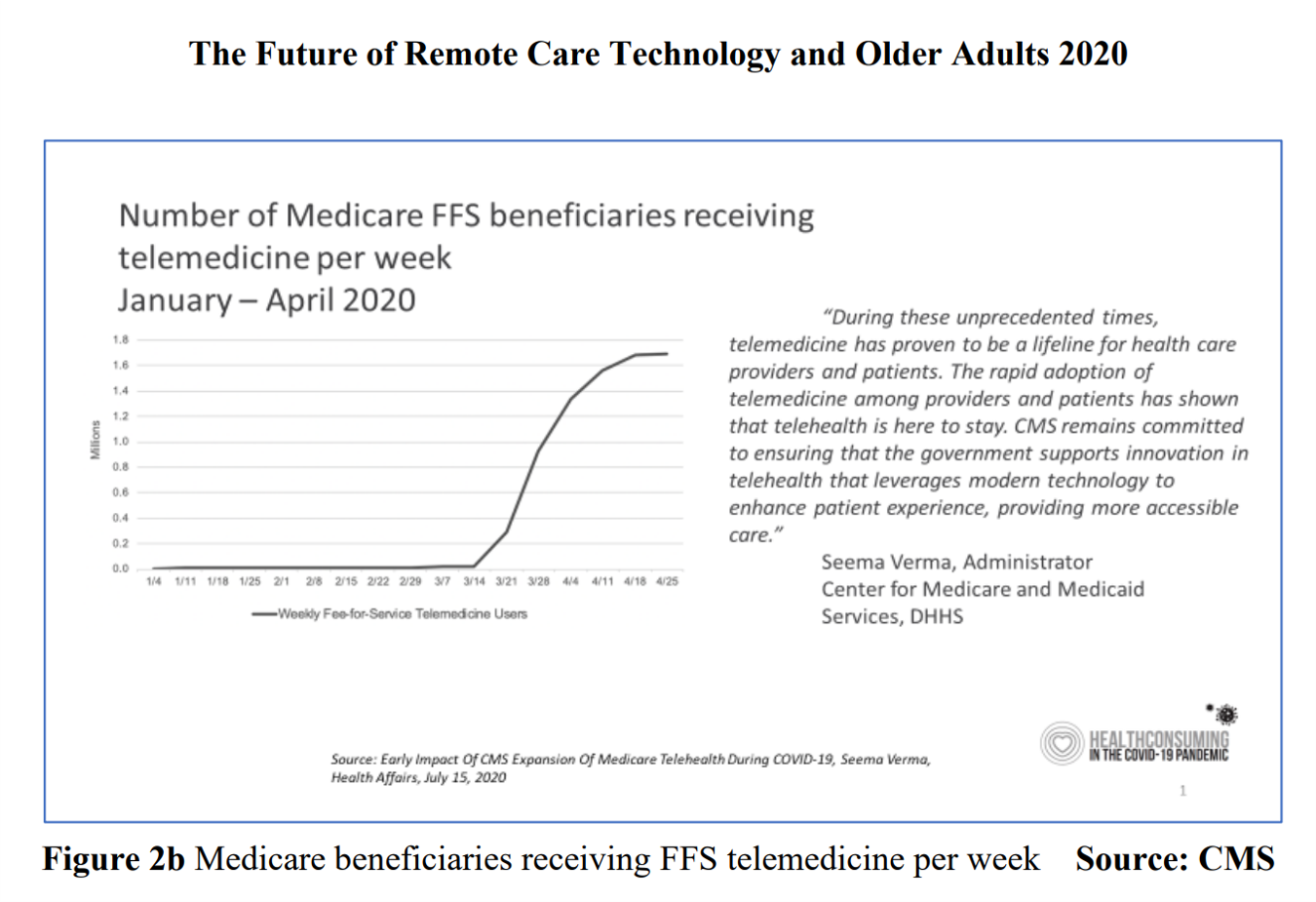
By April 2020, over one million Medicare members were receiving health care via telemedicine. The graph here shows you the hockey-stick growth for virtual care use by older Americans into the second month of the coronavirus pandemic. The COVID-19 public health crisis up-ended all aspects of daily living in America for people of all ages. For older Americans, avoiding the risk of contracting the tricky virus in public, and especially, in health care settings, became Job 1. The pandemic thus nudged older people toward adopting digital lifestyles for daily life, for shopping, for praying, and indeed, for health care. Laurie
Telehealth Use Among Older Americans: Growing Interest, Remaining Concerns
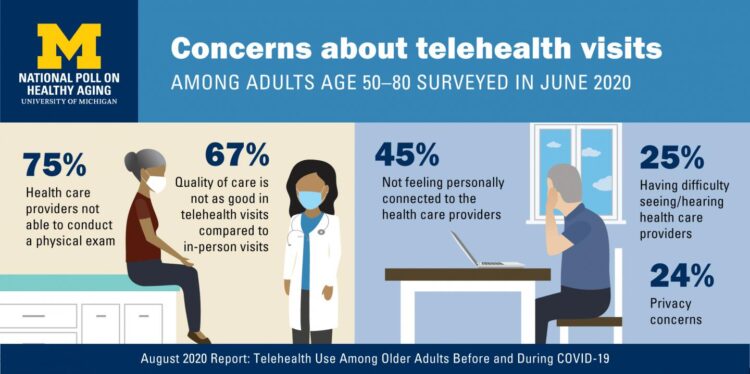
In the Fear of Going Out Era spawned by the COVID-19 pandemic, many patients were loath to go to the doctor’s office for medical care, and even less keen on entering a hospital clinic’s doors. This drove health consumers to virtual care platforms in the first months of the public health crisis — including lots of older people who had never used telemedicine or even a mobile health app. In the August 2020 National Poll on Heathy Aging, the University of Michigan research team found a 26% increase in telehealth visits from 2019 to 2020, March to June 2020 year-over-year.
The Median Hospital Charge In the U.S. for COVID-19 Care Ranges From $34-45K
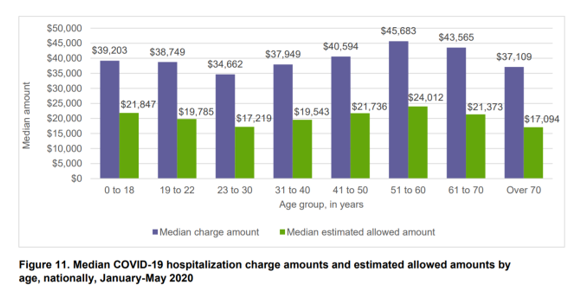
The median charge for hospitalizing a patient with COVID-19 ranged from $34,662 for people 23 to 30, and $45,683 for people between 51 and 60 years of age, according to FAIR Health’s research brief, Key Characteristics of COVID-19 Patients published July 14th, 2020. FAIR Health based these numbers on private insurance claims associated with COVID-19 diagnoses, evaluating patient demographics (age, gender, geography), hospital charges and estimated allowed amounts, and patient comorbidities. They used two ICD-10-CM diagnostic codes for this research: U07.1, 2019-nCoV acute respiratory disease; and, B97.29, other coronavirus as the cause of disease classified elsewhere which was the original code
Most Virtual Care Consumers, Satisfied With Visits in the COVID Era, Expect It for Future Care
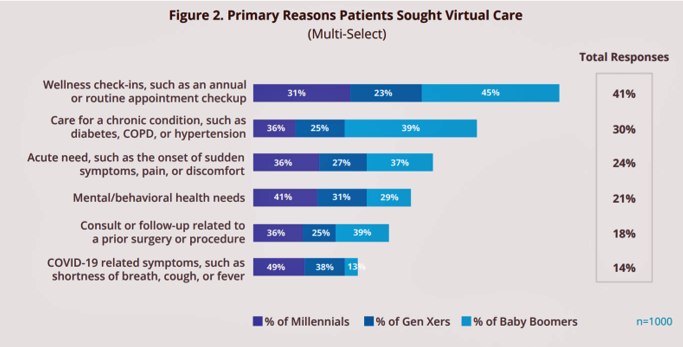
Within days of the coronavirus pandemic emerging in the U.S., health care providers set up virtual care arrangements to convene with patients. Three months into the COVID-19 crisis, how have patients felt about these telehealth visits? In Patient Perspectives on Virtual Care, Kyruus answers this question based on an online survey of 1,000 patients 18 years of age and older, conducted in May 2020. Each of these health consumers had at least one virtual care visit between February and May 2020. The key findings were that: Engaging in a virtual visit was a new-new thing for 72% of people Patients’
Americans Across Political Party Worry About Prescription Drug Prices – Especially to Deal with COVID-19
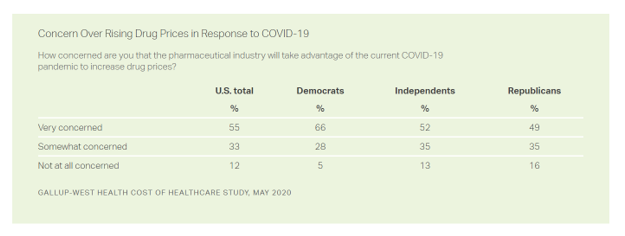
Nine in ten Americans is concerned about the price of prescription drugs in the wake of the coronavirus pandemic, Gallup and West Health found in their survey on the cost of healthcare, published today. A majority of people across political party share this concern: overall, 88% of U.S. adults are concerned about rising drug prices in response to COVID19, split across party ID with: 94% of Democrats, 86% of Independents, and 84% of Republicans. By demographics, more women than men are concerned about rising costs for the three health care spending categories the survey studied: drug prices, insurance premiums, and
Trust My Doctor and Fear the Office: The Telehealth Opportunity in and Beyond the COVID-19 Pandemic
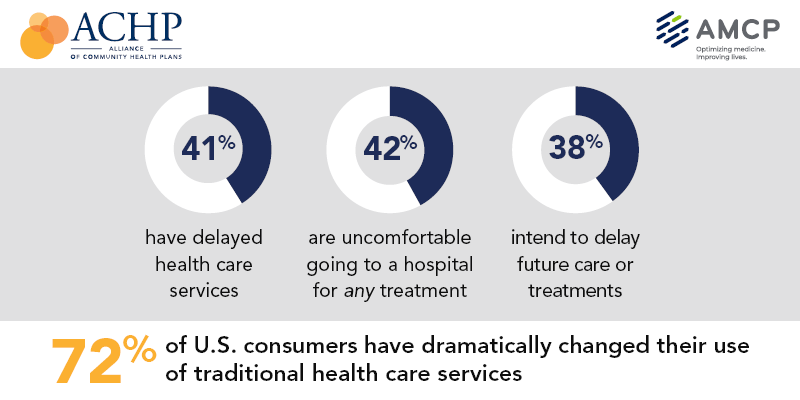
Doctors maintain their top status as U.S. patients’ most-trusted source of coronavirus information. However, as patients continue to be concerned about exposure to COVID-19, 3 in 5 are concerned about being at-risk to the virus in their doctor’s office, according to research from the Alliance of Community Health Plans (ACHP) and AMCP, the Academy of Managed Care Pharmacy. Patients’ concerns of COVID-19 risks have led them to self-ration care in the following ways: 41% have delayed health care services 42% felt uncomfortable going to a hospital for any medical treatment 45% felt uncomfortable using an urgent care or walk-in clinic,
Health Care In the COVID-19 Era – PwC Finds Self-Rationing of Care and Meds Especially for Chronic Care
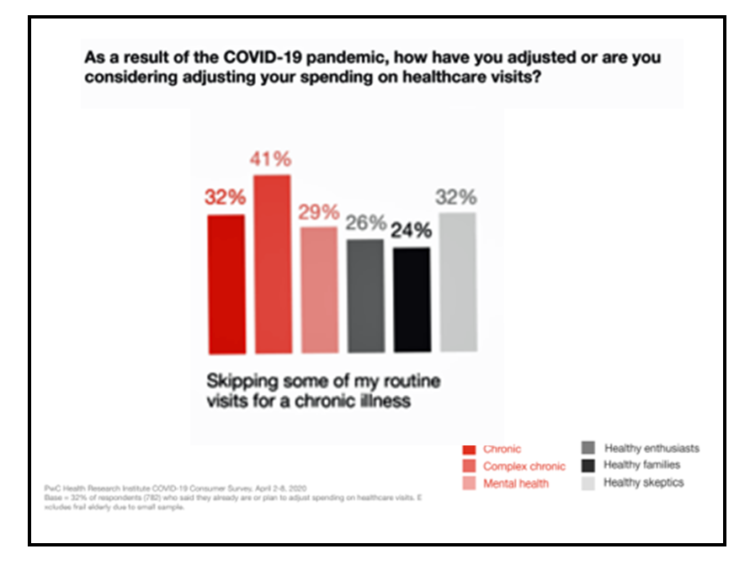
Patients in the U.S. are self-rationing care in the era of COVID-19 by cutting spending on health care visits and prescription drugs. The coronavirus pandemic’s impact on health consumers’ spending varies depending on whether the household is generally a healthy family unit, healthy “enthusiasts,” dealing with a simple or more complex chronic conditions, or managing mental health issues. PwC explored how COVID-19 is influencing consumers’ health care behaviors in survey research conducted in early April by the Health Research Institute. The findings were published in a May 2020 report, detailing study findings among 2,533 U.S. adults polled in early April
Come Together – A Health Policy Prescription from the Bipartisan Policy Center
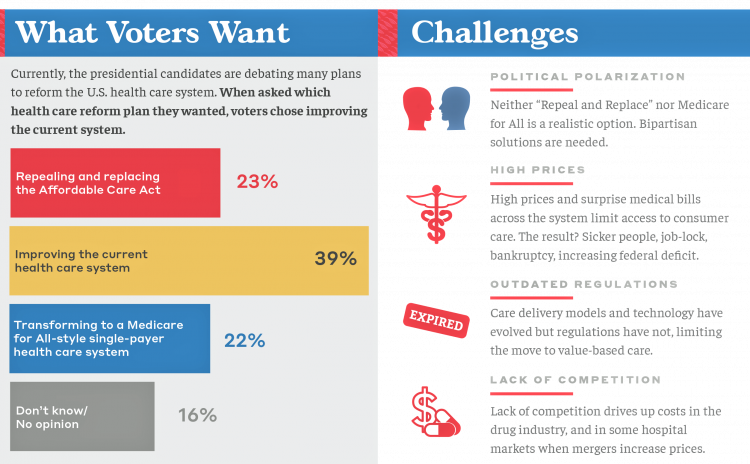
Among all Americans, the most popular approach for improving the health care in the U.S. isn’t repealing or replacing the Affordable Care Act or moving to a Medicare-for-All government-provided plan. It would be to improve the current health care system, according to the Bipartisan Policy Center’s research reported in a Bipartisan Rx for America’s Health Care. The BPC is a truly bipartisan organization, co-founded by Former Democratic Senate Majority Leaders Tom Daschle and George Mitchell, and Former Republican Senate Majority Leaders Howard Baker and Bob Dole. While this political week in America has revealed deep chasms between the Dems and
A Uniting Issue in the United States is Lowering Prescription Drug Costs
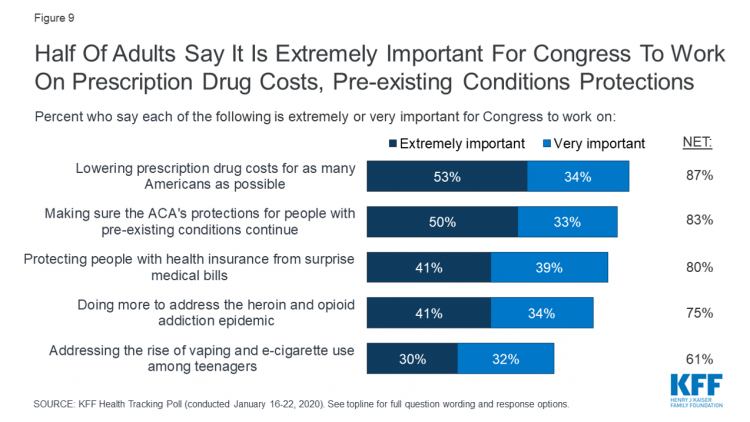
Health care continues to be the top-ranked voting issue in the U.S. looking to the November 2020 Presidential and Congressional elections. The Kaiser Family Foundation conducts the monthly poll which gauges U.S. adults’ perspectives on health care, and this month’s January 2020 Kaiser Health Tracking Poll explores Americans’ views on broad healthcare reform plans and specific medical policy issues. Overall, Americans point to prescription drug costs and the preservation of the Affordable Care Act’s protections for people with pre-existing conditions, the first chart tells us. Third and fourth on voters’ minds are protecting patients from surprise medical bills and better
Medicare Members Are Health Consumers, Too – Our AHIP Talk About Aging, Digital Immigrants, and Personalizing Health/Care
As Boomers age, they’re adopting mobile and smart technology platforms that enable people to communicate with loved ones, manage retirement investment portfolios, ask Alexa to play Frank Sinatra’s greatest hits, and manage prescription refills from the local grocery store pharmacy. Last week, the Giant Eagle grocery chain was the first pharmacy retailer to offer a new medication management skill via Alexa. That program has the potential to change our Medicare members manage meds at home to ensure better adherence, supporting better health outcomes and personal feelings of efficacy and control. [As an aside, consumers really value pharmacies embedded in grocery
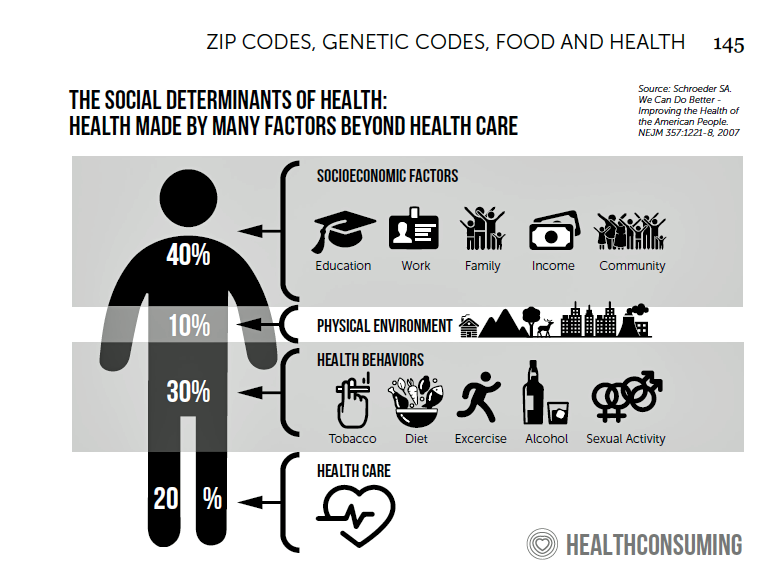
Social Determinants of Health – My Early Childhood Education and Recent Learnings, Shared at the HealthXL Global Gathering
My cousin Arlene got married in Detroit at the classic Book Cadillac Hotel on July 23, 1967, a Sunday afternoon wedding. When Daddy drove us back out to our suburban home about 30 minutes from the fancy hotel, the car radio was tuned to WWJ Newsradio 950, all news all the time. As soon as Daddy switched on the radio, we were shocked by the news of a riot breaking out in the city, fires and looting and gunshots and chaos in the Motor City. Two days later, my father, who did business with Mom-and-Pop retail store owners in the
More Evidence of Self-Rationing as Patients Morph into Healthcare Payors

Several new studies reveal that more patients are feeling and living out their role as health care payors as medical spending vies with other household line items. This role of patient-as-the-payor crosses consumers’ ages and demographics, and is heating up health care as the top political issue for the 2020 elections at both Federal and State levels. In research from HealthPocket, 2 in 5 Americans said they needed to reduce other household expenses to be able to afford their monthly insurance premiums. Four in ten consumers said their monthly health insurance premiums were increasing. One in four people in the
Thinking About Health Care One Year From the 2020 Presidential Election

Today is 4th November 2019, exactly one year to the day that Americans can express their political will and cast their vote for President of the United States. Health care will be a key issue driving people to their local polling places, so it’s an opportune moment to take the temperature on U.S. voters’ perspectives on healthcare reform. This post looks at three current polls to gauge how Americans are feeling about health care reform 365 days before the 2020 election, and one day before tomorrow’s 2019 municipal and state elections. Today’s Financial Times features a poll that found two-thirds
Will Consumers Cross the Cost-and-Trust Chasm Between Prescription Drugs and Hospitals?
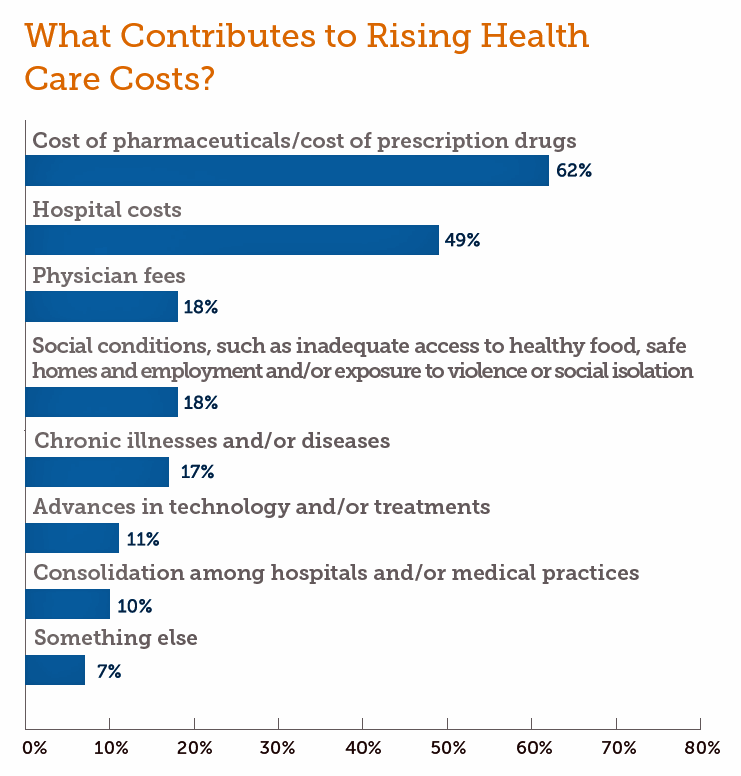
People in the U.S. rank prescription drugs, lab tests, emergency room visits, dental and vision care, preventive services, chronic disease management and mental health care as the “most essential” health care services, according to the 2019 Survey of America’s Patients conducted by The Physicians Foundation. When asked what factors contribute to rising health care costs in America, most consumers cite the cost of prescription drugs. Taken together, these two data points demonstrate the potent political import of prescription drug prices as the U.S. approaches the 2020 Presidential election. The Physicians Foundation surveyed 2,001 U.S. adults between 27 and 75 years
Patients Growing Health Consumer Muscles Expect Digital Services

Patients’ experiences with the health care industry fall short of their interactions with other industries — namely online retail, online banking and online travel, a new survey from Cedar, a payments company, learned. Survata conducted the study for Cedar among 1,607 online U.S. consumers age 18 and over in August and September 2019. These study respondents had also visited a doctor or hospital and paid a medical bill in the past year. One-third of these patients had a health care bill go to collections in the past year, according to Cedar’s 2019 U.S. Healthcare Consumer Experience Study. Among those people
Wasted: $1 of Every $4 Spent on Health Care In America
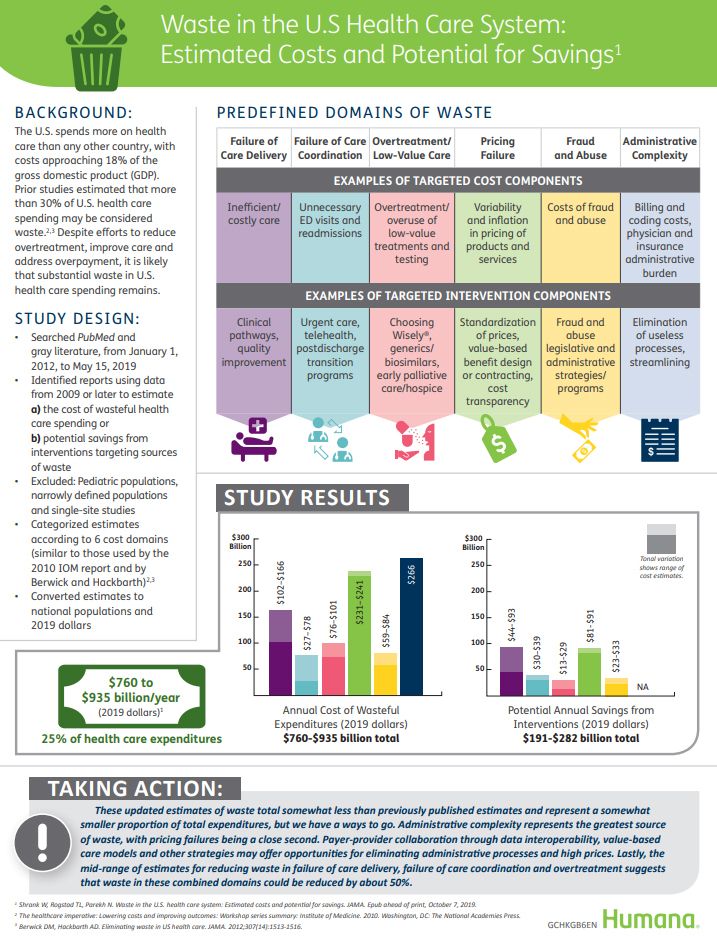
A study in JAMA published this week analyzed research reports that have measured waste in the U.S. health care system, calculating that 25% of medical spending in America is wasted. If spending is gauged at $3.8 trillion, waste amounts to nearly $1 trillion. If spending is 18% of the American gross domestic product (GDP), then some 4.5% of the U.S. economy is wasted spending by the health care system and its stakeholders. In “Waste in the US Health Care System,” a team from Humana and the Univrsity of Pittsburgh recalibrated the previous finding of 30% of wasted spending to the 25%,
The Promise of Telehealth for Older People – the U-M National Poll on Healthy Aging
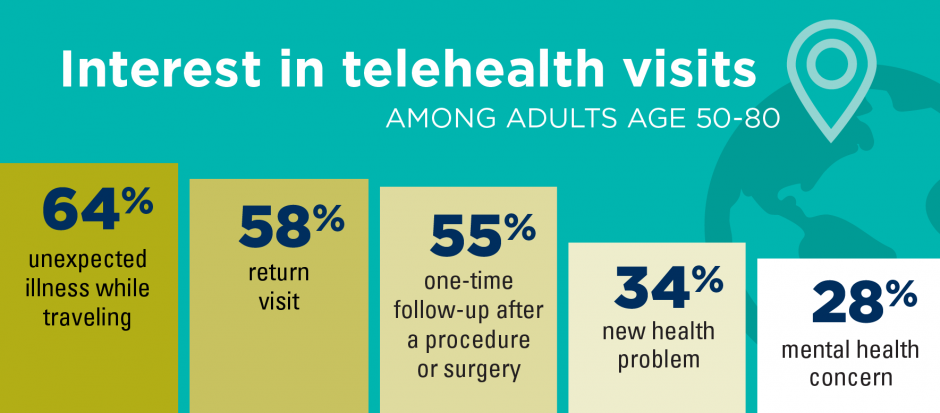
Older people are re-framing their personal images and definitions of aging, from continuing to work past typical retirement age, Skyping and texting with grandchildren, and traveling to destinations well beyond the “snowbird” locales of Florida and Arizona to more active and often charitable/volunteer situations in developing economies. And so, too, are older folks re-imagining how and where their health care services could be delivered and consumed. Most people over 50 years of age are cautious but open to receiving health care virtually via telehealth platforms, according to the National Poll on Healthy Aging from my alma mater, the University of Michigan. U-M’s
Growing Support for Medicare for All – But Do People Really Understand What It Means?
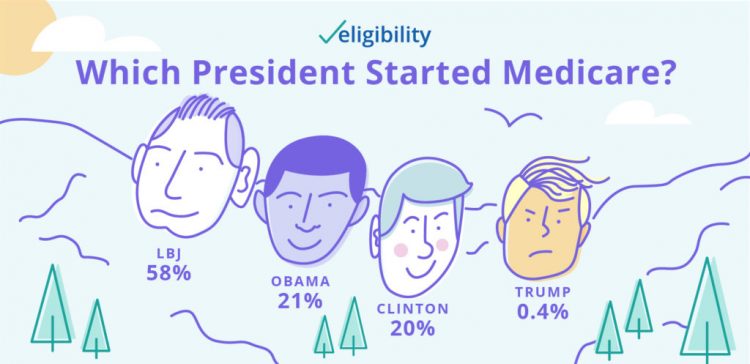
Two new data points converge that beg the question in the title of this post. These two surveys are: The Morning Consult’s poll published today finding growing support among Democratic voters for Medicare for All as the centerpiece for health reform in America; and, A recent study from Eligibility.com on “Medicare Myths Explained,” with the tagline, “How much do you know about Medicare?” Not so very much, Eligibility.com found out. Let’s start with the Morning Consult poll results, which compare support for Medicare for All from January 2019 and August 2019. The headline number from this poll is seen in
A Profile of People in Medicare Advantage Plans – HealthMine’s Survey of “Digital Immigrants”
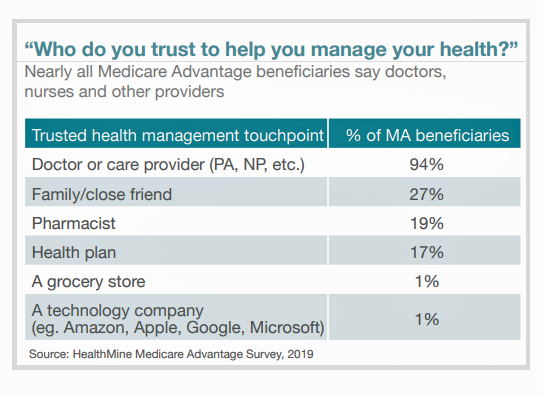
There are over 60 million enrollees in Medicare in 2019, and fully one-third are in Medicare Advantage plans. Medicare is adding 10,000 new beneficiaries every day in the U.S. Medicare Advantage enrollment is fast-growing, shown in the first chart where over 22 million people were in MA plans in January 2019. Better understanding this group of people will be critical to helping manage a fast-growing health care bill, and growing burden of chronic disease, for America. To that end, HealthMine conducted a survey among 800 people enrolled in Medicare Advantage plans ag 65 and over with at least one diagnosed
Talking “HealthConsuming” on the MM&M Podcast

Marc Iskowitz, Executive Editor of MM&M, warmly welcomed me to the Haymarket Media soundproof studio in New York City yesterday. We’d been trying to schedule meeting up to do a live podcast since February, and we finally got our mutual acts together on 6th August 2019. Here’s a link to the 30-minute conversation, where Marc combed through the over 500 endnotes from HealthConsuming‘s appendix to explore the patient as the new health care payor, the Amazon prime-ing of people, and prospects for social determinants of health to bolster medicines “beyond the pill.” https://www.pscp.tv/MMMnews/1eaJbvgovBYJX Thanks for listening — and if you
The New Drug Companies Aren’t Drug Companies At All

The health/care ecosystem continues to morph as the stakeholder groups themselves are blurring across and outside of their core businesses. Today’s example of this is Clover Health, which launched Clover Therapeutics this week. This research organization will develop medicines targeting older adults — which makes sense because Clover Health’s target consumer market is Medicare Advantage beneficiaries. “Clover Therapeutics was created to address the significant unmet needs in chronic progressive diseases in the Medicare population,” Cheng Zhang, Head of Clover Therapeutics, is quoted in the press release. The company will first collaborate with Genentech (Roche) to research and develop therapies based
Health Care and the Democratic Debates – Round 2 – Battle Royale for M4All vs Medicare for All Who Want It – What It Means for Industry

Looking at this photo of the 2020 Democratic Party Presidential candidate debater line-up might give you a déjà vu feeling, a repeat of the night-before debate. But this was Round 2 of the debate, with ten more White House aspirants sharing views — sometimes sparring — on issues of immigration, economic justice, climate change, and once again health care playing a starring role from the start of the two-hour event. The line-up from left to write included: Marianne Williamson. author and spiritual advisor John Hickenlooper, former Governor of Colorado Andrew Yang. tech company executive Pete Buttigieg, Mayor of South Bend,
Health Care and the Democratic Debates – Part 1 – Medicare For All, Rx Prices, Guns and Mental Health

Twenty Democratic Presidential candidates each have a handful of minutes to make their case for scoring the 2020 nomination, “debating” last night and tonight on major issues facing the United States. I watched every minute, iPad at the ready, taking detailed notes during the 120 minutes of political discourse conducted at breakneck speed. Lester Holt, Savannah Guthrie, and Jose Diaz-Balart asked the ten candidates questions covering guns, butter (the economy), immigration, climate change, and of course, health care — what I’m focusing on in this post, the first of two-debate-days-in-a-row. The first ten of twenty candidates in this debate were,
Talk to Me About My Health, Medicare Advantage Beneficiaries Tell J.D. Power
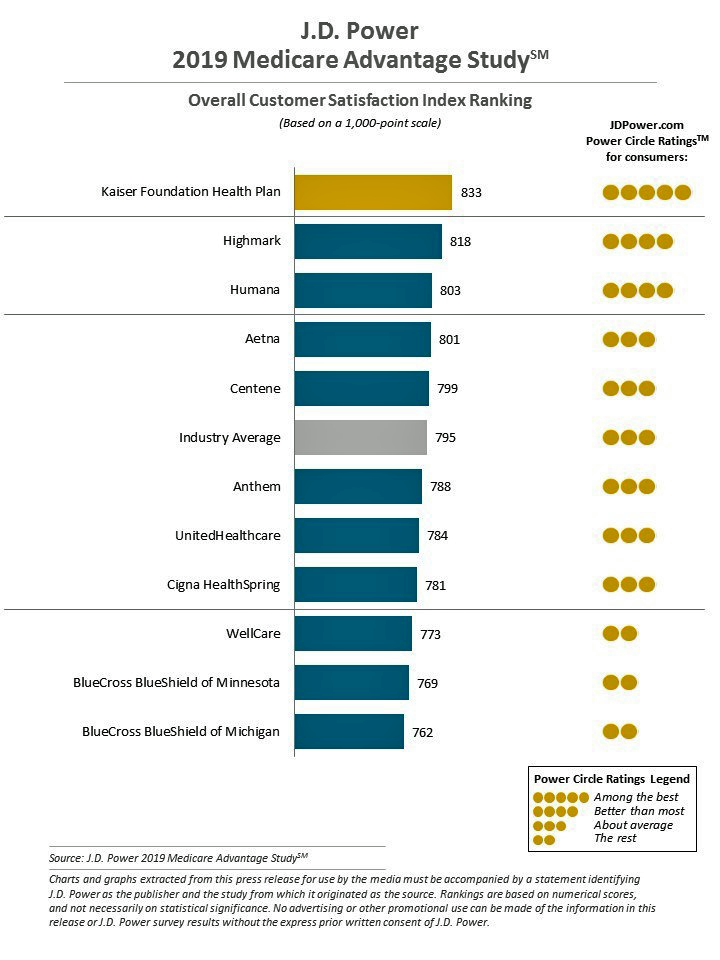
Cost is the major reason why Medicare Advantage plan beneficiaries switch plans, but people who switch also tend to have lower satisfaction scores based on non-cost factors. Those ratings have a lot to do with information and communication, according to J.D. Power’s 2019 Medicare Advantage Plan Study. The Study explores MA beneficiaries’ views on six factors: Coverage and benefits Provider choice Cost Customer service Information and communication, and Billing and payment. Kaiser Foundation Health Plan garnered the top spot for the fifth year in-a-row. By feature, Kaiser achieved 5 “Power Circles” for all factors except for cost and provider choice,
When Will Self-Service Come to Health Care?

At least one in three people who have tried out virtual health care have done so because they use technology in all aspects of life and want to do the same with their healthcare. This data point has informed my vision for self-care and the home as our health hub, bolstered in part through the research of Accenture from which this first graphic comes. A common theme at health care meetings these days is how and when health care will meet its Amazon, Apple, or Uber moment? Lately, one of my speaking topics is the “Amazon Prime-ing” of health consumers,
Prescription Drug Costs In America Through the Patient Lens, via IQVIA, GoodRx and a New $2 Million Therapy

Americans consumed 17.6 prescriptions per person in 2018, two in three of which treated chronic conditions. Welcome to Medicine Use and Spending in the U.S. , the annual review of prescription drug supply, demand and Rx pricing dynamics from the IQVIA Institute for Human Data Science. In a call with analysts this week in which I participated, the Institute’s Executive Director Murray Aitken discussed the report which looks back at 2018 and forward to 2023 with scenarios about what the U.S. prescription drug market might look like five years from now. The report is organized into four sections: medical use
Assessing the GAO’s Report on Single-Payer Healthcare in America: Let’s Re-Imagine Workflow

Calls for universal health care, some under the banner of Medicare for All,” are growing among some policy makers and presidential candidates looking to run in 2020. As a response, the Chairman of the House Budget Committee in the U.S. Congress, Rep. John Yarmuth (D-Ky.), asked the Congressional Budget Office (CBO) to develop a report outlining definitions and concepts for a single-payer health care system in the U.S. The result of this ask is the report, Key Design Components and Considerations for Establishing a Single-Payer Health Care System, published on 1st May by the CBO. The report provides
Will Health Consumers Morph Into Health Citizens? HealthConsuming Explains, Part 5

The last chapter (8) of HealthConsuming considers whether Americans can become “health citizens.” “Citizens” in this sense goes back to the Ancient Greeks: I return to Hippocrates, whose name is, of course, the root of The Hippocratic Oath that physicians take. Greece was the birthplace of Democracy with a capital “D.” Hippocrates’ book The Corpus is thought to be one of the first medical textbooks. The text covered social, physical, and nutritional influences, and the concept of “place” for health and well-being. Here, the discussion detailed the roles of air and water for health. The Hippocratic texts also coached doctors to
Health/Care Everywhere – Re-Imagining Healthcare at ATA 2019

“ATA” is the new three-letter acronym for the American Telemedicine Association, meeting today through Tuesday at the Convention Center in New Orleans. Ann Mond Johnson assumed the helm of CEO of ATA in 2018, and she’s issued a call-to-action across the health/care ecosystem for a delivery system upgrade. Her interview here in HealthLeaders speaks to her vision, recognizing, “It’s just stunning that there’s such a lag between what is possible in telehealth and what is actually happening.” I’m so keen on telehealth, I’m personally participating in three sessions at #ATA19. On Monday 15th April (US Tax Day, which is relevant
What $285,000 Can Buy You in America: Medical Costs for Retirees in 2019
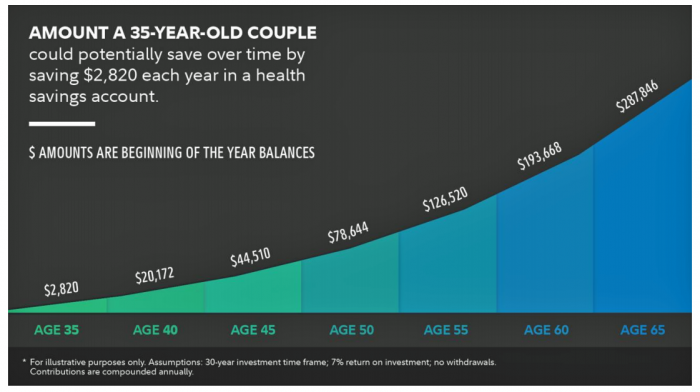
The average 65-year old couple retiring in 2019 will need to have a cash nest-egg of $285,000 to cover health care and medical expenses through retirement years, Fidelity Investments calculated. Fidelity estimates the average retiree will allocate 15% of their annual spending in retirement on medical costs. As if that top-line number isn’t enough to sober one up, there are two more caveats: (1) the $285K figure doesn’t include long-term care, dental services and over-the-counter medicines; and, (2) it’s an after-tax number. So depending on your tax bracket, you have to earn a whole lot more to net the $285,000
National Health Spending Will Reach Nearly 20% of U.S. GDP By 2027
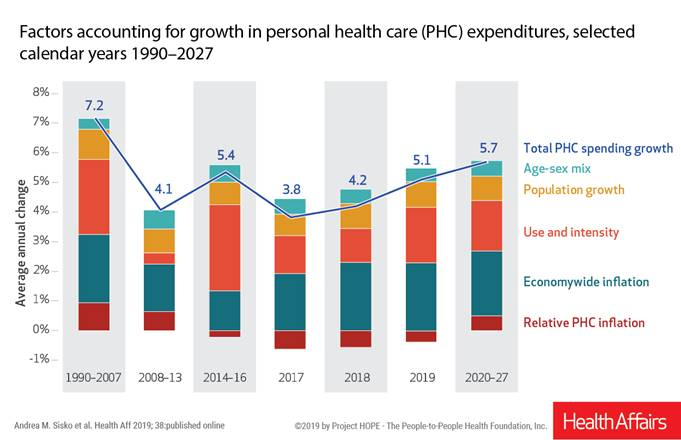
National health spending in the U.S. is expected to grow by 5.7% every year from 2020 to 2027, the actuaries at the Centers for Medicare and Medicaid Services forecast in their report, National Health Expenditure Projections, 2018-2927: Economic And Demographic Trends Drive Spending And Enrollment Growth, published yesterday by Health Affairs. For context, note that general price inflation in the U.S. was 1.6% for the 12 months ending January 2019 according to the U.S. Bureau of Labor Statistics. This growth rate for health care costs exceeds every period measured since the high of 7.2% recorded in 1990-2007. The bar chart illustrates the
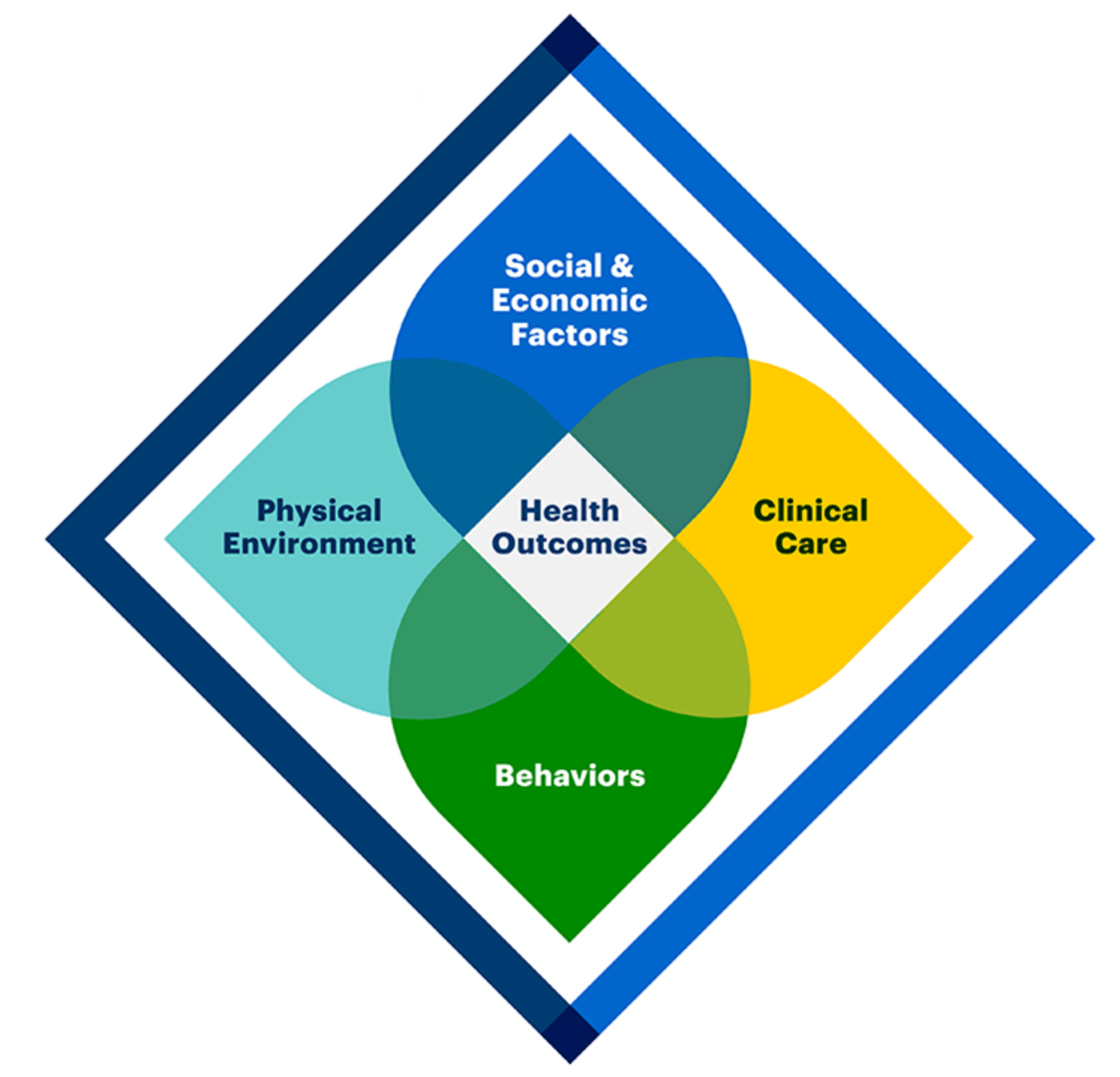
Health Is Social – The Social Determinants of Health at HIMSS19
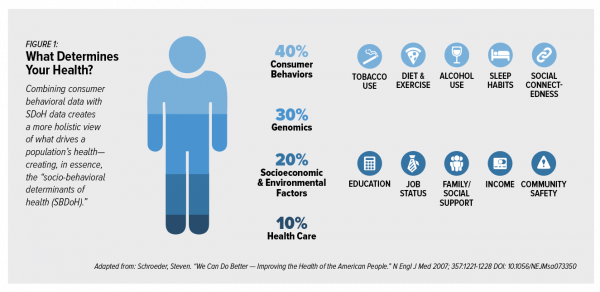
In the health care world, it is now commonly accepted that genes contribute less than half of the influence on peoples’ health status. Other issues play starring roles in overall well-being, including environmental factors, health care services, and social determinants of health (SDOH). These inputs include education, personal economics (like job security and financial stability), physical built environments (think: transportation access, safe and healthy housing), food and nutrition, and access to health care. At HIMSS17, I gave a talk in a big room about how technology can scale SDOH; we had standing room only, which is not a brag —
Heart Health at #CES2019 – Food and Tech as Medicine

Self-care is the new health care as patients, now consumers at greater financial risk for medical spending, are learning. At #CES2019, I’m on the lookout for digital technologies that can help people adopt and sustain healthy behaviors that can help consumers save money on medical care and enhance quality of life-years. This week’s heart-and-food tech announcements at #CES2019 coincide with an FDA recall on a popular drug prescribed to treat hypertension (high blood pressure). Using food and tech as medicine can help people avoid going on medications like statins and others for heart health. An important example of this self-care
Costs, Consumerism, Cyber and Care, Everywhere – The 2019 Health Populi TrendCast

Today is Boxing Day and St. Stephens Day for people who celebrate Christmas, so I share this post as a holiday gift with well-wishes for you and those you love. The tea leaves have been brewing here at THINK-Health as we prepared our 2019 forecast at the convergence of consumers, health, and technology. Here’s our trend-weaving of 4 C’s for 2019: costs, consumerism, cyber and care, everywhere… Health care costs will continue to be a mainstream pocketbook issue for patients and caregivers, with consequences for payors, suppliers and ultimately, policymakers. Legislators inside the DC Beltway will be challenged by the
Healthcare Is Local: Channeling Tip O’Neill in the 2018 Midterm Election Results

As Tip O’Neill’s mantra goes, “All politics is local.” In the U.S. 2018 midterm elections, healthcare voting seems to have translated as a local issue, falling into O’Neill’s axiom. In this election, healthcare was the most important voting issue for consumers, PwC found, ranking above the economy, national security, and education. On this morning after 2018 midterm election results are (mostly) out, it looks like healthcare was a local and state issue for U.S. 2018 midterm voters. The Democrats flipped more than 23 seats in the U.S. House of Representatives to gain control of that chamber. The Senate is up
Healthcare and the F-Word: Health Politics Rank High on November 6, 2018

“Let’s get this thing f-ing done,” Martha McSally passionately asserted on May 4, 2017. Paul Ryan said, on the floor of the U.S. House of Representatives without cursing, “A lot of us have waited seven years to cast this vote.” McSally, who represents Tucson, Arizona, in the U.S. Congress, is running to replace retiring Senator Jeff Flake. McSally was one of the 217 Republicans in the House who voted to repeal the Affordable Care Act, subsequently celebrating a victory in the Rose Garden of the White House with jubilant peers. The final vote was 217-213. Here’s the final roll call
Technology, Aging and Obesity Drive Healthcare Spending, BEA Finds

The U.S. Department of Commerce Bureau of Economic Analysis (BEA) released, for the first time, data that quantifies Americans’ spending to treat 261 medical conditions, from “A” diseases like acute myocardial infarction, acute renal failure, ADHD, allergic reactions, anxiety disorders, appendicitis and asthma, to dozens of other conditions from the rest of the alphabet. High Spending Growth Rates For Key Diseases In 2000-14 Were Driven By Technology And Demographic Factors, a June 2018 Health Affairs article, analyzed this data. This granular information comes from the BEA’s satellite account, using data from the Medical Expenditure Panel Survey which nationally examines expenditures by disease;
How Walmart Could Bolster Healthcare in the Community

Walmart has been a health/care destination for many years. The company that defined Big Box stores in their infancy grew in healthcare, health and wellness over the past two decades, pioneering the $4 generic prescription back in 2006. Today, that low-cost generic Rx is ubiquitous in the retail pharmacy. A decade later, can Walmart re-imagine primary care the way the company did low-cost medicines? Walmart is enhancing about 500 of 3500 stores, and health will be part of the interior redecorating. Walmart has had ambitious plans in healthcare since those $4 Rx’s were introduced. Here’s a New York Times article from





 I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for